شرح المدرسين
Introduction
Embarking on prenatal care marks the commencement of a journey towards a healthy pregnancy. The initial prenatal visit and the first trimester follow-up are critical for early identification of potential risks, developing a comprehensive care plan, and building a meaningful connection between healthcare providers and the expectant mother.
Components of the Initial Prenatal Visit
This essential visit is designed to evaluate thoroughly the health and identify any risks to both the mother and fetus. It generally includes:
History Taking
- Medical and Obstetric History: Expectant mothers are asked to provide detailed information about their medical, obstetric, psychosocial, and family history. This includes any previous pregnancies, miscarriages, preterm deliveries, or experiences with preeclampsia.
- Family History: Information on both maternal and paternal family histories is collected to identify any medical conditions, genetic abnormalities, or patterns of poor obstetrical outcomes.
Physical Examination
- Complete Physical Examination: Includes measuring height and weight, screening for hypertensive pregnancy disorders, and performing breast and pelvic examinations.
- Fetal heart tones are auscultated after 10 weeks of gestation.
Ultrasound Examination
- Indications for First-trimester ultrasound
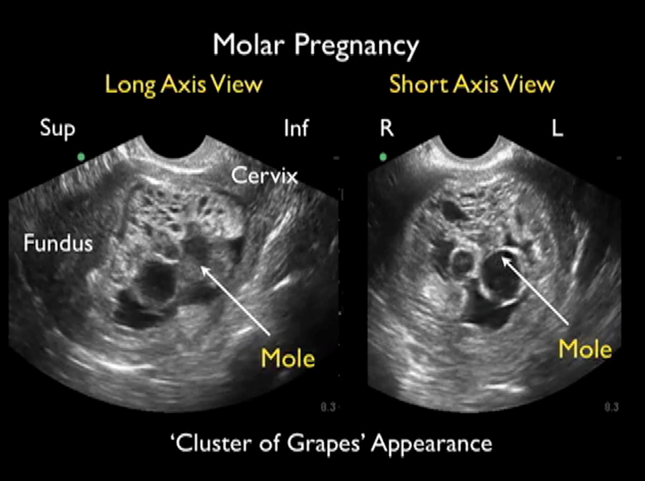
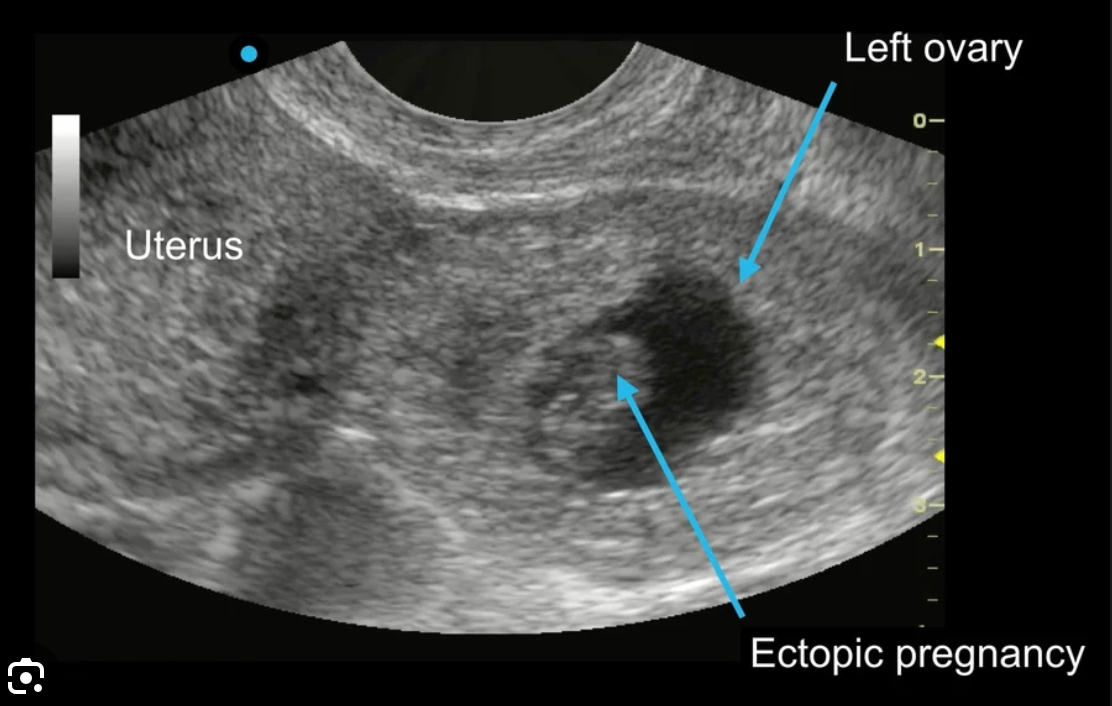
- Confirmation of pregnancy and its location, specifically to exclude ectopic pregnancy and gestational trophoblastic disease.
- Determination of the estimated date of delivery (EDD)
Gestational Age: The first trimester ultrasound is crucial for determining gestational age, especially in pregnancies with uncertain LMP dates, irregular menstrual cycles, or those conceived while on hormonal contraception. It provides a more accurate estimation than menstrual dates, influencing management decisions such as the timing for labor induction and cesarean births.
- Resolving Discrepancies: If there's a discrepancy between the LMP and ultrasound estimates of gestational age, the estimated due date (EDD) is adjusted based on ultrasound findings if:
- The discrepancy exceeds 5 days in gestations under 9 weeks.
- The discrepancy exceeds 7 days in gestations between 9 and 13 weeks.
- Resolving Discrepancies: If there's a discrepancy between the LMP and ultrasound estimates of gestational age, the estimated due date (EDD) is adjusted based on ultrasound findings if:
- Evaluation for the presence of multiple gestations
- Early detection of multiple gestations and the determination of chorionicity and amnionicity are crucial for guiding management strategies.
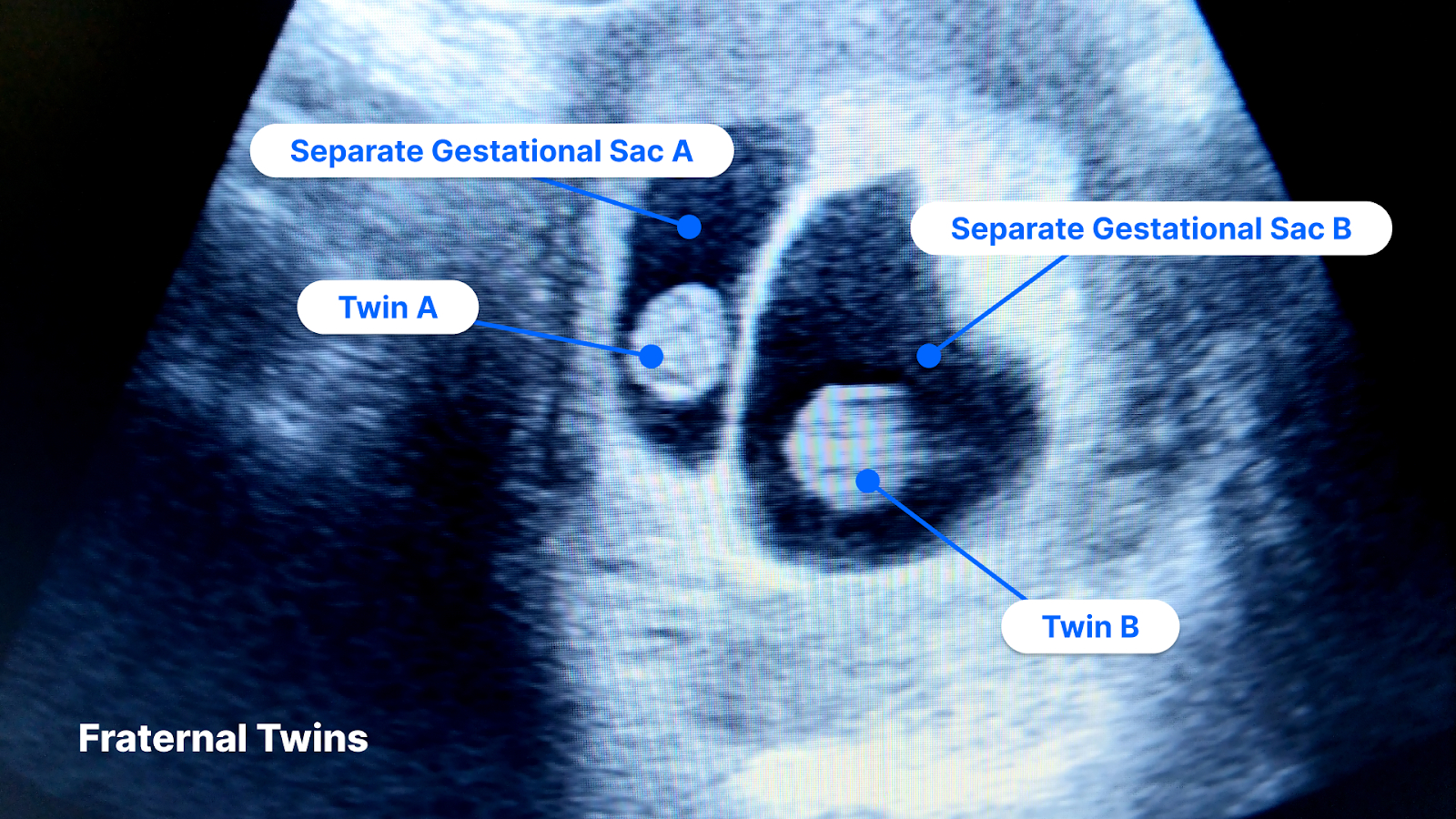
- Early detection of multiple gestations and the determination of chorionicity and amnionicity are crucial for guiding management strategies.
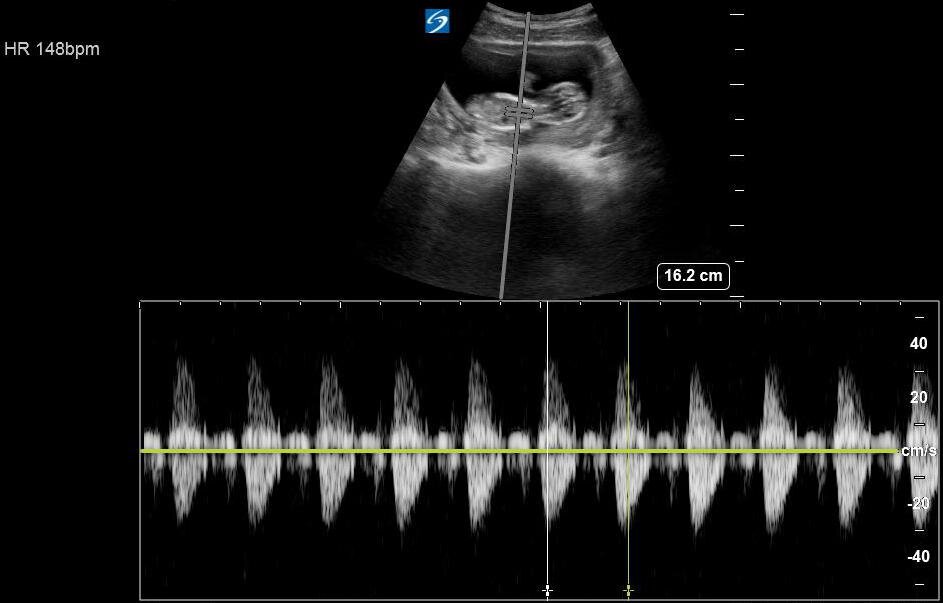
- Assessment of fetal cardiac activity.
- Evaluation of maternal symptoms such as pelvic pain or vaginal bleeding, or abnormalities found on examination like masses or structural uterine anomalies.
- Screening for fetal anomalies, for example, anencephaly.
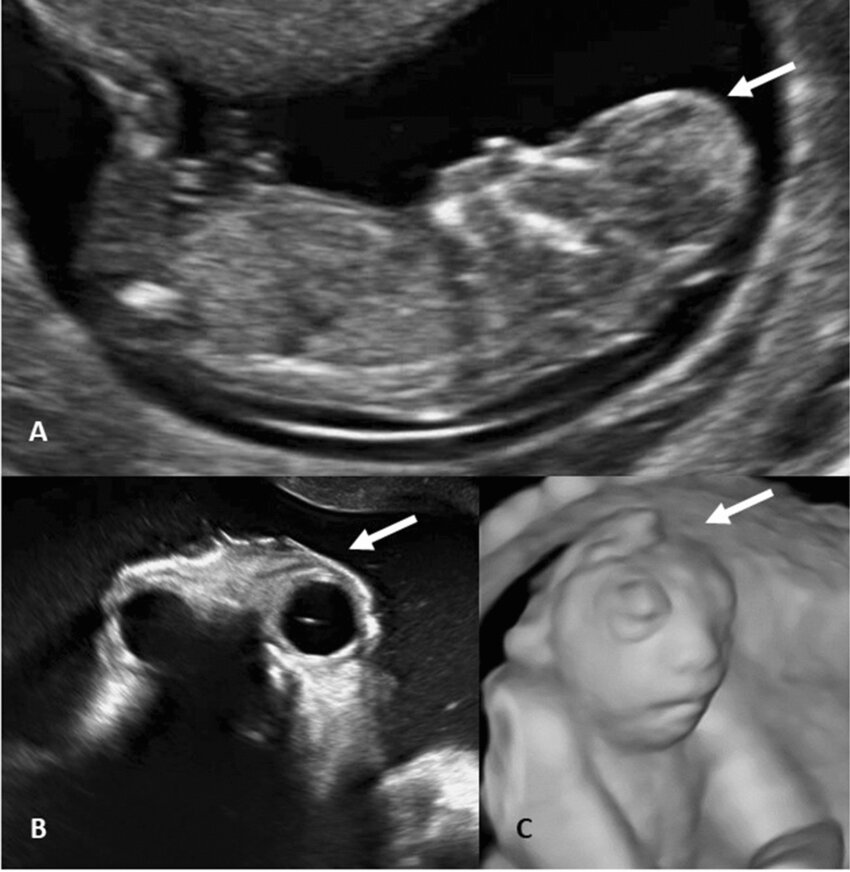
- Measurement of nuchal translucency as part of aneuploidy screening.

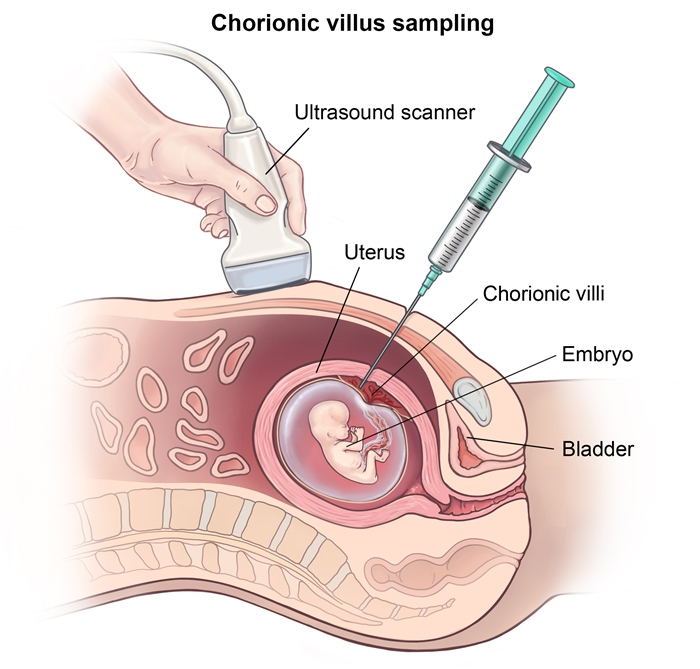
- Providing imaging guidance during invasive procedures, such as chorionic villus sampling (CVS).
- Confirmation of pregnancy and its location, specifically to exclude ectopic pregnancy and gestational trophoblastic disease.
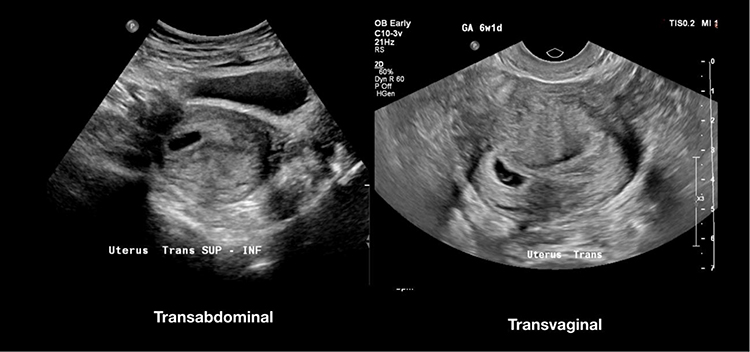
- Modalities for Ultrasound in Pregnancy
- Transvaginal ultrasound: Provides detailed images of the uterus, ovaries, and early pregnancy structures.
- Transabdominal ultrasound: Used for broader overviews of the abdominal cavity and later in pregnancy to assess fetal growth, placental location, and amniotic fluid volume.
Discussion of Screening and Diagnostic Testing
Understanding gestational age is essential for timely and appropriate screening and diagnostic testing for genetic and anatomic abnormalities. This empowers expectant parents with informed choices throughout the pregnancy.
Laboratory Tests and Screening for Medical Comorbidities
Recommended Initial Prenatal Screening Tests for All Patients
- Complete Blood Count (CBC): Screens for anemia and thrombocytopenia.
- Anemia Management: Consider iron deficiency, vitamin B12, or folate deficiency; repeat CBC at 24–28 weeks' gestation.
- Thrombocytopenia Management: Explore differential diagnoses; consider gestational thrombocytopenia if no other cause is identified.
- Blood Typing (ABO and Rhesus) and RBC Antibody Screening: Prevents hemolytic disease of the newborn.
- Management for Rh-negative Individuals Without Anti-D Antibodies: Administer anti-D immunoglobulins for any potentially sensitizing events; repeat Rh antibody testing at 24–28 weeks.
- Urine Dipstick: Screens for proteinuria.
- Management: Confirm with spot urine protein-creatinine ratio or 24-hour urine collection; consider nephrology consultation for proteinuria before 20 weeks' gestation.
- Urine Culture: Screens for asymptomatic bacteriuria.
- Management: Treat according to guidelines; consider repeat culture as test of cure.
- Screening for STIs and Bloodborne Pathogens (HIV, HBV, HCV, Syphilis):
- Management: Follow specific guidelines for confirmed infections; consider specialist referral for positive HCV antibody.
Prenatal Screening Studies for Patients with Select Indications
- Rubella and Varicella Antibody Testing: For patients without evidence of immunity.
- Management: Offer postpartum vaccination for non-immune patients; repeat testing if infection suspected during pregnancy.
- Thyroid-Stimulating Hormone (TSH): For patients at increased risk of thyroid disease.
- Management: Adjust based on trimester-specific TSH reference ranges; further assess with total or free T4 and total T3 as needed.
- Prenatal Chlamydia and Gonorrhea Screening (using NAAT): Especially in patients with STI risk factors.
- Management: Treat according to current guidelines; ensure appropriate follow-up and repeat testing.
- Pap Smear and/or HPV DNA Testing: For patients due for cervical cancer screening.
- Management: Consult OB/GYN specialist for abnormal results; follow guidelines for screening during pregnancy.
- Screening Tests for Latent Tuberculosis (TB): For patients with TB risk factors.
- Management: Follow guidelines for TB management in pregnant individuals.
- Hyperglycemia Testing: For patients with risk factors for Type 2 Diabetes Mellitus (T2DM).
- Management: Repeat screening at 24–28 weeks' gestation if initial screen is negative; manage according to guidelines for gestational and pregestational diabetes mellitus for positive screens.
First Trimester Follow-up (0-13+6 Weeks)
Follow-up visits, tailored to individual maternal needs and any identified risk factors, typically occur every 4 weeks during this phase. This systematic approach ensures a comprehensive evaluation of both maternal and fetal health, laying a solid foundation for a healthy pregnancy path.
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.