سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Background
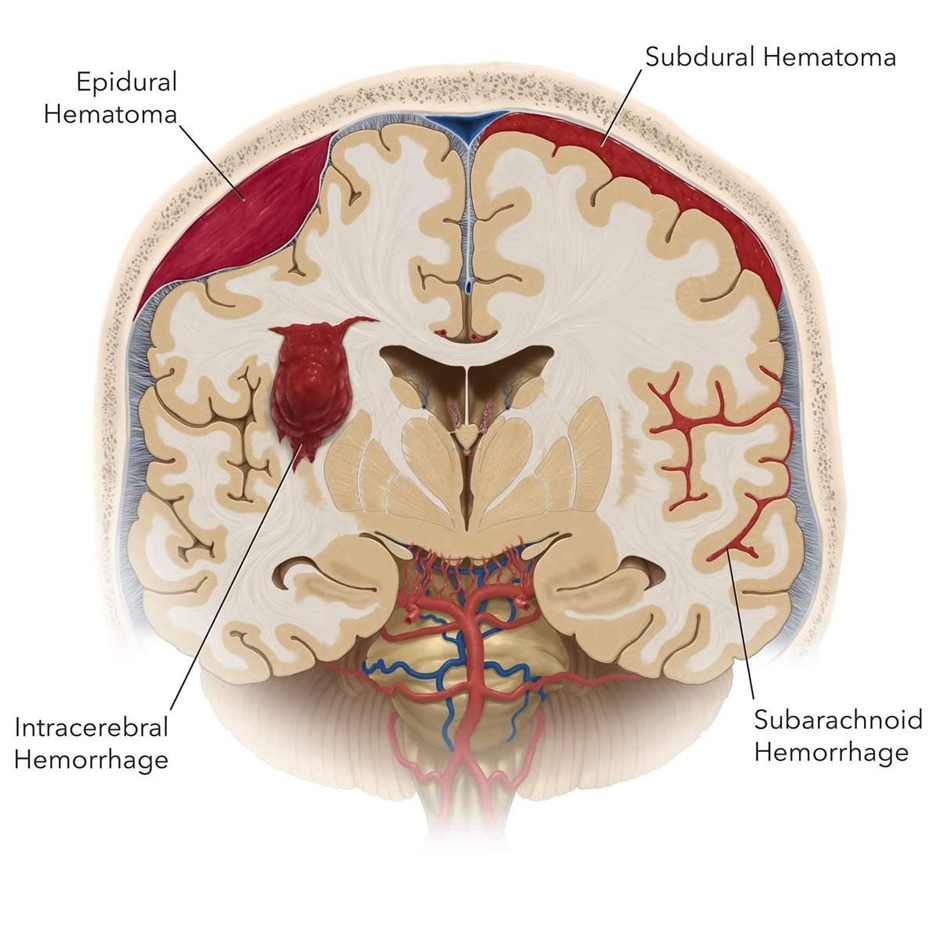
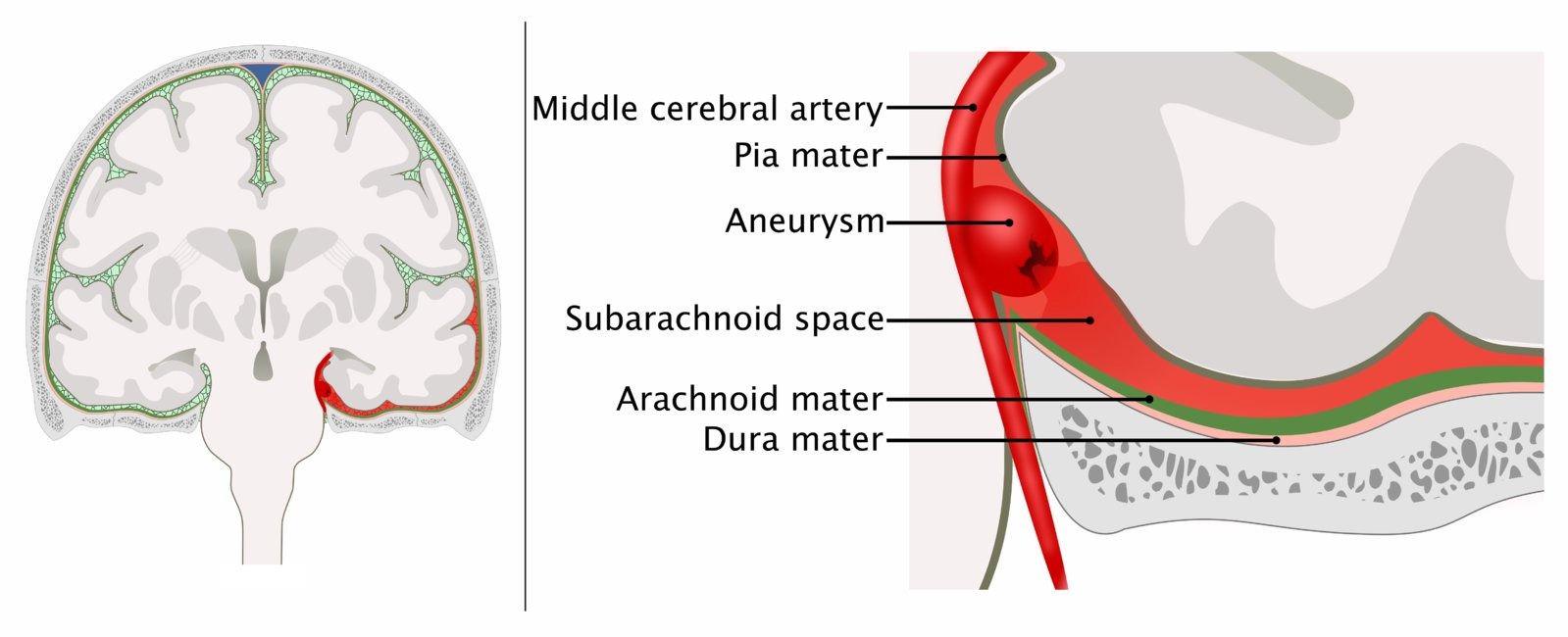
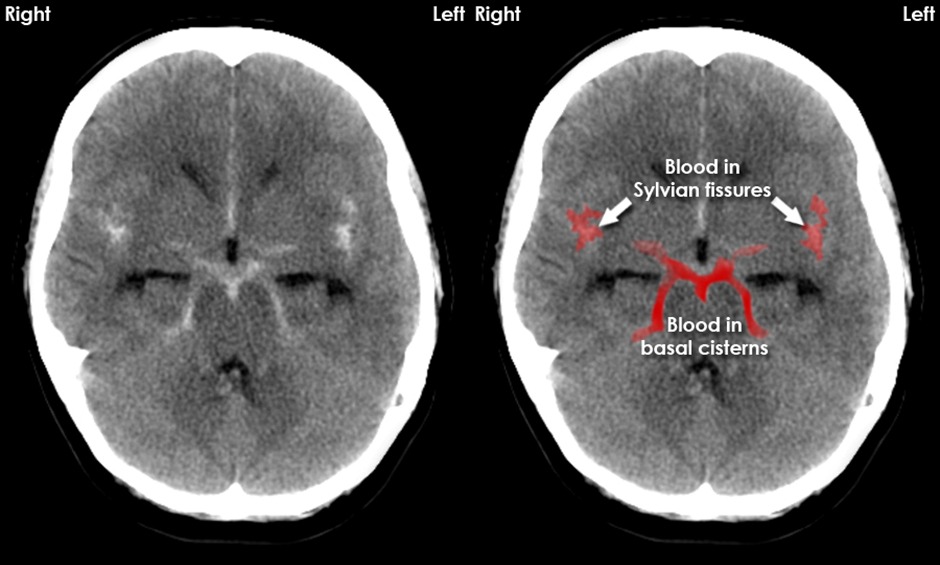
- Subarachnoid haemorrhage (SAH) refers to extravasation of blood (bleeding) into subarachnoid space (where cerebrospinal fluid is housed) between pia mater and arachnoid mater (usually secondary to head trauma)
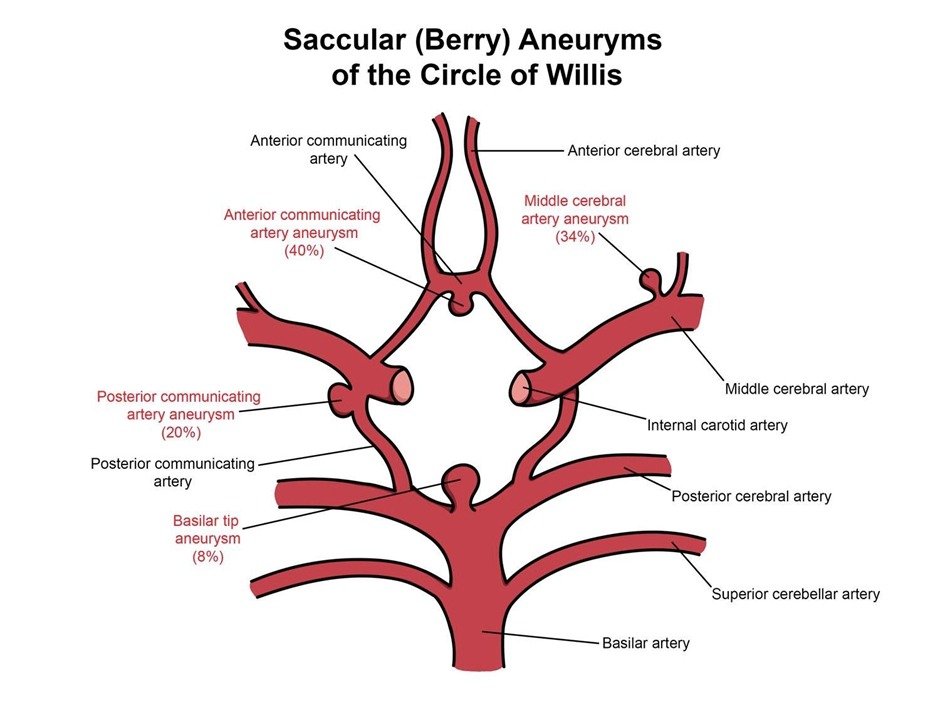
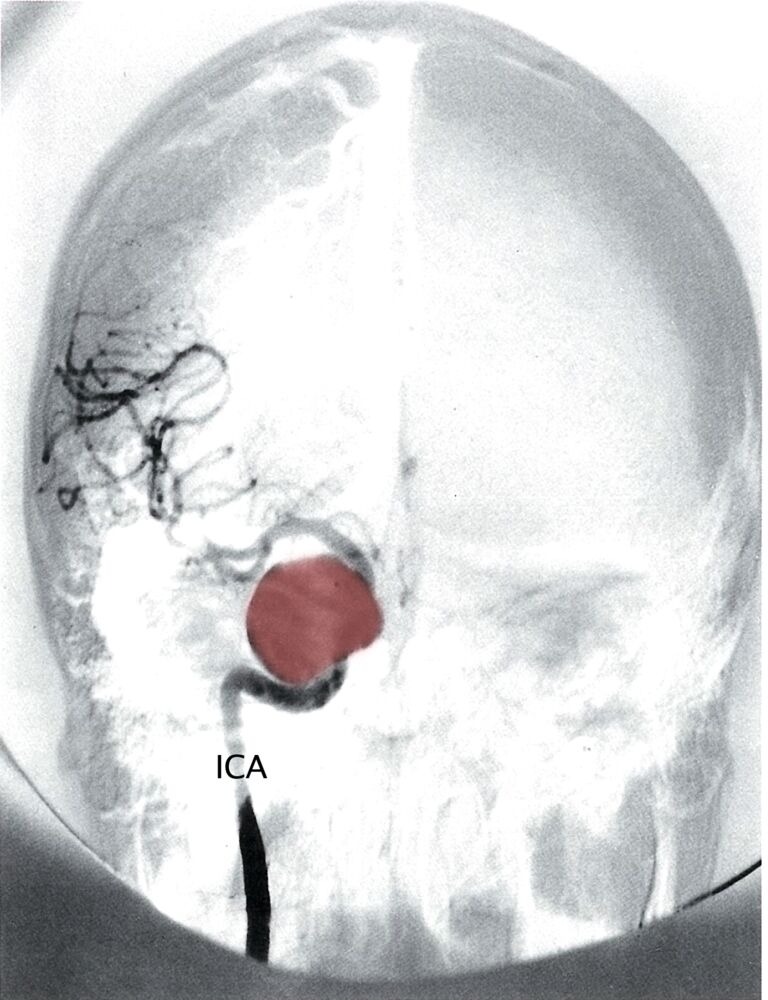
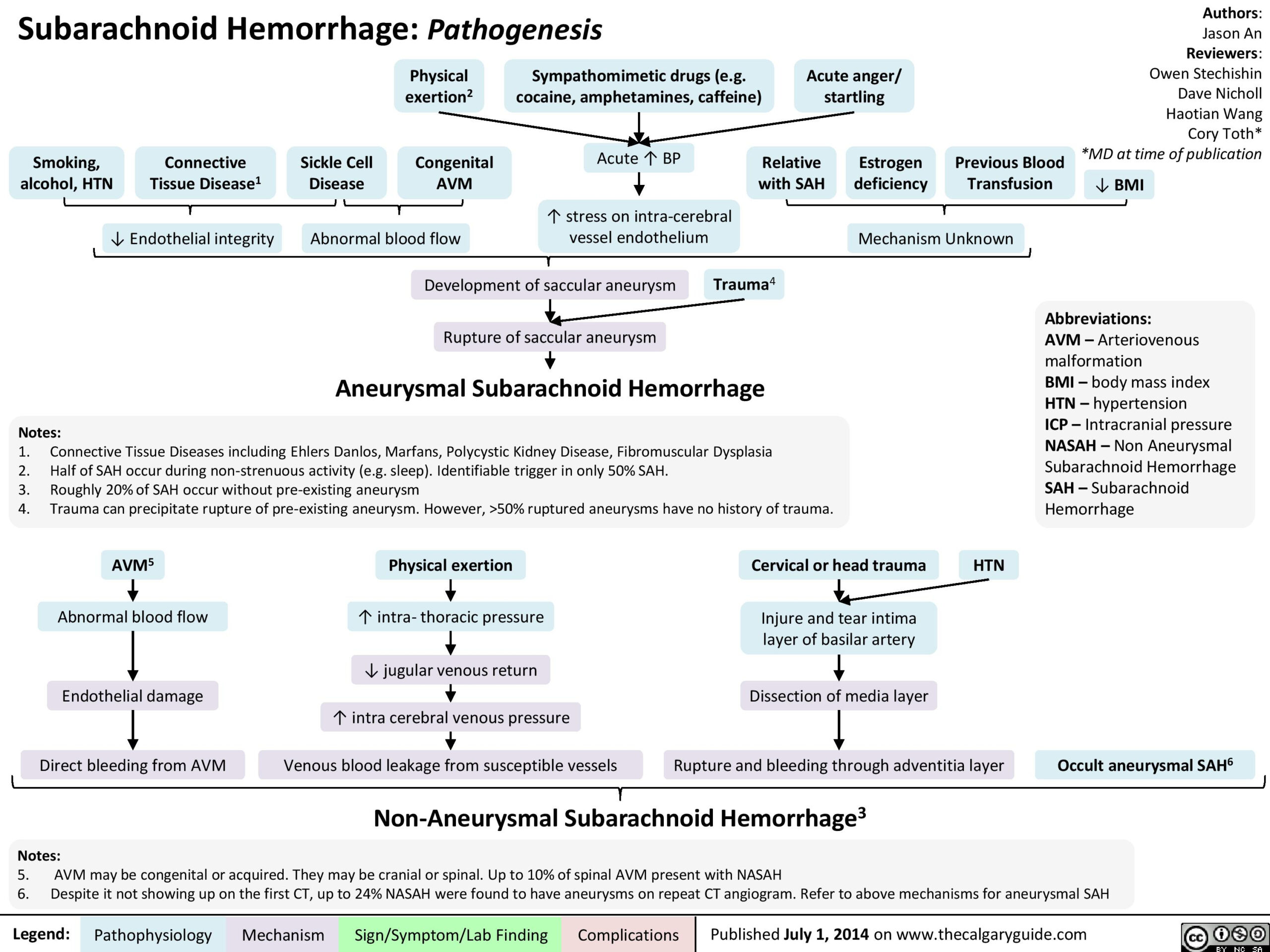
- Nontraumatic (spontaneous) SAH occurs in the setting of a ruptured cerebral saccular (berry) aneurysm or arteriovenous malformation (AVM)
- Prehospital mortality rates from acute SAH have been reported to be 22% to 26% and the course of symptoms is very rapid
- Patients complain of “worst headache of their life” or “thunderclap headache”
- Rupture of an aneurysm can result from an acute trigger, such as physical exertion or can occur in the absence of an acute trigger, such as in sleep
| Extradural hemorrhage | Subdural hemorrhage | Subarachnoid hemorrhage | |
|---|---|---|---|
| Location |
|
|
|
| Pathophysiology |
|
|
|
| Clinical presentation |
|
|
|
| CT findings | Convex shaped |
|
|
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Risk factors for SAH
- Smoking (most important preventable and modifiable factor)
- Hypertension
- Polycystic kidney disease
| For alert patients >15 years of age with new severe non-traumatic headache reaching maximum intensity within 1 hour. Patients require additional investigation for SAH if they meet any of the following criteria. | |
| 1 |
|
| 2 |
|
| 3 |
|
| 4 |
|
| 5 |
|
| 6 |
|
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Risk factors for rerupture
| Characteristics | Risk factors |
| Rerupture | |
| Residual aneurysm |
|
| Coiled aneurysm |
|
| De novo | |
| Formation |
|
| Growth and rupture |
|
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
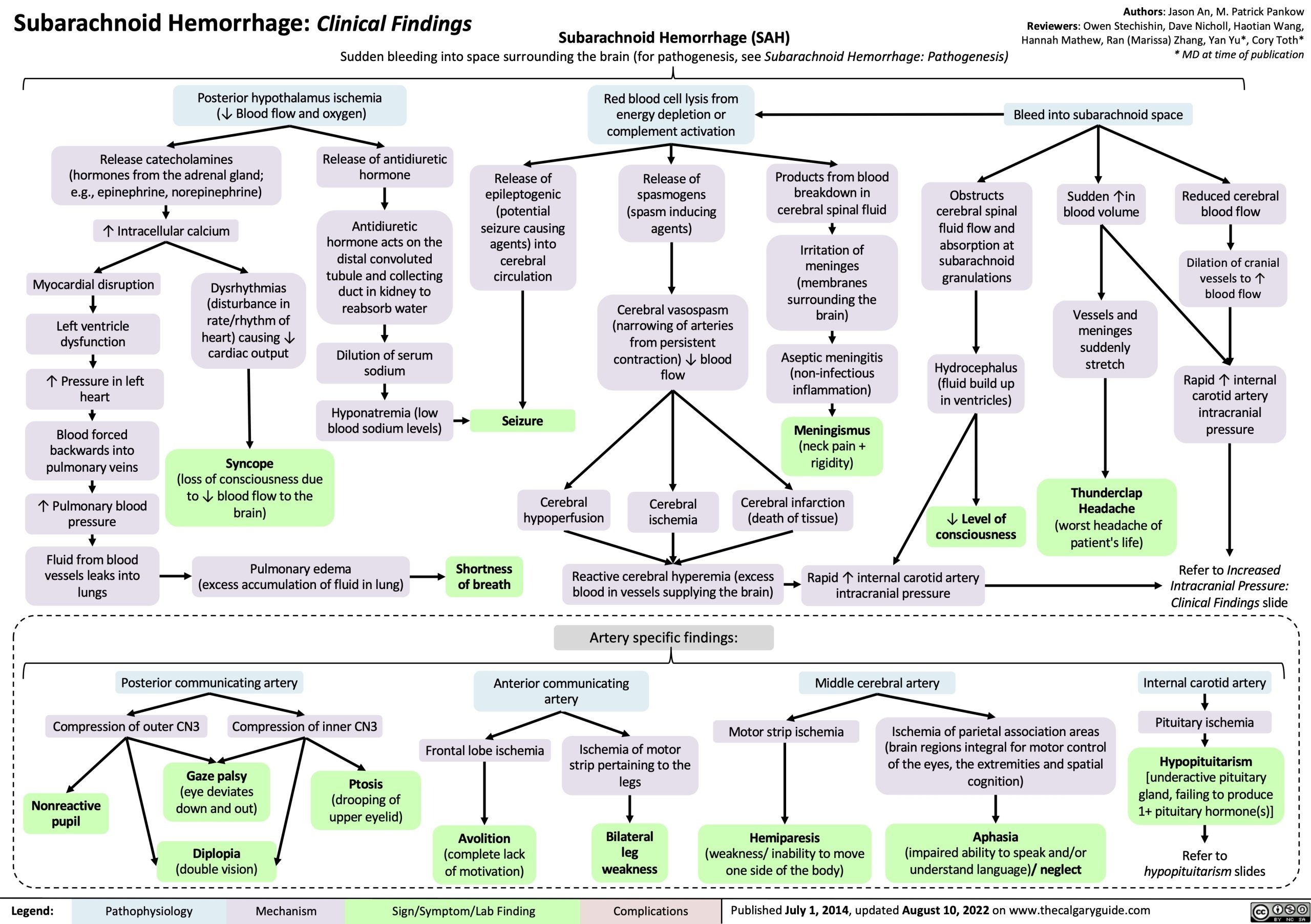
Clinical presentation
- Sudden onset of severe headache often described as “the worst headache of my life”
- Nausea and vomiting (secondary to increased intracranial pressure)
- Signs of meningeal irritation (nuchal rigidity)
- Photophobia and visual changes
- Focal neurological deficits
- Seizures
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Diagnosis
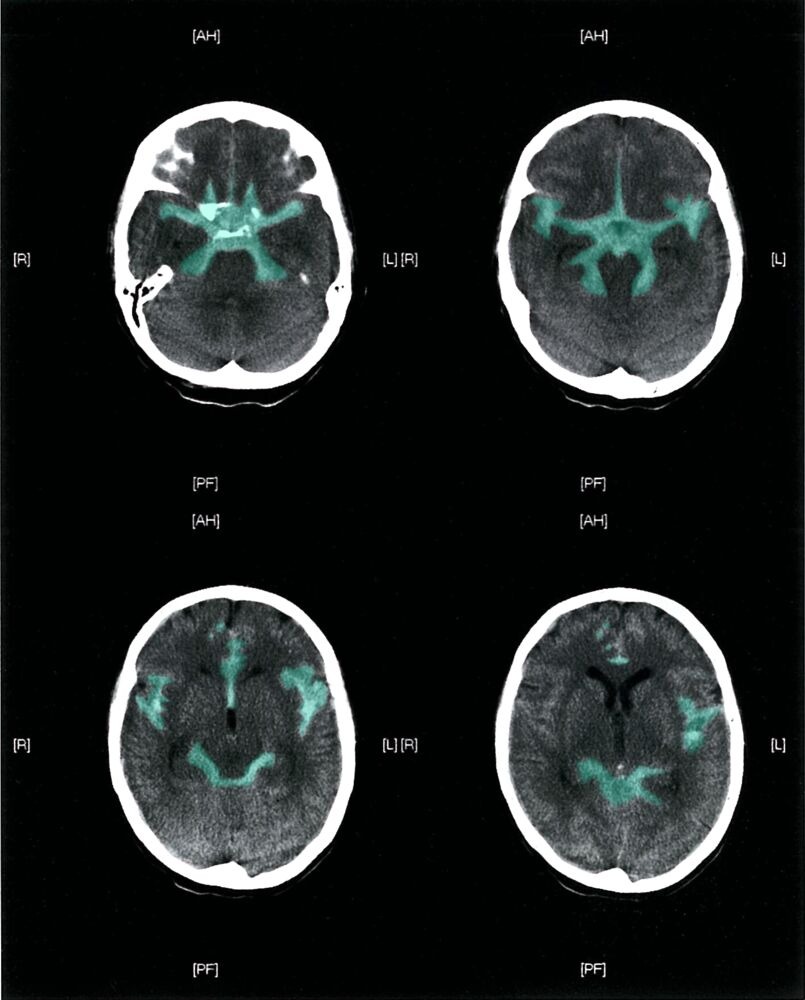
- CT head without contrast (hyperdensities in the suprasellar cisterns extending peripherally)
- When CT head without contrast is normal and there is still high suspicion for SAH (over 6 hours from onset of symptoms, lumbar puncture (LP_ is indicated
- LP shows xanthromia (bloody or yellow)
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Complications
- Arterial vasospasm can occur due to blood breakdown or rebelled 3-10 days after haemorrhage (prevented by nimodipine)
- Communicating and/or obstructive hydrocephalus
- Hyponatremia (secondary to development of SIADH)
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Treatment
- Medical (nimodipine as a prophylaxis to reduce the risk of vasospasm and delayed cerebral ischemia)
- Surgical (Aneurysmal repair)
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Mind Maps
| Overview of Subarachnoid Hemorrhage | |
|---|---|
| Clinical features |
|
| Complications |
|
| Diagnosis |
|
| Treatment |
|
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.
فيديوهات الشرح
بطاقات تفاعلية
أسئلة ممارسة
اشترك الآن