Introduction
Episiotomy, the surgical enlargement of the posterior aspect of the vagina by an incision to the perineum during the last part of the second stage of labor, has been a common obstetric procedure intended to facilitate vaginal delivery and prevent severe perineal tears. However, its routine use has been reevaluated over time, leading to a more selective approach in modern obstetric practice.
Definition and Rationale
The primary purpose of an episiotomy is to widen the birth outlet to facilitate the delivery of the baby. This procedure was historically performed routinely to prevent severe perineal trauma, but current evidence and guidelines recommend a more judicious, case-by-case application.
Selective Use Only
Current recommendations strongly advise against the routine performance of episiotomy , citing increased risks of severe perineal trauma and wound complications compared to restricted use. The decision to perform an episiotomy is now made selectively, based on specific clinical scenarios rather than as a standard practice for all vaginal deliveries.
Potential Indications
While there are no absolute indications for an episiotomy, certain situations may warrant its consideration, including:
- The need for expedited vaginal delivery.
- Operative vaginal delivery (e.g., forceps or vacuum-assisted delivery).
- Shoulder dystocia.
The decision to perform an episiotomy is heavily reliant on the delivering clinician's judgment, influenced by the clinical scenario at the time of delivery.
Technique
Proper technique and patient preparation are crucial:
- Informed consent is obtained.
- Adequate anesthesia is administered.
- The fetal scalp is protected prior to making the incision.
- The specific type and rationale for the episiotomy are documented in the delivery record.
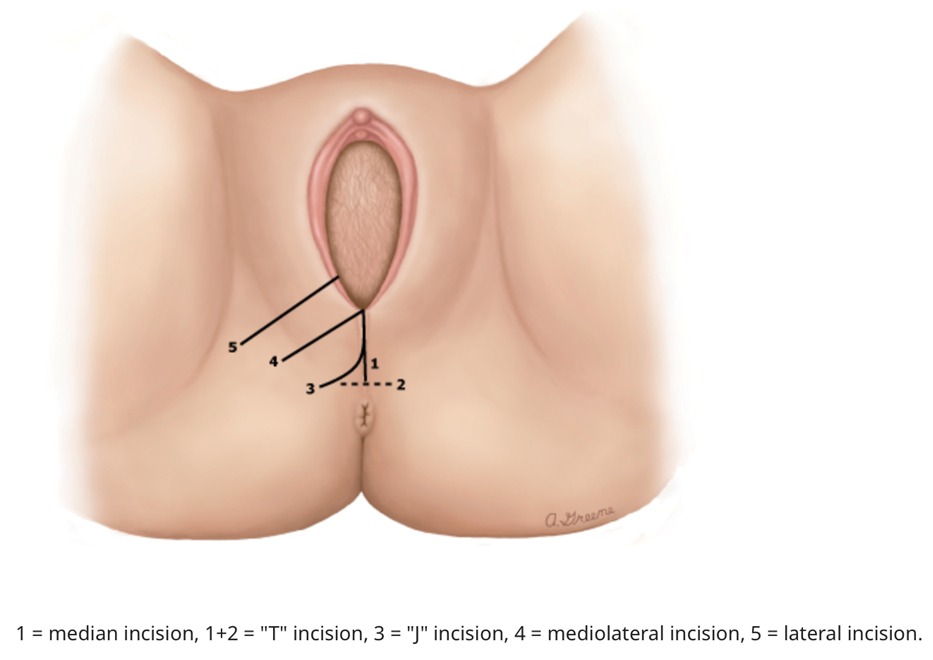
Types of Episiotomy:
- Median (Midline) Episiotomy
Popular in the United States, this technique involves an incision starting within 3 mm of the posterior fourchette's midline, extending downwards between 0 and 25 degrees of the sagittal plane. It's valued for its simplicity and ease of repair. - Mediolateral Episiotomy
Favored in Europe, the incision begins similarly near the midline but is directed laterally at a minimum 60-degree angle towards the ischial tuberosity, aiming to mitigate the risk of anal sphincter damage. - T Episiotomy
This variant expands the vaginal opening via an inverted T-shaped incision, offering more space than a median episiotomy alone. - Lateral Episiotomy
It involves an off-center start, blending mediolateral angulation with a position adjustment to reduce risks associated with typical mediolateral episiotomies during crowning. - Anterior Episiotomy (Deinfibulation)
Specifically indicated for women with prior female circumcision, it involves incising the fused labia minora to reveal the urethral meatus, preserving clitoral remnants. - J Incision
A less common option, resembling the letter "J," starts at the fourchette and extends caudally, then laterally, sparing the transverse perineal muscle when possible.
Choice of Procedure
When an episiotomy is deemed necessary, a mediolateral or lateral episiotomy is preferred to a median (midline) episiotomy, as the former options are associated with a lower risk of anal sphincter laceration.
Complications
- Infection
- Hematoma
- Third and fourth degree extension
- Cellulitis
- Dehiscence
- Abscess
- Dyspareunia
- Altered sexual function
- Perineal pain
- Incontinence: urinary, fecal, flatus
- Rectovaginal fistula
- Impaired pudendal nerve conduction
- Necrotizing fasciitis
Conclusion
The shift from routine to selective episiotomy use reflects an evolving understanding of the procedure's benefits and risks. By carefully considering the indications and employing the correct technique, clinicians can optimize maternal outcomes, reducing the incidence of complications associated with episiotomy.
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.