Introduction
Normal human labor involves regular uterine contractions and transient interruptions of fetal oxygenation. While most fetuses withstand the rigors of labor without issue, a subset may experience distress. Intrapartum fetal heart rate (FHR) monitoring emerges as a pivotal tool in assessing fetal well-being during labor, enabling timely interventions to mitigate the risk of neurological injury or death.
Goal of Intrapartum FHR Monitoring
- To ascertain fetal oxygenation status during labor
- To facilitate the timely implementation of interventions when necessary
Candidates for Intrapartum Fetal Monitoring
- High-risk Pregnancies: Continuous electronic FHR monitoring is typically advocated to closely monitor fetal well-being.
- Low-risk Pregnancies: Options include either intermittent or continuous electronic FHR monitoring.
Exceptions to intrapartum FHR monitoring arise when potential FHR abnormalities would not alter management strategies, such as in extremely preterm labors below the viability threshold or when fetal anomalies incompatible with life are present.
Continuous vs. Intermittent Monitoring
- Continuous Electronic FHR Monitoring: real-time, continuous feedback on fetal heart rate patterns, allowing for immediate identification of abnormalities that may signify distress.
- Intermittent Auscultation: regular checks with a Doppler or fetoscope.
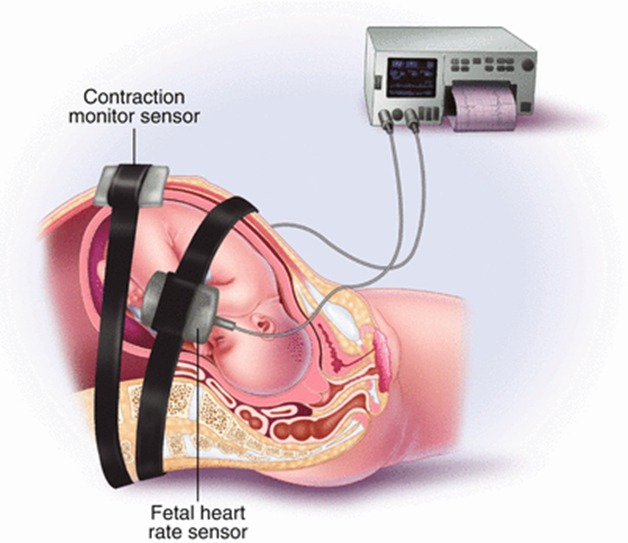
External vs. Internal Monitoring
- External FHR Monitoring: This noninvasive approach is generally as reliable as internal monitoring for most cases. It involves the use of a Doppler ultrasound device placed on the maternal abdomen to detect fetal heart motion and calculate the heart rate. Autocorrelation technology minimizes signal variation, offering a clear tracing of FHR.
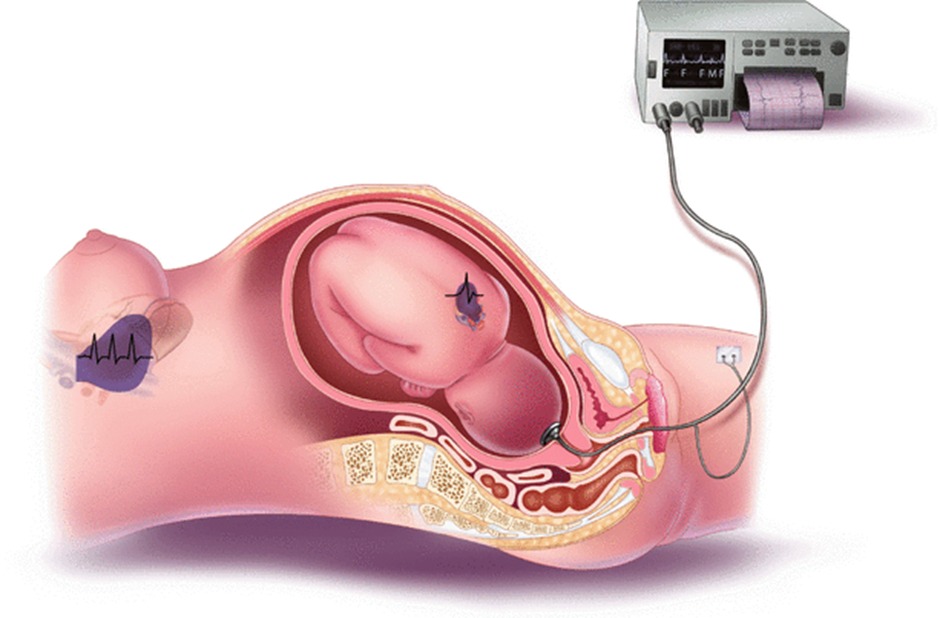
- Internal FHR Monitoring: Preferred in situations where external tracing quality is compromised (due to early gestational age, maternal habitus, or multiple gestation, among others). It involves placing a bipolar spiral electrode on the fetal scalp to obtain a more direct and clear signal of the FHR.
Frequency and Duration of Monitoring
- Initial Assessment
- Upon admission, a standard assessment of 20 to 30 minutes is recommended to identify fetuses at risk for abnormal FHR patterns.
- Continuous Monitoring
- Low-risk Pregnancies: Continuous monitoring is advised when feasible, with FHR review every 30 minutes during the first stage of labor and every 15 minutes during the second stage.
- High-risk Pregnancies: Continuous monitoring with more frequent reviews—every 15 minutes during the first stage and every 5 minutes during the second stage.
- Intermittent Auscultation
- An alternative for low-risk pregnancies, it involves listening to the FHR for ≥60 seconds and record the rate during and immediately after a uterine contraction at least every 30 minutes during the active phase of the first stage of labor and at least every 15 minutes during the second stage .
- If risk factors for fetal compromise are present, the FHR is determined, evaluated, and recorded preferably before, during, and after a uterine contraction at least every 15 minutes during the active phase of the first stage of labor and at least every 5 minutes during the second stage.
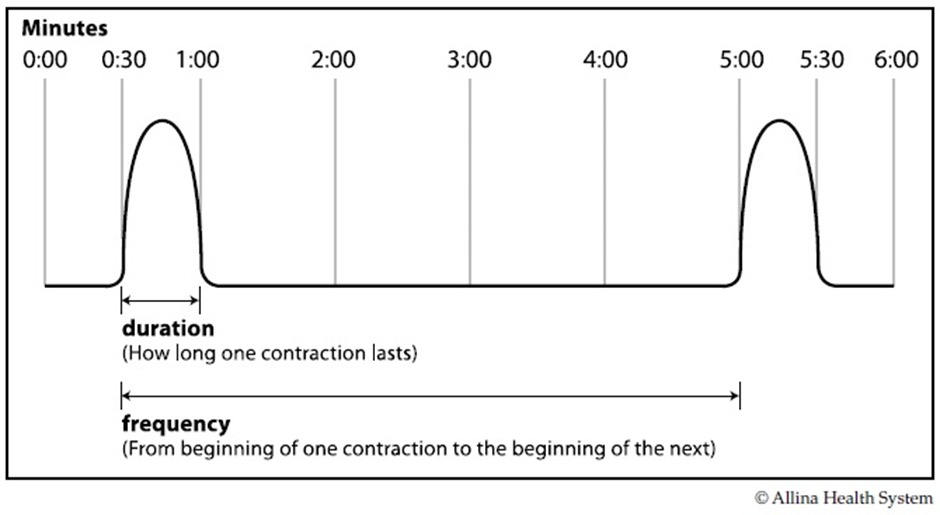
Assessment of Uterine Activity
- The interpretation of FHR patterns should be conducted alongside an assessment of uterine activity, considering factors like contraction frequency, intensity, duration, and resting tone.
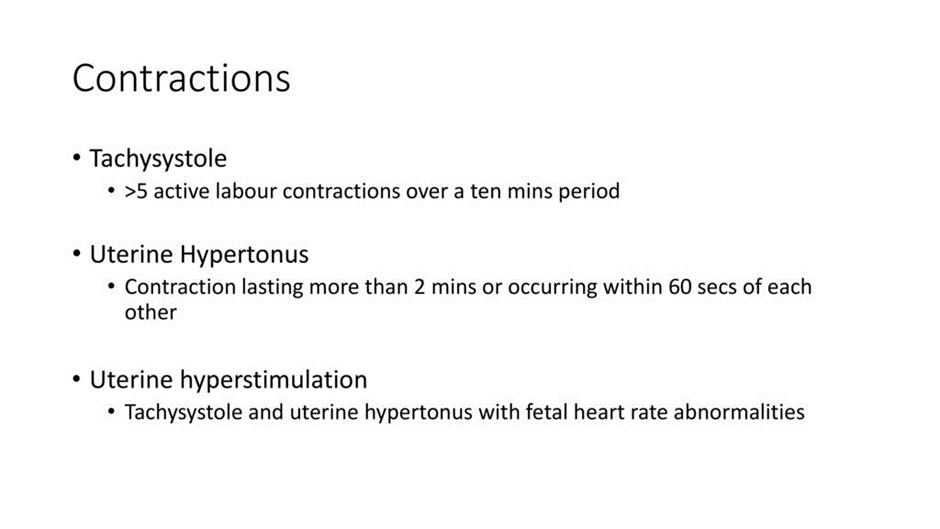
- The NICHD defines normal uterine contraction frequency as five or fewer contractions in 10 minutes, averaged over 30 minutes, with higher frequencies categorized as tachysystole.
Assessment of fetal heart
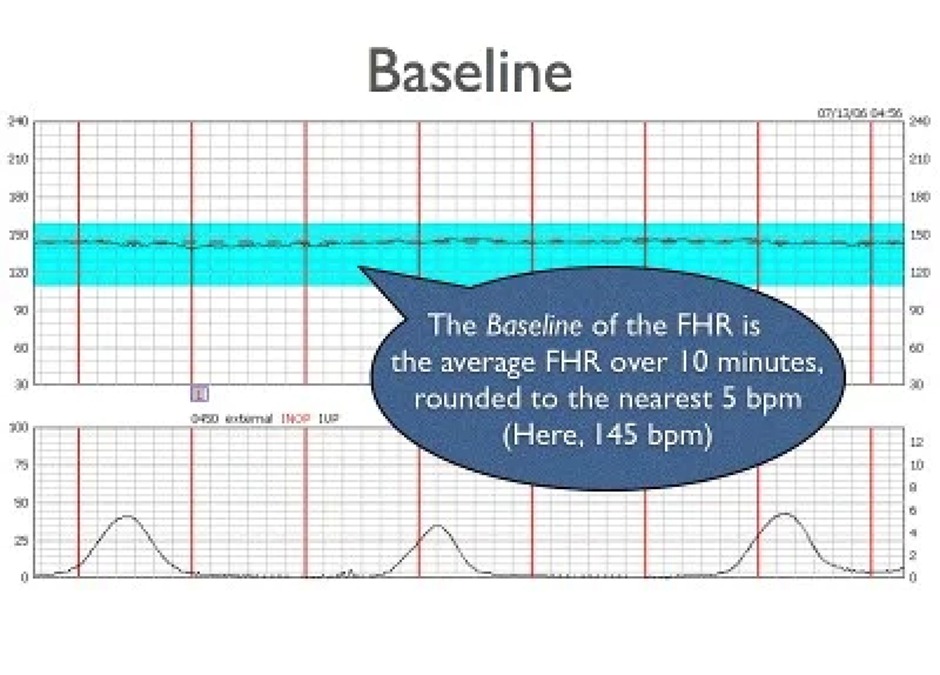
Baseline FHR
The baseline rate is the mean bpm over a 10-minute interval —- indicating a healthy fetal autonomic and cardiovascular system.
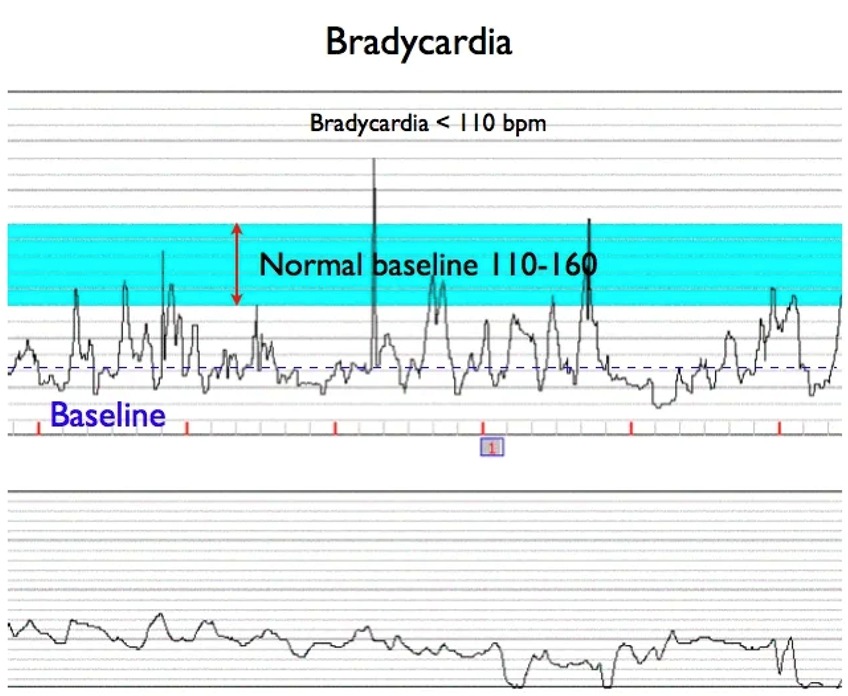
- Bradycardia = below 110 bpm — may suggest maternal beta-blocker use, hypothermia, hypoglycemia, hypothyroidism, fetal heart block, or interruptions in fetal oxygenation.
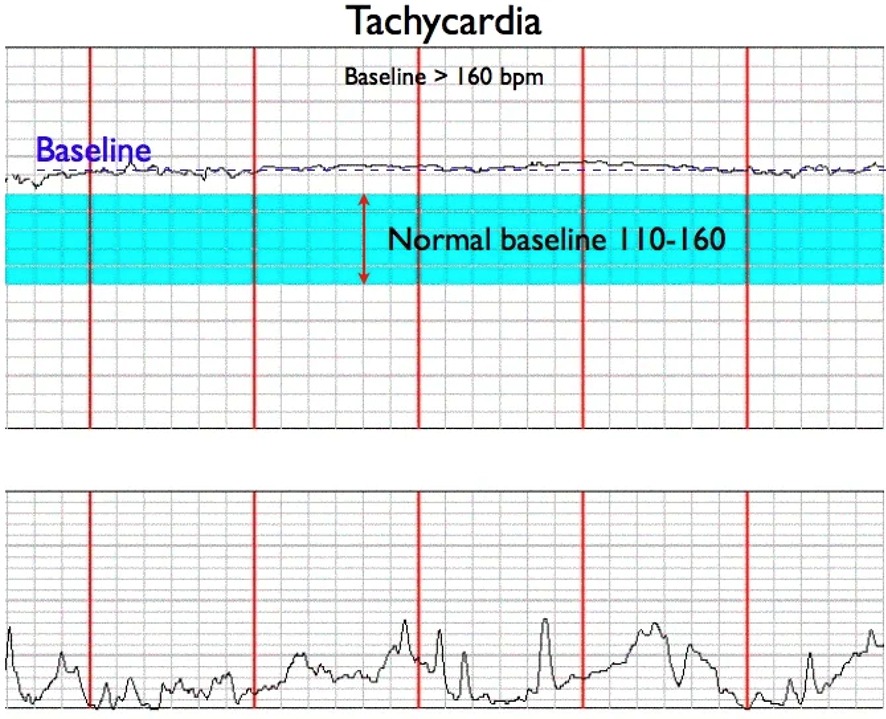
- Normal = 110 to 160 bpm — healthy fetal autonomic and cardiovascular system.
- Tachycardia = over 160 bpm — can be caused by maternal fever, infections, certain medications, hyperthyroidism, increased catecholamines, fetal anemia, arrhythmia, or oxygenation interruptions.
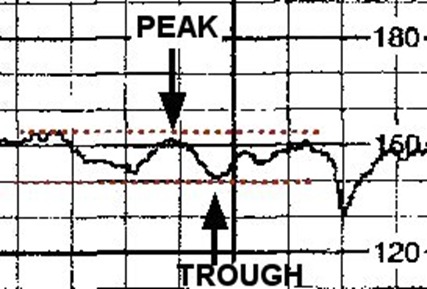
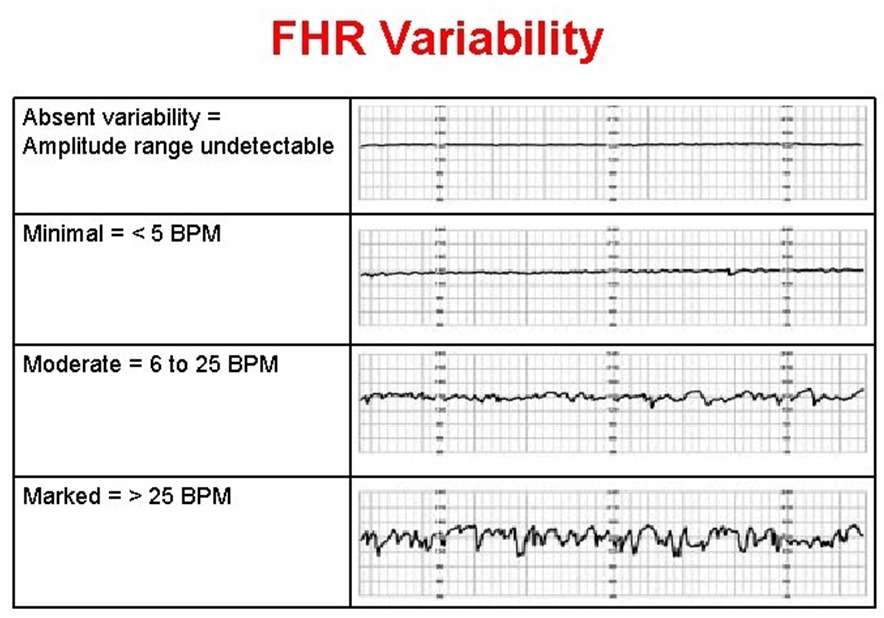
FHR Variability
Fluctuations in baseline that are irregular in amplitude and frequency , Measured in a 10-minute window , The amplitude is measured peak to trough — Is the result of integrated activity between the sympathetic and parasympathetic branches of the autonomic nervous system.
- Absent = amplitude undetectable — poor predictors of fetal metabolic acidemia or hypoxic injury.
- Minimal = amplitude 0 to 5 bpm — poor predictors of fetal metabolic acidemia or hypoxic injury.
- Moderate = amplitude 6 to 25 bpm —- Indicates a well-oxygenated fetus and a functional autonomic nervous system, suggesting the absence of significant hypoxia or metabolic acidemia.
- Marked = amplitude over 25 bpm — It may be a normal variant or an exaggerated autonomic response to transient or sustained interruption of fetal oxygenation.
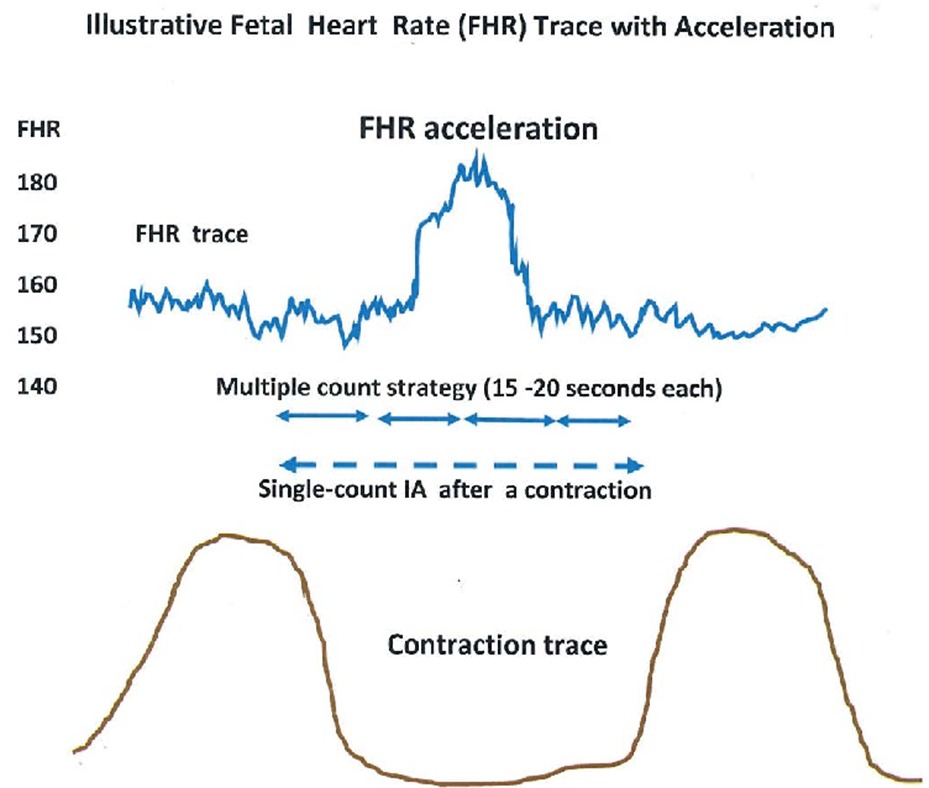
Accelerations
- An abrupt increase in the FHR. often linked to fetal movements, a positive sign of fetal well-being, reflecting adequate oxygenation and absence of metabolic acidemia.
- An abrupt increase in the FHR. Before 32 weeks of gestation, accelerations should last ≥10 sec and peak ≥10 bpm above baseline. As of 32 weeks gestation, accelerations should last ≥15 sec and peak ≥15 bpm above baseline.
- A prolonged acceleration is ≥2 minutes but less than 10 minutes. An acceleration of 10 minutes or more is considered a change in baseline.
Decelerations
An abrupt decrease in FHR below the baseline. The decrease is ≥15 bpm, lasting ≥15 secs and <2 minutes from onset to return to baseline.
- Early Deceleration
- A gradual decrease and return to baseline of the FHR associated with a uterine contraction. The nadir of the FHR and the peak of the contraction occur at the same time. The deceleration's onset, nadir, and termination are usually coincident with the onset, peak, and termination of the contraction.
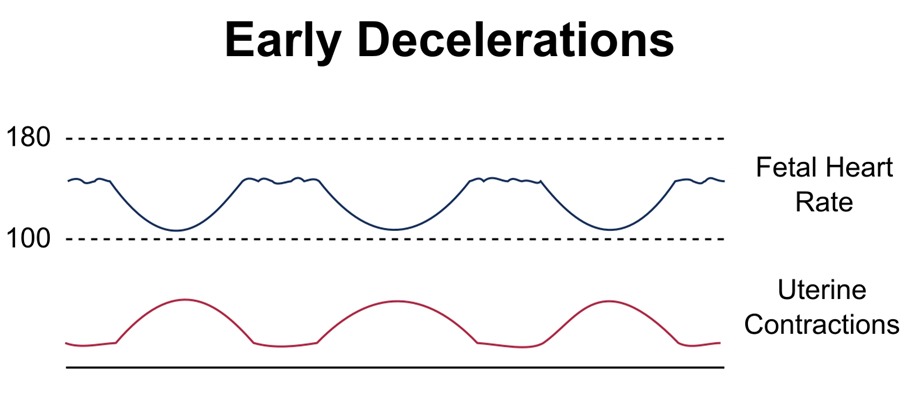
- A gradual decrease and return to baseline of the FHR associated with a uterine contraction. The nadir of the FHR and the peak of the contraction occur at the same time. The deceleration's onset, nadir, and termination are usually coincident with the onset, peak, and termination of the contraction.
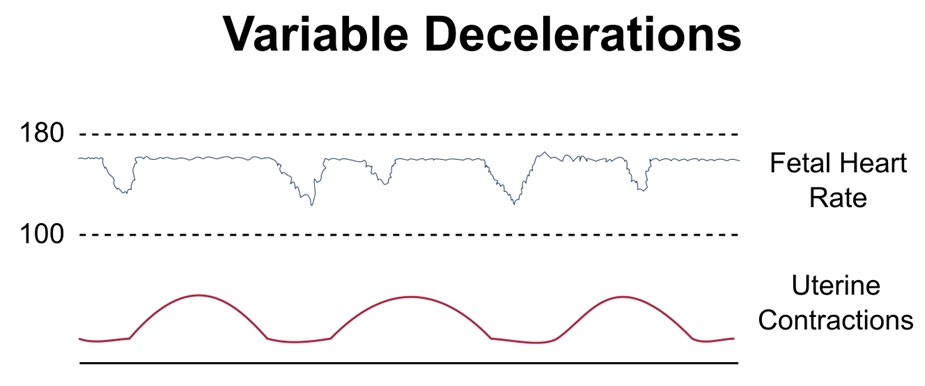
- Variable Deceleration
- The onset, depth, and duration of variable decelerations commonly vary with successive uterine contractions.
- Results from transient umbilical cord compression
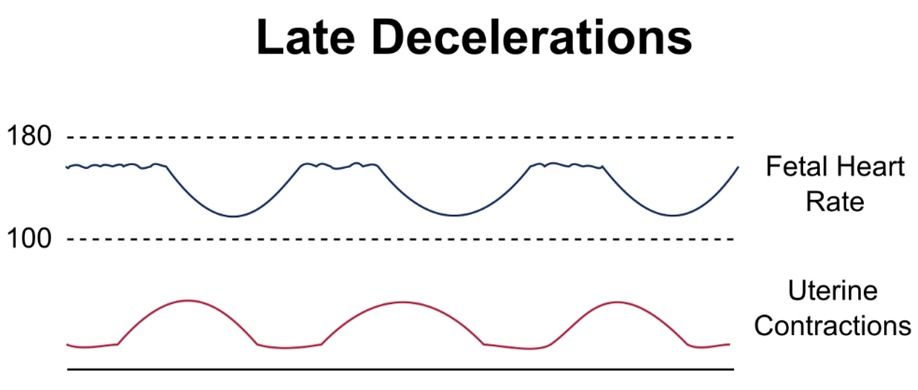
- Late Deceleration
- A gradual* decrease and return to baseline of the FHR associated with a uterine contraction. The deceleration is delayed in timing, with the nadir of the deceleration occurring after the peak of the contraction. The onset, nadir, and recovery usually occur after the onset, peak, and termination of a contraction.
- Usually a reflex response to transient fetal hypoxemia, indicating reduced oxygen delivery to the fetus.
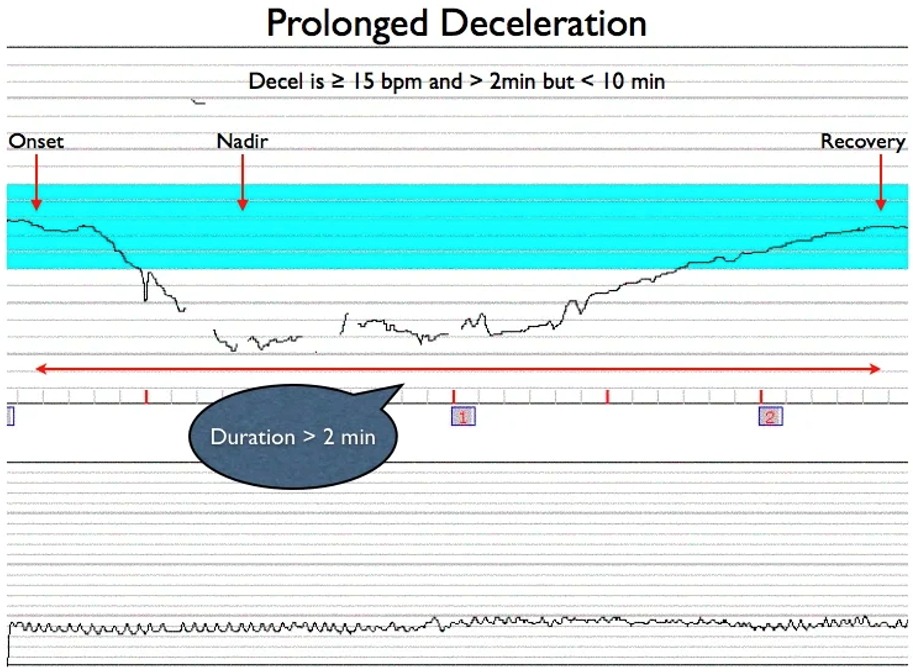
- Prolonged Deceleration
- Defined by a drop in FHR of ≥15 bpm lasting 2 to 10 minutes, prolonged decelerations are critical signs that may indicate more severe or extended interruptions in fetal oxygenation.
- A decrease in FHR below the baseline of 15 bpm or more, lasting at least 2 minutes but <10 minutes from onset to return to baseline. A prolonged deceleration of 10 minutes or more is considered a change in baseline.
- Sinusoidal Pattern
- A rare, smooth, sine wave-like pattern in FHR, historically associated with severe fetal anemia. The exact pathophysiology remains unclear, but its presence demands careful evaluation and consideration of fetal well-being.
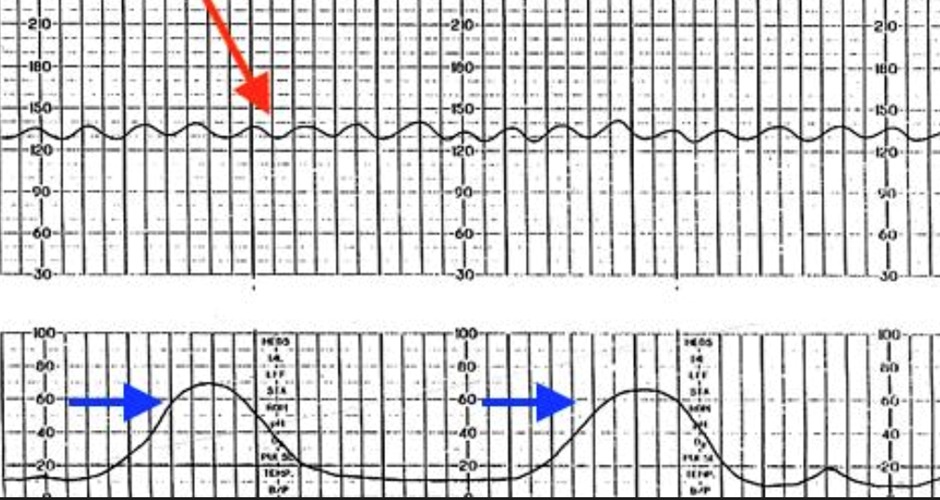
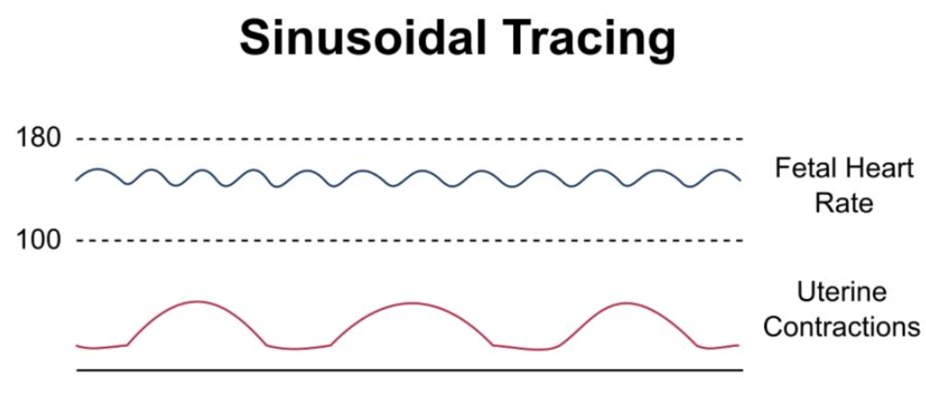
- A rare, smooth, sine wave-like pattern in FHR, historically associated with severe fetal anemia. The exact pathophysiology remains unclear, but its presence demands careful evaluation and consideration of fetal well-being.
Interpretation of an FHR tracing
|
NICHD criteria for category I, II, and III FHR tracings |
|
|
Category I |
All of the following criteria must be present. Tracings meeting these criteria are predictive of normal fetal acid-base balance at the time of observation.
|
|
Category III |
Category III tracings are predictive of abnormal fetal acid-base status at the time of observation. Prompt evaluation is indicated and most parturients will require expeditious intervention, such as change in position, treatment of hypotension, and discontinuation of any uterotonic drugs being administered. Category III tracings include either (1) or (2) below.
|
|
Category II |
FHR tracing does not meet criteria for either category I or III and is considered indeterminate. |
Management of intrapartum fetal heart rate tracings
|
Management of intrapartum fetal heart rate tracings |
||
| Fetal heart rate tracing | Possible etiologies and interpretation | Management |
|
Category I |
||
|
Baseline 110 to 160 beats per minute with moderate variability and no late or variable decelerations. Accelerations and early decelerations may be present or absent. |
This is a normal tracing. |
Intermittent or continuous fetal monitoring based on clinical status and underlying risk factors. Review every 30 minutes in the first stage and every 15 minutes in the second stage of labor. |
|
Category II |
||
| Intermittent variable decelerations (<50% of contractions) | Common finding usually associated with normal outcome. | No intervention required. |
| Recurrent variable decelerations (>50% of contractions) | Umbilical cord compression. May be associated with impending acidemia, especially if progressive increase in depth, duration, and frequency. Moderate variability and/or accelerations suggest fetus is not currently acidemic. |
Reposition mother to left or right lateral. Amnioinfusion is an option. Adjunctive measures to promote fetal oxygenation (intravenous fluid bolus, reduce uterine contraction frequency) may be useful. Initiate scalp stimulation to provoke fetal heart rate acceleration, which is a sign that the fetus is not acidotic.
Delivery is indicated if tracing does not improve and acidemia suspected. |
| Recurrent late decelerations | Transient or chronic uteroplacental insufficiency, such as from hypotension, tachystole, or maternal hypoxia. Accelerations and/or moderate variability suggest fetus is not currently acidemic. |
Reposition mother to left or right lateral. Adjunctive measures to promote fetal oxygenation include intravenous fluid bolus, reduce uterine contraction frequency. Persistent late decelerations with minimal variability and absent accelerations suggest fetal acidemia; this is even more likely if variability is absent (category III). Initiate scalp stimulation to provoke fetal heart rate acceleration, which is a sign that the fetus is not acidotic.
Delivery is indicated if tracing does not improve. |
| Fetal tachycardia (baseline heart rate greater than 160 beats per minute for at least 10 minutes) | Infection, medication, maternal medical disorders, obstetric complications, fetal tachyarrhythmia (typically rate over 200 beats per minute). Fetal acidemic more likely when associated with minimal or absent variability, absent accelerations, and/or recurrent decelerations. |
Treat underlying cause, if known. Initiate scalp stimulation to provoke fetal heart rate acceleration, which is a sign that the fetus is not acidotic.
Delivery is indicated if tracing does not improve and acidemia suspected. |
| Bradycardia (baseline heart rate less than 110 beats per minute for at least 10 minutes) | Acute onset may be due to hypotension, umbilical cord occlusion, rapid fetal descent, tachysystole, abruption, uterine rupture. Fetal acidemia more likely when associated with minimal or absent variability and absent accelerations during baseline periods. | Treat underlying cause, if known. Initiate scalp stimulation to provoke fetal heart rate acceleration, which is a sign that the fetus is not acidotic. Delivery is indicated if tracing does not improve and acidemia suspected. |
| Prolonged decelerations (15 beats per minute drop below baseline for more than 2 and less than 10 minutes) | ||
| Minimal variability | Fetal sleep, medication, fetal acidemia. If due to fetal sleep, should recover in 20 to 60 minutes. If due to maternal medication, should recover as medication wears off. |
If decreased fetal oxygenation suspected, reposition mother to left or right lateral. Adjunctive measures to promote fetal oxygenation include intravenous fluid bolus, reduce uterine contraction frequency. Initiate scalp stimulation to provoke fetal heart rate acceleration, which is a sign that the fetus is not acidotic.
If no improvement and no accelerations, delivery is indicated if acidemia suspected or confirmed by scalp pH. |
|
Tachysystole (more than 5 contractions in 10 minutes, averaged over 30 minutes) with fetal heart rate changes.
Tachysystole that is spontaneous and associated with a normal fetal heart rate pattern does not require treatment, but the possibility of placental abruption as the underlying etiology should be considered. |
Spontaneous labor: Tachysystole may be associated with fetal acidemia if accompanied by recurrent fetal heart rate decelerations. |
Reposition mother to left or right lateral, intravenous fluid bolus. If ineffective, reduce uterine contraction frequency with a tocolytic.
Initiate scalp stimulation to provoke fetal heart rate acceleration, which is a sign that the fetus is not acidotic. |
| Induction or augmentation. | Decrease or stop uterotonic medications. Reposition mother to left or right lateral, intravenous fluid bolus. If ineffective, reduce uterine contraction frequency with a tocolytic. Initiate scalp stimulation to provoke fetal heart rate acceleration, which is a sign that the fetus is not acidotic. | |
|
Category III |
||
| Absent baseline variability and recurrent late decelerations, recurrent variable decelerations, or bradycardia | Increased risk of fetal acidemia. | Prepare for delivery and reposition mother to left or right lateral, intravenous fluid bolus. Initiate scalp stimulation to provoke fetal heart rate acceleration, which is a sign that the fetus is not acidotic. If no improvement after conservative measures and scalp stimulation does not result in acceleration, delivery is advisable. |
| Sinusoidal | Increased risk of hypoxemia. Risk of acidemia increased if prolonged or amplitude of 15 beats per minute or more. | Prepare for delivery and reposition mother to left or right lateral, intravenous fluid bolus. Initiate scalp stimulation to provoke fetal heart rate acceleration, which is a sign that the fetus is not acidotic. If no improvement after conservative measures and scalp stimulation does not result in acceleration, delivery is advisable. |
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.