شرح المدرسين
Summary
Approach to Screening and Testing
Prenatal care includes crucial decisions regarding genetic carrier screening and tests for chromosomal abnormalities. It is recommended to offer these screenings to all patients, ideally at the initial prenatal visit, to ensure timely identification and management of potential risks to the fetus.
Counseling Prior to Testing
Before conducting any prenatal genetic tests, it is imperative to provide comprehensive counseling to expectant parents. This counseling should cover the spectrum of available tests, including their benefits, limitations, and the implications of test results. This process ensures that parents make informed decisions that align with their values and preferences.
Options for Screening and Testing
- Genetic Carrier Screening:
- Genetic carrier screening is a critical component of prenatal care, aimed at identifying individuals who carry a gene for a genetic disorder that could be passed on to their offspring. This screening is recommended for all patients, providing valuable information for prospective parents regarding their risk of having a child with a genetic condition.
- Cystic Fibrosis (CF): A genetic disorder affecting the lungs, pancreas, and other organs, leading to severe respiratory and digestive problems. Screening for CF is crucial because it is one of the most common genetic disorders in the Caucasian population.
- Spinal Muscular Atrophy (SMA): A genetic disorder characterized by loss of motor neurons, leading to muscle wasting and weakness. SMA screening is vital due to its potential severity and the availability of treatment options that can significantly improve outcomes if started early.
- Hemoglobinopathies: Genetic disorders affecting the structure or production of the hemoglobin molecule in red blood cells. Common hemoglobinopathies include sickle cell disease and thalassemias. Screening for carriers of hemoglobinopathies is typically done using red blood cell indices as a minimum screening method. However, for a more comprehensive analysis, high-performance liquid chromatography (HPLC) or capillary electrophoresis is recommended. These methods provide a detailed profile of hemoglobin variants, offering more accurate identification of carriers and the specific type of hemoglobinopathy.
- Genetic carrier screening is a critical component of prenatal care, aimed at identifying individuals who carry a gene for a genetic disorder that could be passed on to their offspring. This screening is recommended for all patients, providing valuable information for prospective parents regarding their risk of having a child with a genetic condition.
- Testing for Chromosomal Abnormalities:
- Noninvasive Aneuploidy Screening:
- This category includes screening through maternal serum biomarkers and ultrasound markers, or the more recent cell-free fetal DNA testing. These noninvasive tests estimate the risk of chromosomal conditions such as Down syndrome (Trisomy 21), Edwards syndrome (Trisomy 18), and Patau syndrome (Trisomy 13) without posing risks to the fetus.
- Invasive Genetic Testing:
- For a definitive diagnosis, invasive tests like amniocentesis or chorionic villus sampling (CVS) are available. While offering precise information about the fetus's chromosomes, these procedures carry a small risk of miscarriage and are usually recommended when there is a high risk or indication of genetic abnormalities.
- Noninvasive Aneuploidy Screening:
Follow-Up and Counseling
Depending on the outcomes of these tests, additional genetic counseling and/or further testing may be offered. Follow-up counseling is crucial for interpreting test results, understanding the risks and benefits of further testing, and making informed decisions about the pregnancy.
One-step Screening Tests for Fetal Chromosomal Abnormalities
Screening tests for fetal chromosomal abnormalities are essential components of prenatal care, enabling early detection of potential genetic conditions. Below is an overview of the main screening tests available, their timing, components, and how their results are interpreted.
Cell-free Fetal DNA Testing (cffDNA)
- Timing: From 9–10 weeks' gestation onwards
- Components: Analysis of fetal DNA fragments isolated from a maternal blood specimen.
- Interpretation: This test is the most sensitive and specific screening method for common fetal chromosomal aneuploidies, such as trisomy 21 (Down syndrome), trisomy 18 (Edwards syndrome), and trisomy 13 (Patau syndrome). It can also identify the sex of the fetus.
Sonographic Nuchal Translucency (NT Screen)
- Timing: 10–14 weeks' gestation
- Components: A transabdominal ultrasound measures the fluid at the back of the fetal neck.
- Interpretation: A positive screen is defined as NT ≥ 3 mm or greater than the 99th percentile for the crown-rump length measurement. Increased NT is linked with an increased risk of aneuploidy and fetal cardiac abnormalities.
First-Trimester Combined Screening
- Timing: 10–14 weeks' gestation
- Components: This screening combines the NT screen with maternal serum measurements of β-HCG, PAPP-A, and optionally AFP.
- Interpretation: The risk of aneuploidy is assessed based on maternal age, laboratory results, and NT measurement. This approach offers a comprehensive risk evaluation for chromosomal abnormalities.
Overview of first-trimester combined screening test results Condition HCG PAPP-A Nuchal translucency Trisomy 21 ↑ ↓ ↑ Trisomy 18 ↓ ↓ ↑↑ Trisomy 13 ↓ ↓ ↑
Triple Screen Test and Quad Screen Test
- Timing: 15–22 weeks' gestation
- Components: These tests measure β-HCG, AFP, unconjugated estriol, and, in the Quad test only, inhibin A.
- Interpretation: Risk evaluation is based on maternal age and laboratory results. These tests also assess the risk of neural tube defects, providing a broader spectrum of prenatal screening.
Overview of quad and triple screening test results Condition HCG AFP Estriol Inhibin A (quad test only) Trisomy 21 ↑ ↓ ↓ ↑ Trisomy 18 ↓ ↓↓ ↓↓ ↔︎ or ↓ Neural tube defects ↔︎ ↑ ↔︎ Abdominal wall defects
Multi-Step Screening Tests for Fetal Chromosomal Abnormalities
Multi-step screening tests for fetal chromosomal abnormalities offer a phased approach to prenatal screening, combining results from different stages of pregnancy to assess the risk of chromosomal abnormalities. Below is an overview of the integrated screen and sequential integrated screening, detailing their timing, components, and interpretation.
Integrated Screen
- First Specimen (10–13 weeks' gestation):
- Components: NT screen, PAPP-A.
- Second Specimen (15–22 weeks' gestation):
- Components: Quad screen test (measuring β-HCG, AFP, unconjugated estriol, and inhibin A).
- Interpretation: The risk of aneuploidy is assessed based on the combined results from the first and second trimesters. Results are provided only after the second-trimester testing is completed, offering a comprehensive risk analysis.
Sequential Integrated Screening
- First Specimen (10–13 weeks' gestation):
- Components: NT screen, PAPP-A, β-HCG, and optionally AFP.
- Interpretation: The risk of aneuploidy is calculated based on the results of the first-trimester testing. Recommendations for follow-up testing are made accordingly, allowing for earlier decision-making.
- Second Specimen (15–22 weeks' gestation):
- Components: Quad screen test.
- Further Steps: Depending on the results of the first-trimester testing, patients may choose to proceed with the second specimen testing for a more detailed risk assessment or may opt for diagnostic testing based on initial risk estimations.
Invasive Prenatal Diagnostic Testing
Invasive prenatal diagnostic testing is a critical aspect of prenatal care, providing definitive information about genetic and chromosomal abnormalities in the fetus. These tests are performed through procedures like chorionic villus sampling (CVS), amniocentesis, and, in select cases, cordocentesis. Each of these methods has specific timings, procedures, indications, and potential complications associated with them.
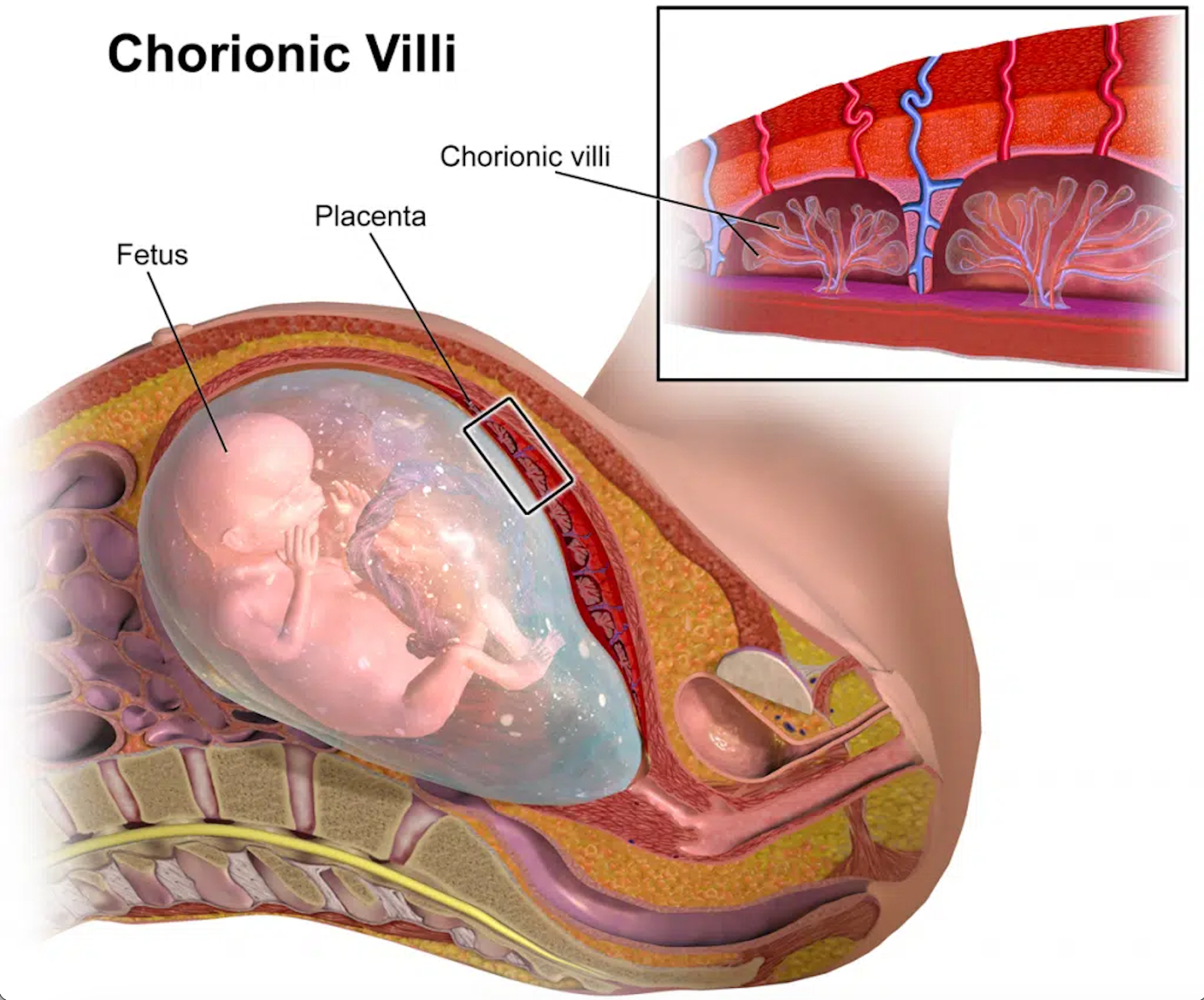
Chorionic Villus Sampling (CVS)
- Timing: 10–13 weeks' gestation.
- Procedure: Can be performed transcervically or transabdominally, involving the needle aspiration of a small amount of placental tissue under ultrasound guidance.
- Indications: Primarily used for early evaluation of fetal genetic abnormalities. Indications include follow-up of abnormal noninvasive genetic screening results or fetal structural abnormalities observed on ultrasound.
- Complications: Includes a miscarriage risk of approximately 0.2%, limb defects, vaginal bleeding, and other less common complications.
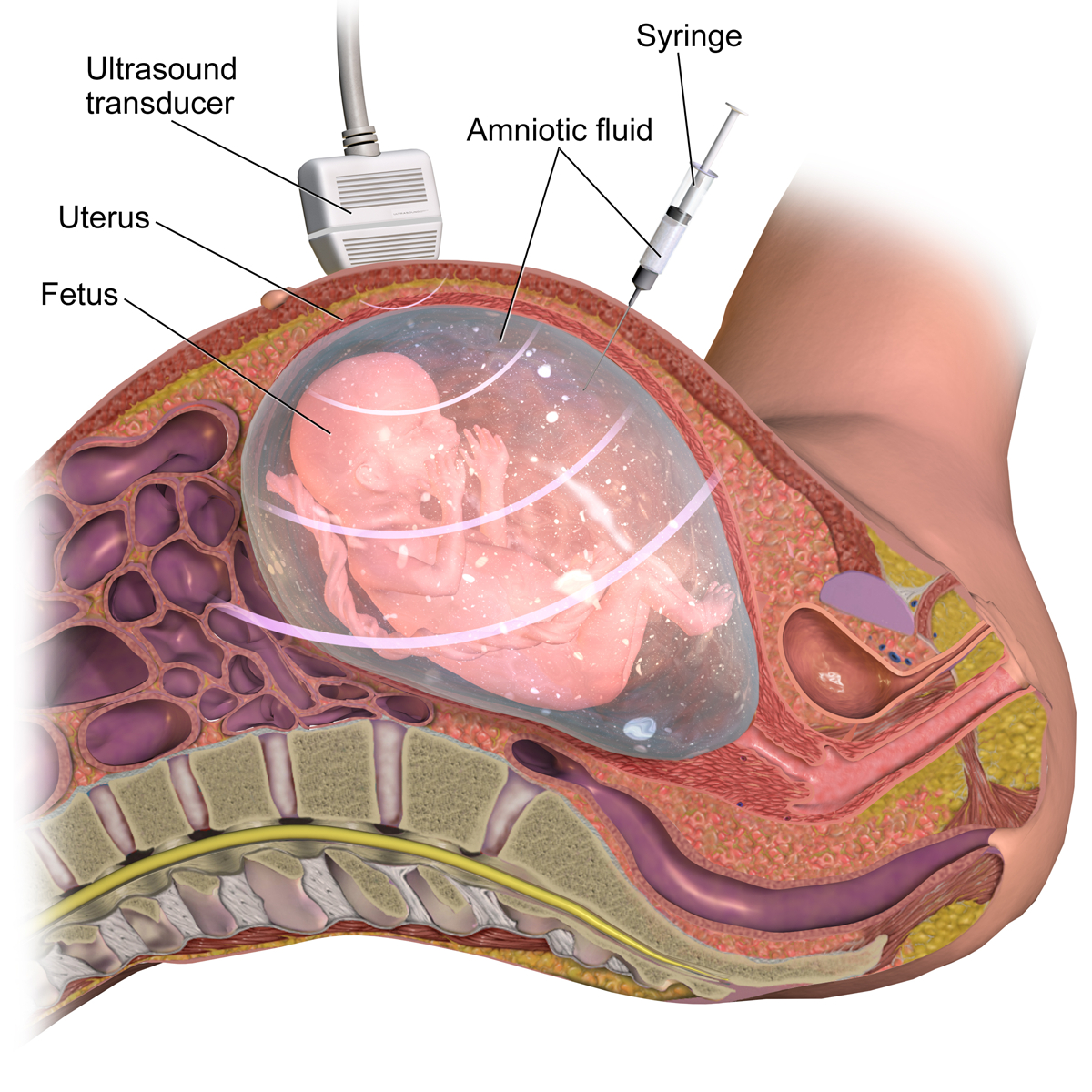
Amniocentesis
- Timing: From 15 weeks' gestation onwards, most commonly between 15-20 weeks.
- Procedure: Involves the transabdominal needle aspiration of amniotic fluid under ultrasound guidance.
- Indications: Beyond the evaluation for fetal genetic abnormalities, amniocentesis is used for fetal blood typing in Rh alloimmunization cases, diagnosis of certain suspected infections, and therapeutic amnioreduction in cases of polyhydramnios.
- Complications: The risk of miscarriage ranges from 0.1-0.3%, with potential for vaginal bleeding, leaking of amniotic fluid, premature rupture of membranes, and infection.
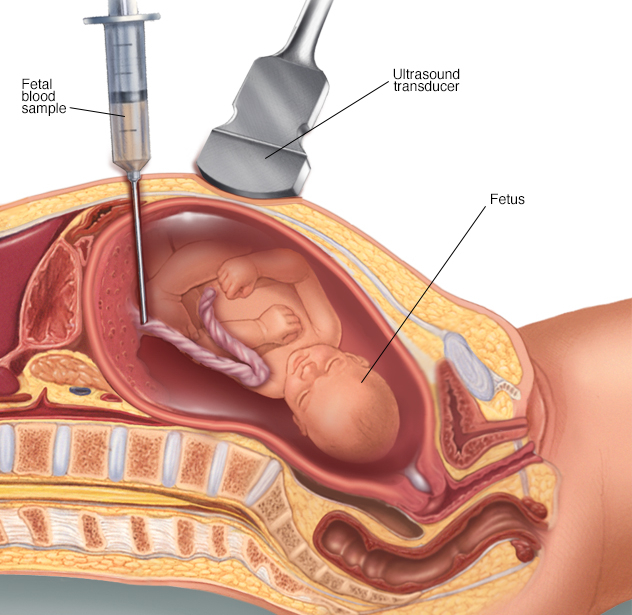
Cordocentesis
- Timing: After 18 weeks' gestation.
- Procedure: Involves the transabdominal insertion of a needle into the umbilical cord to sample fetal blood from the umbilical vein.
- Indications: Though rarely used for genetic abnormalities evaluation, it's primarily for fetal hemoglobin testing to assess the severity of fetal anemia.
- Complications: Includes a higher miscarriage risk of 1–2%, umbilical cord bleeding, and fetal heart rate abnormalities.
Chromosomal Testing of Specimens
The specimens collected through these diagnostic procedures can undergo various chromosomal testing such as DNA microarray, karyotyping, fluorescence in situ hybridization (FISH), and direct detection of specific DNA mutations. These tests provide comprehensive insights into the genetic health of the fetus, enabling informed decision-making for expectant parents and healthcare providers.
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.