Definition
Labour is defined as the process characterised by regular, painful uterine contractions that result in progressive dilation and effacement of the cervix, leading to the descent and eventual expulsion of the foetus.Signs and symptoms of labour
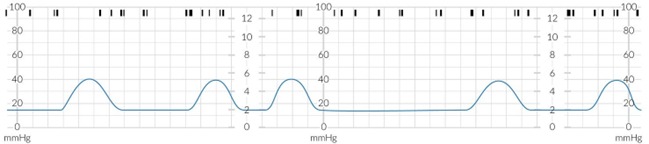
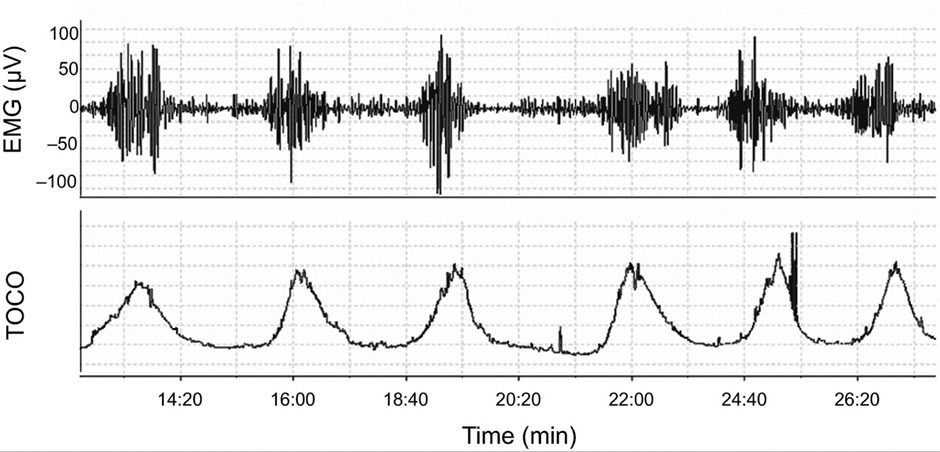
- Contractions: Regular, increasingly intense and painful uterine contractions are the hallmark of labor. Unlike Braxton Hicks contractions ("false labor"), true labor contractions do not subside with movement or changes in activity and become more frequent and stronger over time.
- Cervical Changes: The cervix dilates (opens) and effaces (thins out) in preparation for the baby to pass through the birth canal. These changes are often monitored by healthcare providers to assess the progression of labor.
- Rupture of Membranes (Water Breaking): This can occur as a sudden gush or a slow leak of amniotic fluid from the vagina. For some women, this happens before labor starts; for others, it occurs during labor.
- Bloody Show: The loss of the mucus plug that seals the cervix can indicate that labor is approaching. It may be accompanied by a small amount of blood or spotting, known as the "bloody show."
- Lower Back Pain and Cramping: Pain and discomfort may not be limited to contractions. Many women experience a dull ache in their lower back and cramping that can be similar to menstrual cramps.
- Diarrhea or Nausea: Some women may experience gastrointestinal disturbances such as nausea or loose stools as labor approaches, due to the body's natural preparation processes.
- Increased Pressure: As the baby descends into the pelvis, there may be increased pressure in the pelvic area, sometimes described as feeling like the baby is "bearing down."
- Nesting Instinct: Some women experience a burst of energy and the urge to "nest" or prepare the home for the baby's arrival shortly before labor begins.
Contractions
| Contractions | ||||
| Time | Characteristics | |||
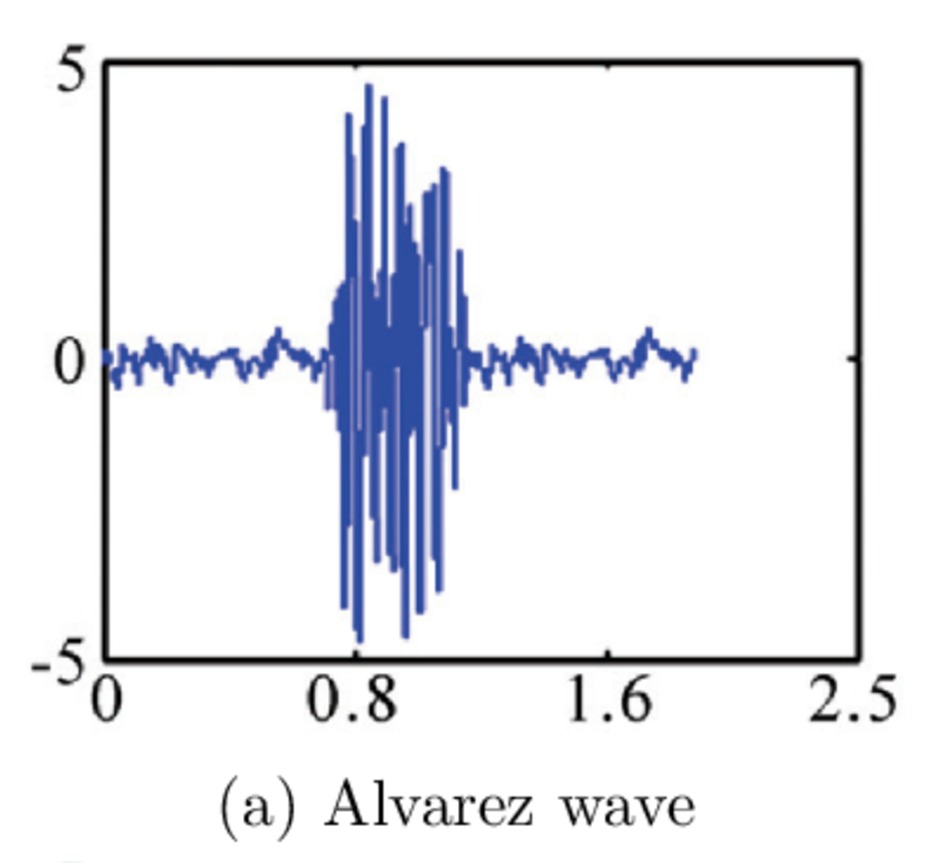
| Uterine contractions during pregnancy | Alvarez-waves |
|
|
|
| Braxton Hicks contractions(false labour) |
|
|
||
| Prelabor |
|
|
||
| Labor | Stage 1: cervical dilation and effacement till fully dilated cervix |
|
|
|
| Stage 2: foetal expulsion |
|
|
||
| Stage 3: placental expulsion or afterbirth |
|
|
||
| Afterpains |
|
|
||
Rupture of Membranes
The breaking of the amniotic sac and the release of the amniotic fluid surrounding the fetus.
- Spontaneous Rupture of Membranes (SROM): This is the most common type of ROM, occurring naturally as labor begins or progresses. It is not induced by medical interventions. The timing of SROM varies; it may happen at the onset of labor or during any stage of labor before the delivery of the baby.
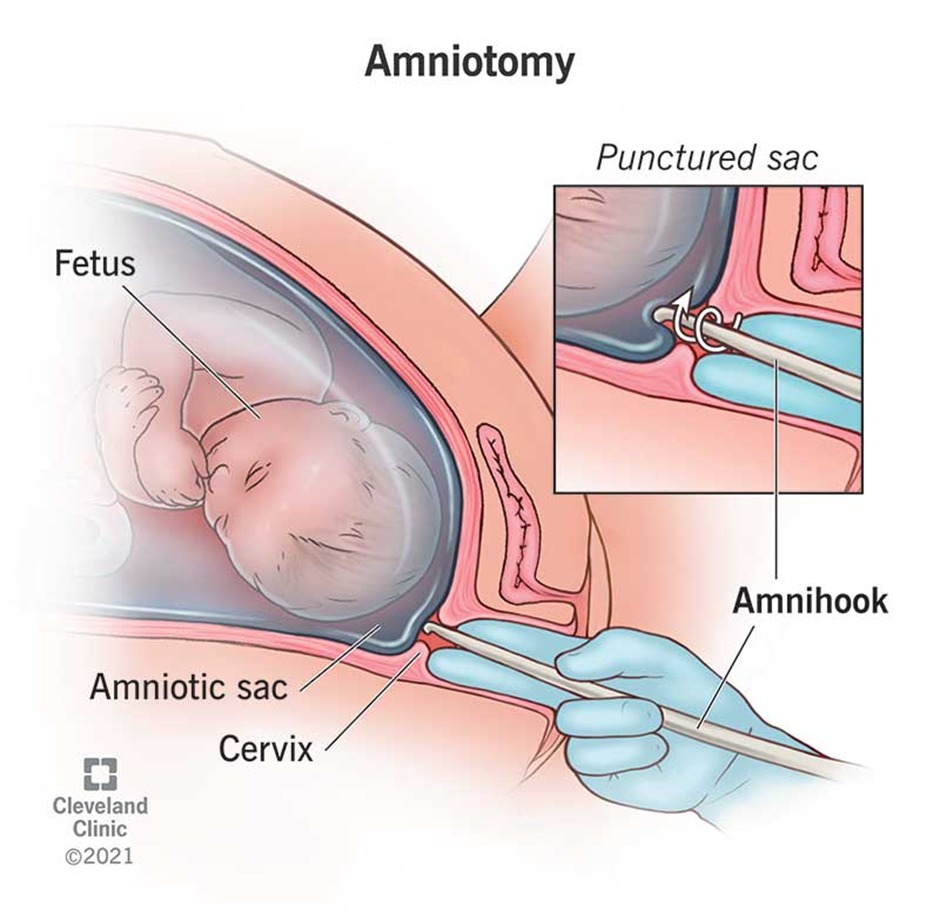
- Artificial Rupture of Membranes (Amniotomy): This is a deliberate medical procedure performed to induce or accelerate labor. It involves the use of a special instrument to puncture the amniotic sac. Amniotomy is done for various reasons, including to strengthen labor contractions or to allow for internal monitoring of the fetus.
- Delayed Rupture of Membranes: Occurs when the membranes rupture late in the labor process, sometimes just before or during the actual delivery of the baby. This is less common and can be spontaneous.
Abnormal Rupture of Membranes
- Premature Rupture of Membranes (PROM): Refers to ROM that occurs before labor begins, regardless of the gestational age. If PROM happens near the term (37 weeks or later), it may lead to labor within a short period.
- Preterm Premature Rupture of Membranes (PPROM): This is a subtype of PROM that occurs before 37 weeks of gestation and before the onset of labor. PPROM increases the risk of preterm delivery, infections, and complications for both the mother and the fetus.
- Prolonged Rupture of Membranes: When more than 18-24 hours pass between the rupture of the membranes and the onset of labor, it is considered prolonged. This condition raises the risk of infection for both the mother and the baby.
Clinical Features and Diagnostics
- The typical clinical presentation includes a sudden gush of fluid from the vagina, which can also present as a continuous leak. The fluid is usually pale yellow or clear.
- Diagnostic Approaches:
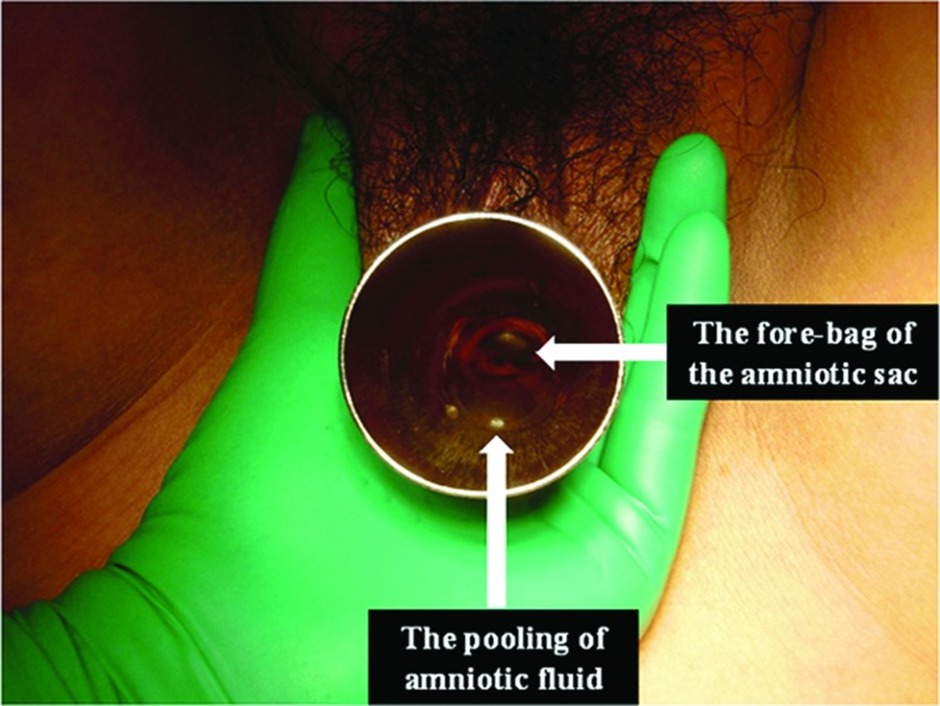
- Sterile Speculum Examination: This is performed to confirm ROM if the diagnosis is uncertain. During this examination, healthcare providers look for evidence of amniotic fluid leakage.
- Pooling: The visual observation of amniotic fluid in the posterior fornix of the vagina.
- Litmus Test or Nitrazine Test: These tests check the pH of the fluid. Amniotic fluid has a higher pH compared to normal vaginal secretions, which can help confirm the ROM.

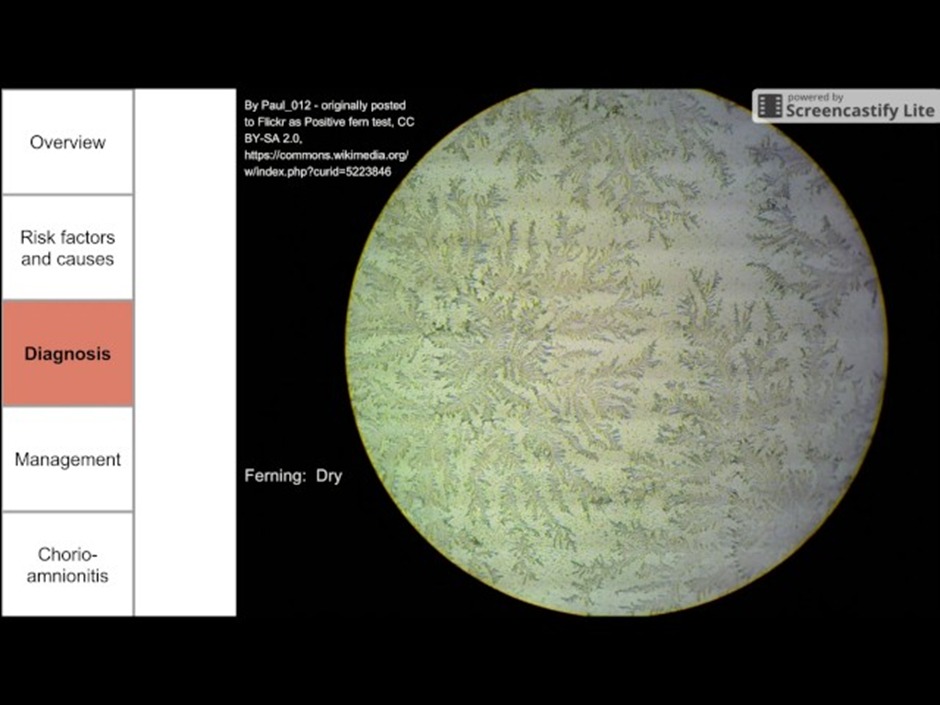
- Ferning Test: A microscopic examination of the dried fluid can show a fern-like pattern, indicative of amniotic fluid due to its unique salt composition.
Cervical evaluation
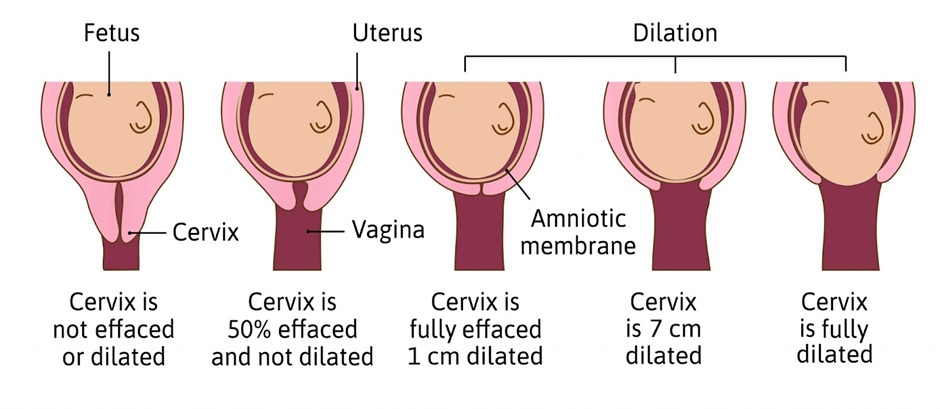
- Cervical Dilation
- Definition: The opening of the cervix measured in centimeters, from 0 (closed) to 10 (fully dilated).
- Significance: Dilation is a primary indicator of labor progress. It reflects the cervical opening necessary for the fetus to pass through the birth canal.
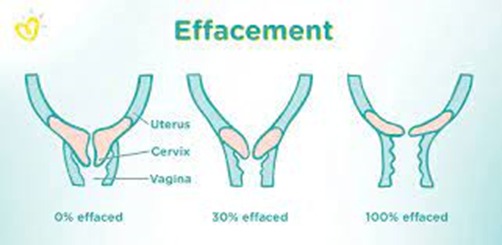
- Cervical Effacement
- Definition: The thinning and shortening of the cervix, measured as a percentage from 0% (no effacement, or fully thick) to 100% (completely thinned out).
- Significance: Effacement typically precedes or accompanies dilation, especially for first-time mothers, and is an important indicator of the cervix preparing for delivery.
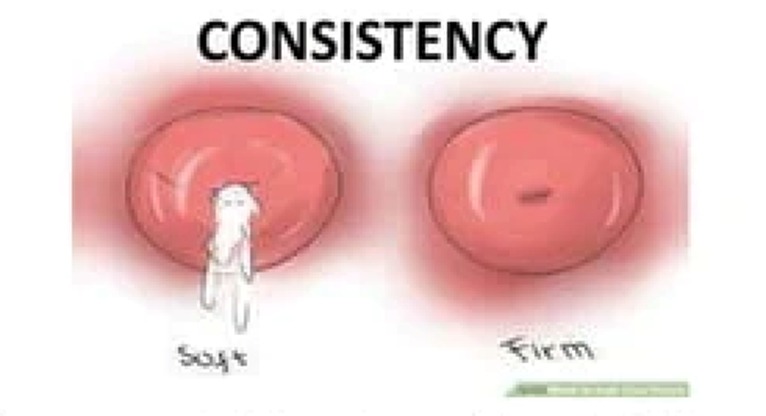
- Cervical Consistency
- Definition: The texture of the cervix, which can range from firm (similar to the tip of a nose), to medium (like the lips), to soft (resembling the inside of a cheek).
- Significance: The softening of the cervix (ripening) is an important precursor to effacement and dilation.
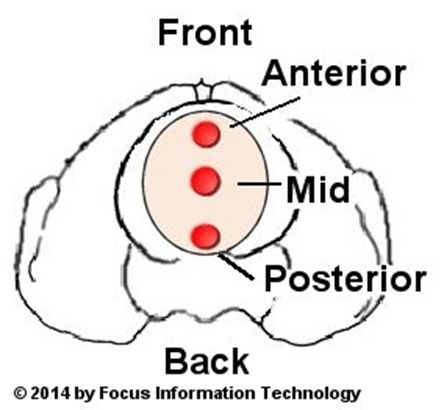
- Cervical Position
- Definition: The position of the cervix within the vagina, which can be posterior (towards the back), mid-position, or anterior (towards the front).
- Significance: As labor progresses, the cervix typically moves from a more posterior to an anterior position, making it more accessible for examination and indicating progression towards delivery.
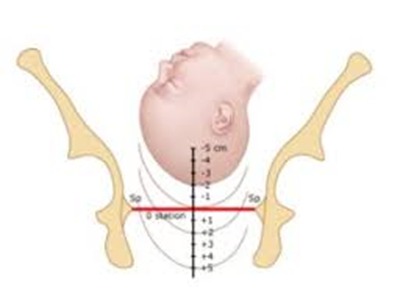
- Fetal Station
- Definition: The position of the baby's presenting part (usually the head) in relation to the ischial spines of the pelvis, measured in centimeters from -5 (high, not engaged in the pelvis) to +5 (at the pelvic outlet, ready for birth).
- Significance: Fetal station provides information about the descent of the fetus through the birth canal and is an important component of assessing labor progress.
Stages of labor
| Stages of labor | ||||
| Stage | Characteristics and Normal Progress | Duration: Nulliparous Patients | Duration: Multiparous Patients | |
| First Stage of Labor |
The first stage of labor is the period from the onset of labor until the cervix is completely dilated. This stage is divided into two phases:
|
≤ 20 hours | ≤ 14 hours | |
| Latent Phase |
|
|||
| Active Phase |
|
|
|
|
| Second Stage of Labor |
|
|
|
|
| Passive Phase |
|
|||
| Active Phase |
|
|||
| Third Stage of Labor |
|
|
|
|
| Fourth Stage of Labor |
|
|
|
|
Management of Labour
First Stage of Labor
- Analgesia: Offer analgesia upon request to manage labor pain effectively.
- Fetal Heart Rate Monitoring: Continuous or intermittent monitoring to assess fetal well-being.
- Fetal Position Assessment: Use Leopold maneuvers (abdominal examination) and pelvic examination (palpation of fetal sutures/fontanelles) to determine fetal position. If unclear, perform an ultrasound.
- Cervical Dilation and Fetal Head Descent: Regularly assess to gauge labor progress.
- Management of Bleeding: In case of heavier bleeding but with normal maternal vital signs and fetal heart tracing, continue with planned delivery and frequent observation.
Second Stage of Labor
- Positioning: Assist the mother in finding comfortable and safe positions to facilitate childbirth.
- Guidance Through Delivery: Guide the delivery of the fetus through the vaginal canal, understanding the mechanics of childbirth and expected fetal movements.
- Umbilical Cord Clamping: Delay clamping the umbilical cord for no less than 30–60 seconds post-delivery to enhance neonatal outcomes.
Third Stage of Labor
- Active Management: Implement active management techniques to reduce the risk of postpartum hemorrhage. This includes administering oxytocin to induce stronger uterine contractions.
- Controlled Cord Traction: Use the Brandt-Andrews maneuver for placenta delivery if it does not occur spontaneously.
- Placenta Examination: Check the placenta for completeness, including the presence of an umbilical cord, complete amniotic membranes, and three blood vessels (one vein, two arteries), to ensure no retained products.
- Repair Lacerations: Address any obstetric lacerations promptly.
Fourth Stage of Labor
- Monitoring: Vigilantly monitor the mother to rule out postpartum hemorrhage or preeclampsia. This stage focuses on the mother's recovery, including continued uterine contractions to minimize blood loss and the expulsion of any remaining contents.
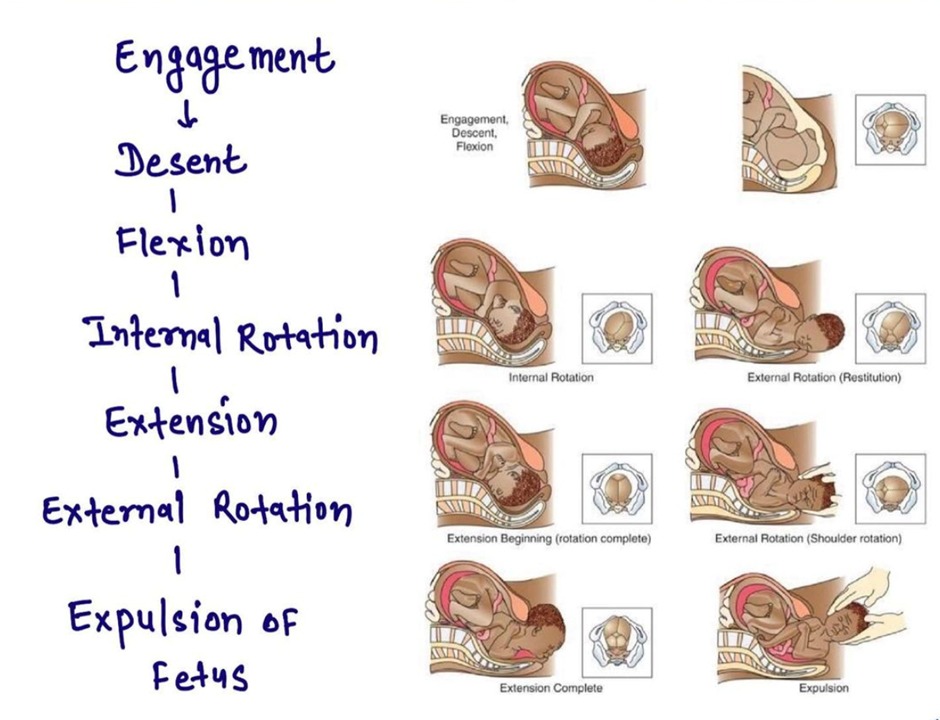
The cardinal movements during childbirth
- Engagement: The fetal head enters the pelvic inlet in an orientation that best fits the shape of the pelvis. This usually means the narrowest diameter of the fetal head aligns with the widest diameter of the pelvic inlet.
- Descent: Following engagement, the fetus begins to move down the birth canal. Descent is influenced by maternal contractions, gravity, and the bearing-down efforts of the mother.
- Flexion: As the fetal head descends, it encounters resistance from the pelvic floor and cervix, causing the chin to move toward the chest. This increases the presenting diameter's chance to fit the pelvic dimensions.
- Internal Rotation: The fetal head rotates within the pelvis to align with the pelvic outlet. This rotation is typically about 90 degrees, moving from a transverse to an anterior-posterior position to match the pelvic outlet's shape.
- Extension: Once the fetal head reaches the pelvic floor, it extends so that the head can pass under the pubic symphysis. This movement involves the fetal head moving upward and forward.
- Restitution and External Rotation: After the head emerges, it rotates (restitution) to realign with the shoulders, which have remained in the position they assumed during internal rotation. The shoulders then undergo external rotation to navigate through the pelvis, and this movement causes the head to complete its rotation to the position it held before internal rotation.
- Expulsion: Finally, the rest of the fetus's body is delivered, typically with the anterior shoulder first, followed by the posterior shoulder, and then the torso and legs.
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.