Introduction
Childbirth is a complex and dynamic process that, while natural, carries potential risks for both the mother and the newborn. One of the most common complications affecting birthing individuals is perineal lacerations, tears in the perineal area caused by the significant stretching forces during labor and delivery.
Epidemiology
Perineal lacerations represent the most prevalent obstetric injury of the pelvic floor, affecting a significant number of individuals during vaginal delivery. These injuries can have lasting impacts on a woman's physical health and quality of life.
Risk Factors
Several factors increase the risk of perineal lacerations, including:
- Macrosomia: Delivering a larger-than-average baby.
- Forceps Delivery: The use of instruments to assist in the delivery.
- Nulliparity: Having no previous vaginal deliveries.
- Prolonged Second Stage of Labor: Extended pushing period.
- Occiput Posterior Delivery: Baby’s head facing the mother’s abdomen.
- Rapid Delivery of the Fetal Head in Breech Presentation.
- Head Extension Before Crowning.
- Lack of Perineal Elasticity: Due to conditions like perineal edema.
Classification
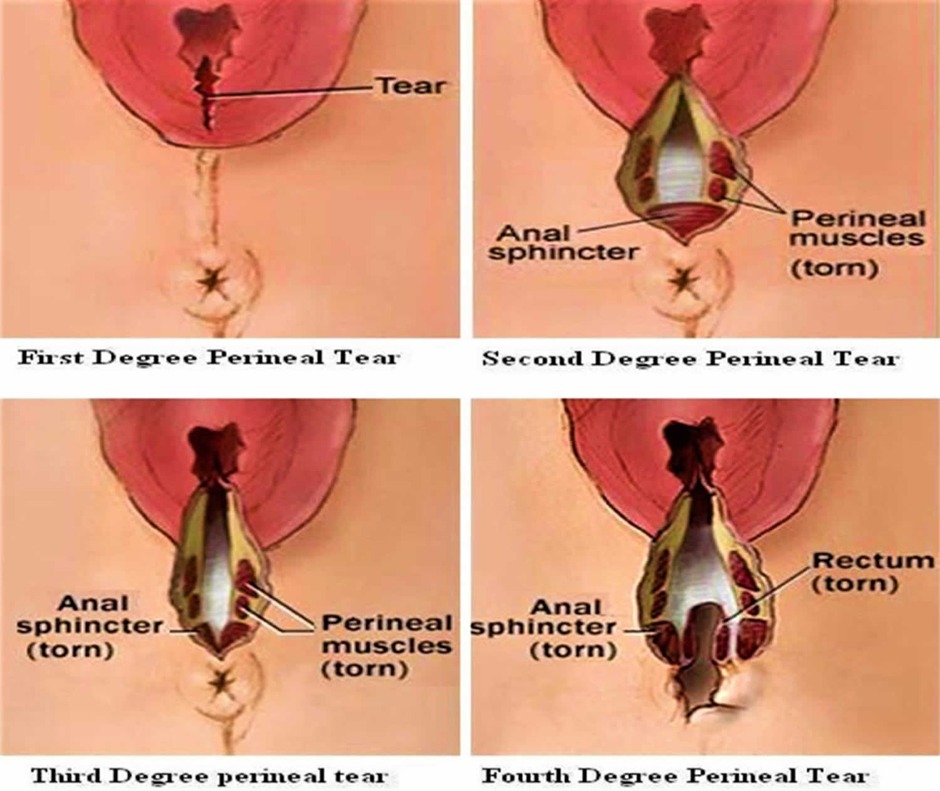
Perineal lacerations are categorized based on their severity:
- First Degree: Involves the skin and superficial structures without affecting the perineal muscles.
- Second Degree: Extends to the perineal muscles but not the anal sphincter.
- Third Degree: Involves the external anal sphincter, categorized further based on the extent of the sphincter tear.
- Fourth Degree: The most severe, involving tears through the anal sphincter and into the rectum.
Clinical Features
Symptoms of perineal lacerations can appear immediately or months post-delivery, including perineal edema, dysuria, signs of infection, and symptoms of pelvic floor dysfunction like fecal incontinence or pelvic organ prolapse.
Diagnosis
Diagnosis involves a thorough examination, including a digital rectal examination to assess sphincter tone and possible defects. Endoanal ultrasonography may be employed for a detailed evaluation of the sphincters' integrity.
Treatment
Treatment strategies vary by the degree of the laceration:
- First and Second Degree: Minor tears may require no suturing, with conservative treatments like NSAIDs or sitz baths recommended.
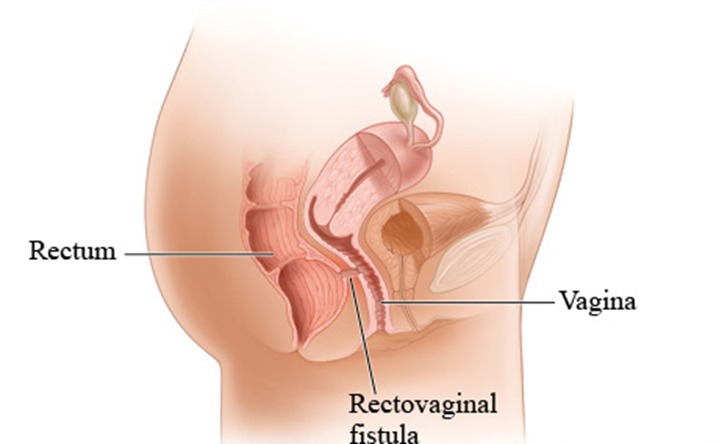
- Third and Fourth Degree: More severe tears necessitate surgical repair under regional or general anesthesia, focusing on reconstructing the anal sphincters, mucosa, and rectovaginal septum.
Complications
While first and second-degree lacerations generally heal without significant long-term issues, third and fourth-degree tears can lead to complications such as pain, dyspareunia, rectovaginal fistulae, hemorrhage, infection, and wound dehiscence.
Prevention
Preventative measures include the application of warm compresses to the perineum during delivery, aiming to enhance elasticity and reduce the risk of severe lacerations.
Conclusion
Perineal lacerations are a significant concern in obstetric care, with potential for profound impacts on postpartum recovery and long-term pelvic health. Understanding risk factors, implementing preventative measures, and ensuring prompt, appropriate treatment are key to mitigating these risks and promoting the health and well-being of mothers.
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.