سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
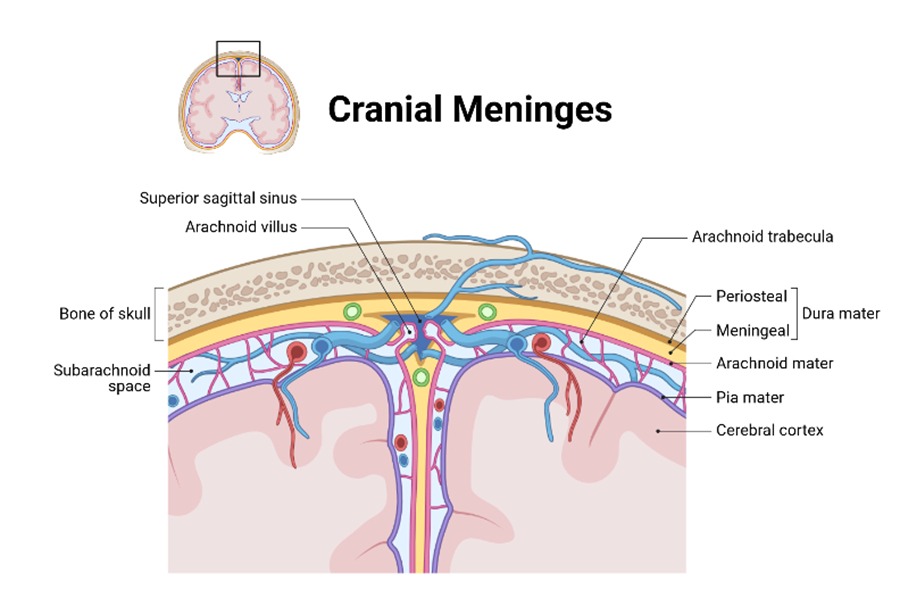
Introduction
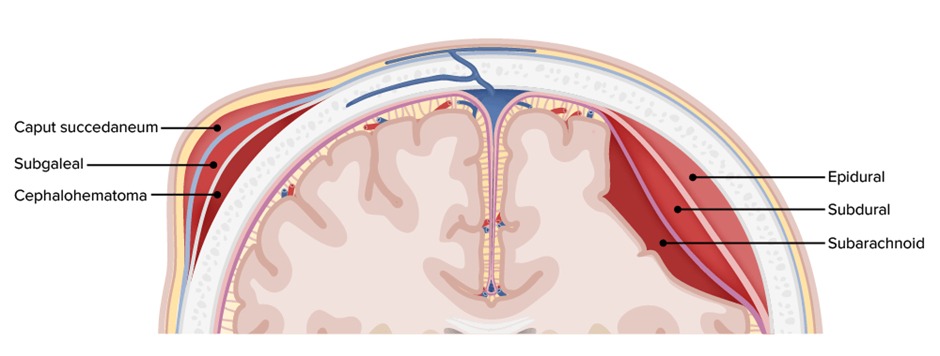
- Subdural hematoma (SDH) is usually secondary to traumatic head injury
- Subdural hematomas have been classified based on the time they become clinically symptomatic following injury into acute, subacute and chronic subdural hematomas
- A typical clinical scenario includes a patient with history of head injury that is followed by worsening neurological state
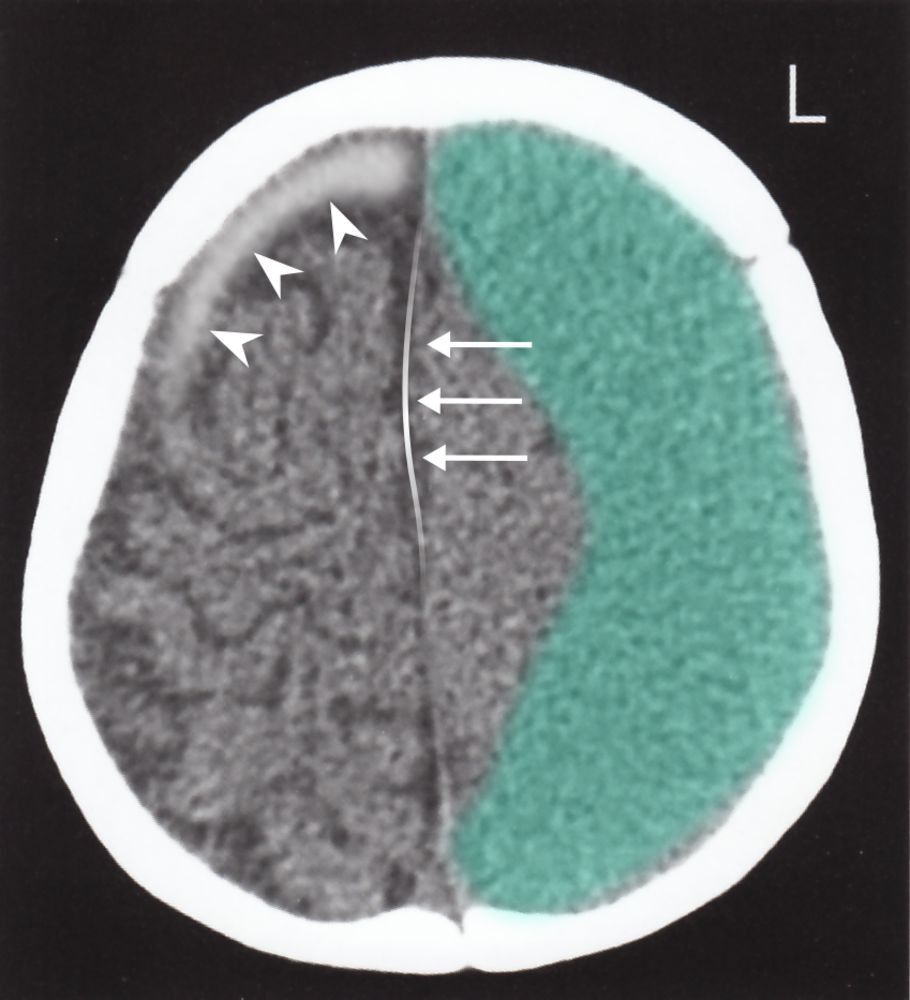
- CT shows a crescent shaped collection of blood that DOES cross the suture lines. The midline might shift in some cases
| Extradural hemorrhage | Subdural hemorrhage | Subarachnoid hemorrhage | |
|---|---|---|---|
| Location |
|
|
|
| Pathophysiology |
|
|
|
| Clinical presentation |
|
|
|
| CT findings | Convex shaped |
|
|
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Classifications Based on Timing
- Acute subdural hematoma — less than 3 days
- Subacute subdural hematoma — 4 - 21 days
- Chronic subdural hematoma — more than 21 days
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
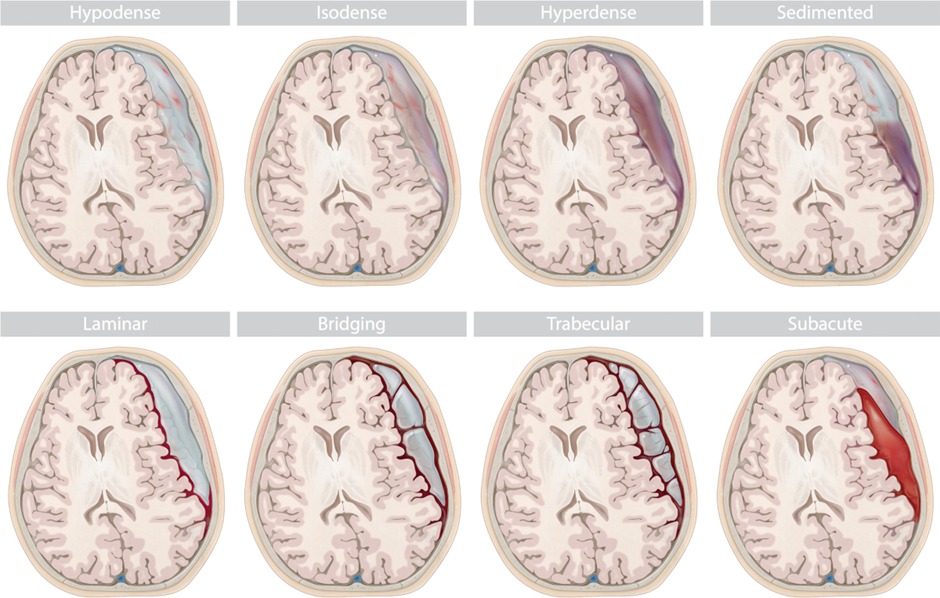
Classifications Based on CT scan
- This classification depends on the density of the hematoma in relation to the adjacent brain tissue
- Acute SDH is hyperdense (white)
- Chronic SDH is hypodense

سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
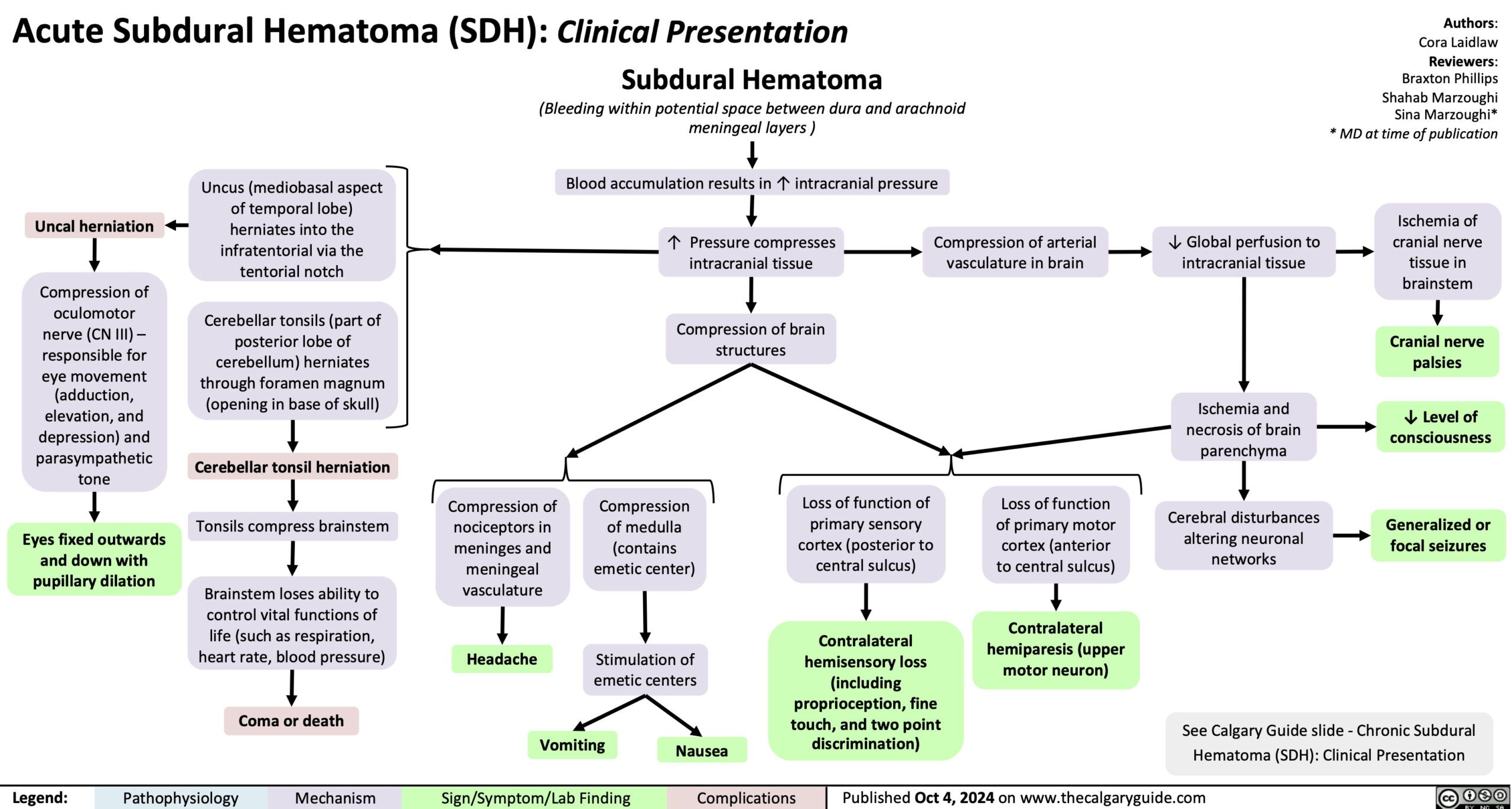
Acute Subdural Hematoma
- Motor vehicle accidents are common causes of aSDH in children and young adults; older adults, especially those on anticoagulants and antiplatelet agents, may present after a minor fall
- Acute SDH are bilateral in approximately one-third of cases (epidural hematomas are only bilateral in 3% of cases only)
- It is accompanied by a fracture in the cranial vault or base of the skull in nearly 80% of cases
- Treatment of acute SDH requires evacuation of the hematoma (a craniotomy is nearly always necessary for this condition)
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Clinical Presentation in Acute SDH
- An acute SDH should be suspected in a patient who presents with a severe head injury whose neurological state is either failing to improve or deteriorating
- An acute SDH must be distinguished from epidural hematomas that usually have a lucid interval of improvement
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Acute SDH Prognosis
- Many factors may influence outcome of patients such as patient age and size of the hematoma
- Mortality rates in patients younger than 40 years were nearly 20%, whereas age 40 - 80 years was associated with a mortality rate of 65%. Patients older than 80 years had a mortality rate of nearly 88%
- Many patients do not regain their previous levels of functioning, especially after an acute subdural hematoma that was very severe and required surgical intervention
- Poor prognostic indicators include low Glasgow coma score on admission (less than 5), pupillary abnormalities, alcohol use, and difficulty in controlling intracranial pressure
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
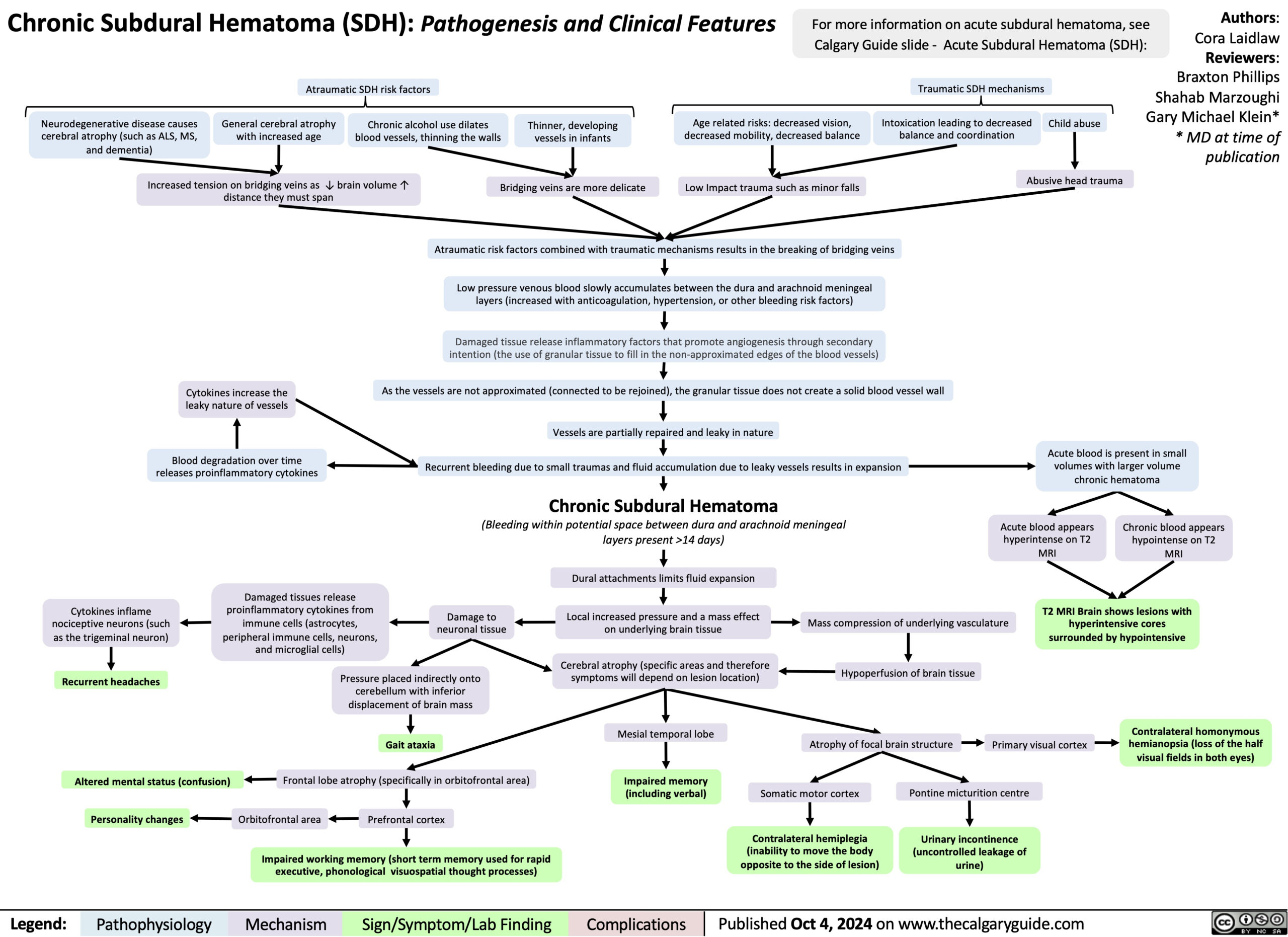
Chronic Subdural Hematoma
- One-third of patients have no definite history of preceding head trauma
- Non-traumatic chronic SDH is related to rupture of fragile bridging veins in a relatively atrophic brain (patients are usually over 50 years)
- Shrinkage of the brain (due to atrophy) allows the brain to move more freely. A relatively minor injury can lead to movement of the brain and subsequent rupture of the bridging veins
- Chronic SDH is mainly concerning for patients who are on anticoagulant therapy. They are prone to develop SDH after a relatively minor trauma
- Treatment of chronic SDH requires evacuation of the hematoma (through burr holes or craniotomy)
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Clinical Presentation in Chronic SDH
- The predominant characteristic symptom is a decline in the level of consciousness and the patient might become abruptly unconscious
- A progressive dementia (might be mistaken for Alzheimer’s disease). However, the course of the dementia in chronic SDH cases is usually more rapid and progressive
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Chronic SDH Prognosis
- Morbidity and mortality rates with surgical treatment of chronic subdural hematoma are estimated at 11% and 5%
- No clear prognostic indicators are associated with chronic SDH. However, early diagnosis and intervention before significant neurological deterioration may be related with a more favorable prognosis
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Diagnosis
- CT scan is the radiological investigation of choice
- Acute SDH is hyperdense (white)
- Chronic SDH is hypodense
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Treatment
- Treatment of subdural hematoma is craniotomy to evacuate the collection of blood
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.
فيديوهات الشرح
بطاقات تفاعلية
أسئلة ممارسة
اشترك الآن