سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Background
- Peptic ulcer disease (PUD) is an erosion or defect in the mucosal lining of the stomach, duodenum, and sometimes the lower oesophagus (due to imbalance between the mucosal protective factors and gastric acid secretions)
- The leading cause is helicobacter pylori followed by nonsteroidal anti-inflammatory drugs (NSAIDs) use
- Risk factors include NSAIDs, smoking, stress and age (ulcer incidence increases with age)
- Associated conditions include: Zollinger-Ellison syndrome (suspect in patients with refractory duodenal ulcers), Behçet’s disease, and Crohn’s disease
| Gastric ulcer | Duodenal ulcer | |
| Pain |
|
|
| H. Pylori infection |
|
|
| Mechanism |
|
|
| Other causes |
|
|
| Risk of carcinoma |
|
|
| Helicobacter pylori infection | |
| Clinical presentation |
|
| Diagnosis |
|
| Treatment |
|
Version 2
Definition
- Peptic ulcer disease (PUD): Erosion or defect in the mucosal lining of the stomach, duodenum, and sometimes lower esophagus that extends through the muscularis mucosae (≥0.5 cm diameter)
Epidemiology
- ★ Prevalence: 5-10% lifetime risk in general population
- ★ Most common age:
- Duodenal ulcers: 30-55 years
- Gastric ulcers: 55-70 years
- ★ Gender:
- Duodenal ulcers: Male > Female (4:1)
- Gastric ulcers: Male = Female
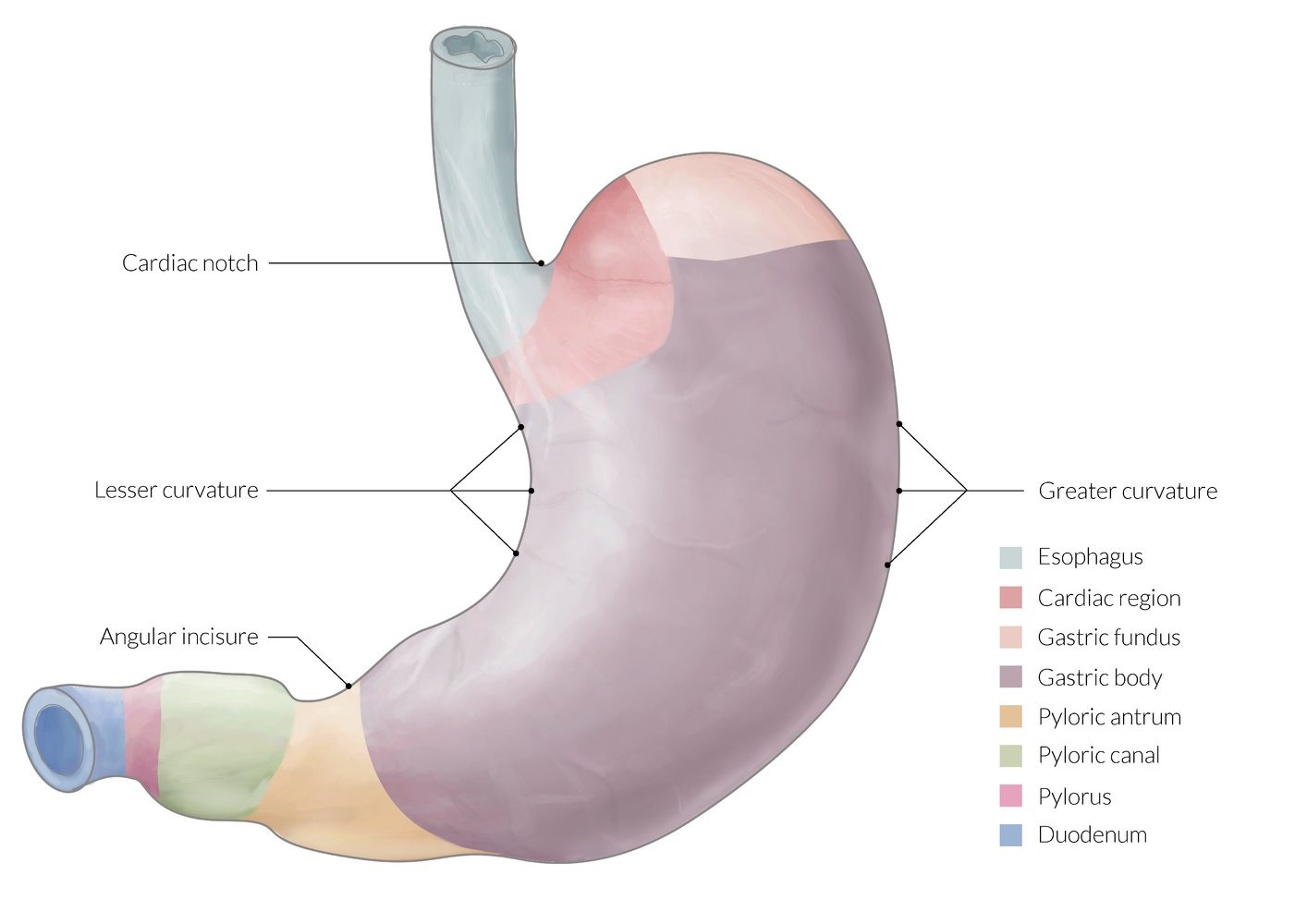
- ★ Most common location: First part of duodenum (duodenal bulb)
Risk Factors
- Major risk factors:
- ★ H. pylori infection (most important)
- ★ NSAIDs (including low-dose aspirin)
- Smoking (impairs healing)
- Advanced age (>60 years)
- Previous PUD history
- Associated conditions:
- ★ Zollinger-Ellison syndrome (gastrinoma) - suspect with refractory/multiple ulcers
- Behçet's disease
- Crohn's disease
- Systemic mastocytosis
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Types/Classification
| Feature | Gastric Ulcer | Duodenal Ulcer ★ |
| Frequency | 25% of PUD | ★ 75% of PUD (most common) |
| Pain timing |
|
|
| H. pylori association | 70% | ★ 90% |
| Pathophysiology | ↓ Mucosal protection | ↓ Mucosal protection OR ↑ Acid secretion |
| Other causes | ★ NSAIDs (most common after H. pylori) | Zollinger-Ellison syndrome |
| Malignancy risk |
|
|
| Most common location | ★ Lesser curvature of antrum | ★ First part of duodenum (within 3 cm of pylorus) |
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Helicobacter pylori
| Helicobacter pylori Infection | |
| Microbiology |
|
| Virulence factors |
|
| Clinical presentation |
|
| Diagnosis |
|
| Treatment |
|
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Clinical presentations
- Symptoms
- Asymptomatic (20%)
- Gnawing epigastric pain (most commonly at the upper quadrants)
- Nocturnal pain (due to circadian rhythm of gastric acid secretion)
- Hematemesis and Melina
- Perforated viscus (severe pain, guarding, rigidity, reduced bowel sounds, and signs of shock)
- Physical examination
- Abdominal tenderness
- Peritoneal signs if perforation
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Clinical Presentations - Version 2
Classic Presentations by Demographics
- ★ Young male (30-40 years) with epigastric pain relieved by food: Duodenal ulcer
- ★ Elderly patient (>60 years) with epigastric pain worsened by food + weight loss: Gastric ulcer (rule out malignancy)
- ★ Patient with multiple ulcers in unusual locations: Zollinger-Ellison syndrome
- ★ Patient on chronic NSAIDs with iron deficiency anemia: NSAID-induced ulcer with chronic bleeding
Symptoms
- Most common symptom: ★ Epigastric burning/gnawing pain (70-80%)
- Asymptomatic: 20% (especially elderly on NSAIDs)
- Other symptoms:
- Nausea/vomiting
- Bloating, belching
- Early satiety (gastric ulcer)
- ★ Nocturnal awakening (duodenal ulcer)
- Alarm symptoms (require immediate EGD):
- ★ Age >55 with new-onset dyspepsia
- ★ Unintentional weight loss
- ★ Progressive dysphagia
- ★ Persistent vomiting
- ★ GI bleeding (hematemesis, melena)
- ★ Iron deficiency anemia
- Family history of gastric cancer
Physical Examination
- Uncomplicated PUD:
- Epigastric tenderness
- Otherwise normal exam
- Complicated PUD:
- Perforation: ★ Rigid abdomen, rebound tenderness, absent bowel sounds
- Bleeding: Tachycardia, hypotension, melena/hematemesis
- Obstruction: Succussion splash, visible peristalsis
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Diagnosis
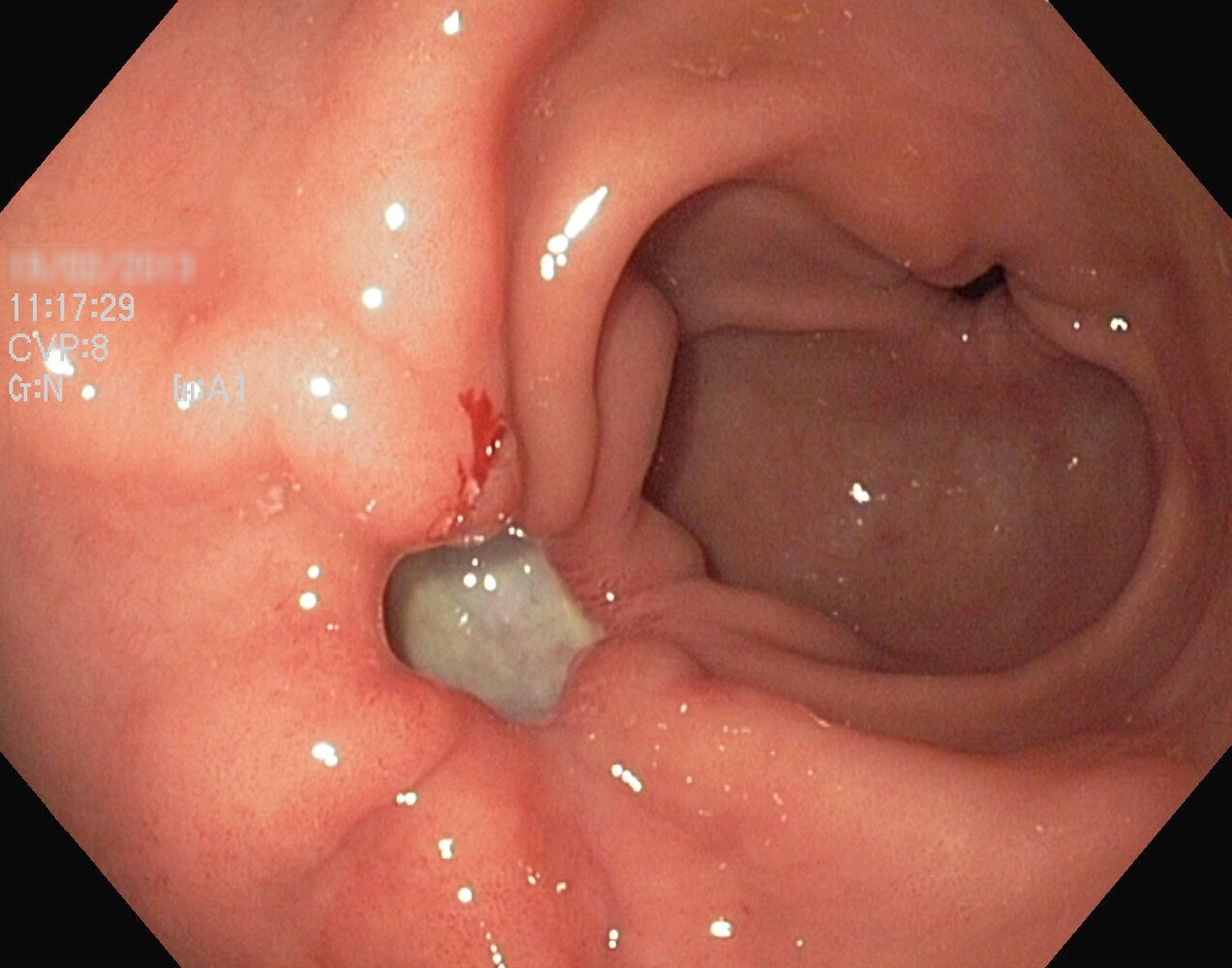
- Esophageogastroduodenoscopy (EGD) is the gold standard
- Biopsy (to differentiate between benign ulcers and malignancy)
- Abdominal and chest X-rays (to detect pneumoperitoneum secondary to perforation)
- Rule out malignancy
- Rule out helicobacter pylori
| EGD Findings | Probable cause |
| Shallow and multiple | NSAIDs |
| Big and heaped up margins | Malignancy |
| Single ulcer | Helicobacter pylori |
| Multiple ulcer in intestines | Gastrinoma |
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Diagnosis - Version 2
Diagnostic Algorithm
★ HIGH-YIELD DIAGNOSTIC APPROACH:
- Age <55 without alarm symptoms: Test and treat for H. pylori
- Age ≥55 OR alarm symptoms: Proceed directly to EGD
- Failed empiric therapy: EGD with biopsy
Diagnostic Tests
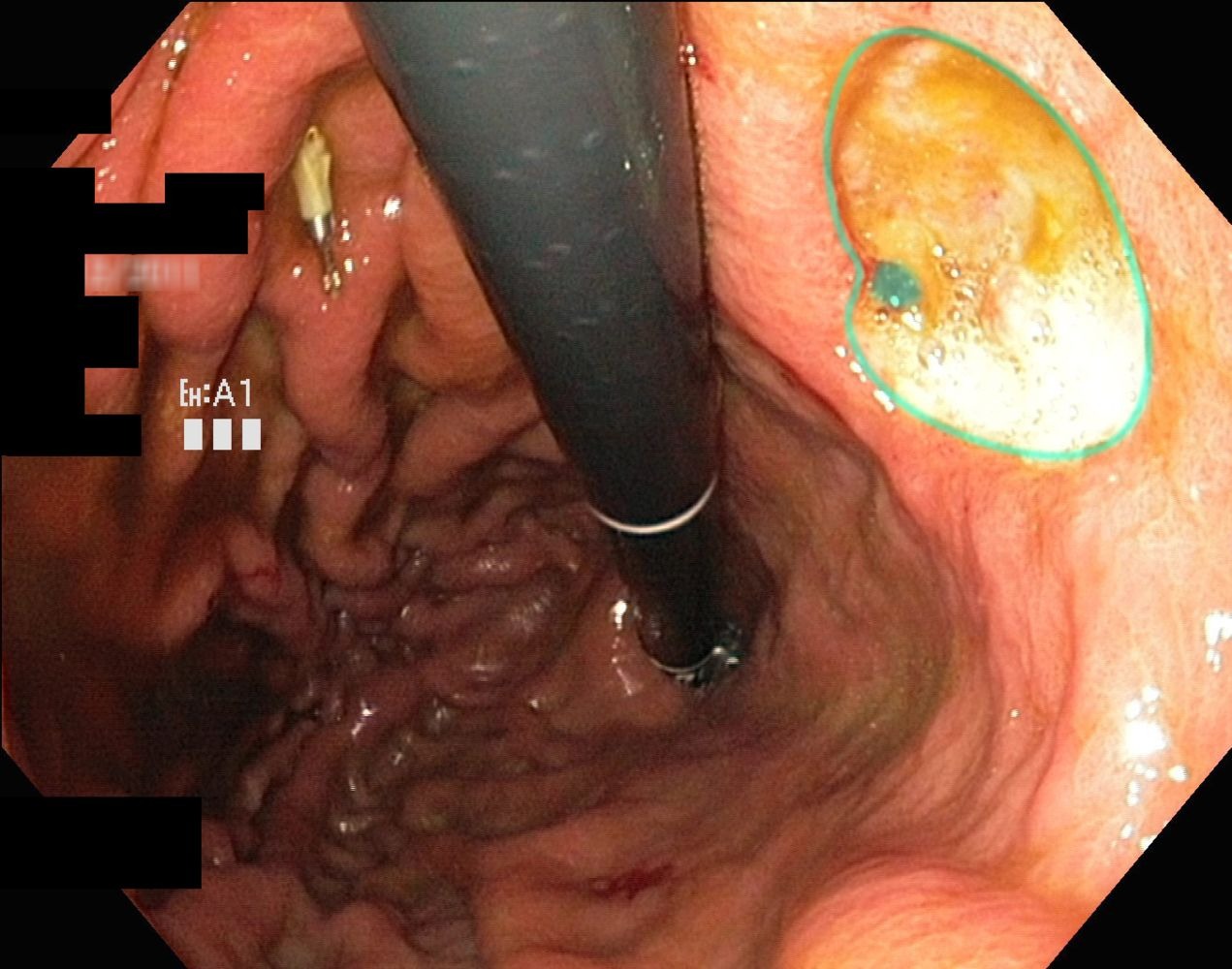
- ★ Gold standard: EGD with biopsy
- Direct visualization
- Biopsy for H. pylori and malignancy
- Therapeutic intervention if bleeding
- H. pylori testing:
- Non-invasive:
- ★ Urea breath test (95% sensitive/specific)
- ★ Stool antigen test (>90% sensitive/specific)
- Serology (not for active infection)
- Invasive (during EGD):
- ★ Rapid urease test (CLOtest)
- Histology
- Culture (for antibiotic resistance)
- Non-invasive:
- Other tests:
- Serum gastrin: If Zollinger-Ellison suspected (>1000 pg/mL)
- CXR/CT: Free air under diaphragm if perforation
EGD Findings
| EGD Finding | Probable Cause | Action |
| Multiple shallow ulcers | ★ NSAIDs | Stop NSAIDs, PPI therapy |
| Large ulcer with heaped margins | ★ Malignancy | Multiple biopsies (6-8) |
| Single deep ulcer | H. pylori | Biopsy, triple therapy |
| Multiple ulcers in jejunum | ★ Zollinger-Ellison syndrome | Check serum gastrin, CT/MRI for gastrinoma |
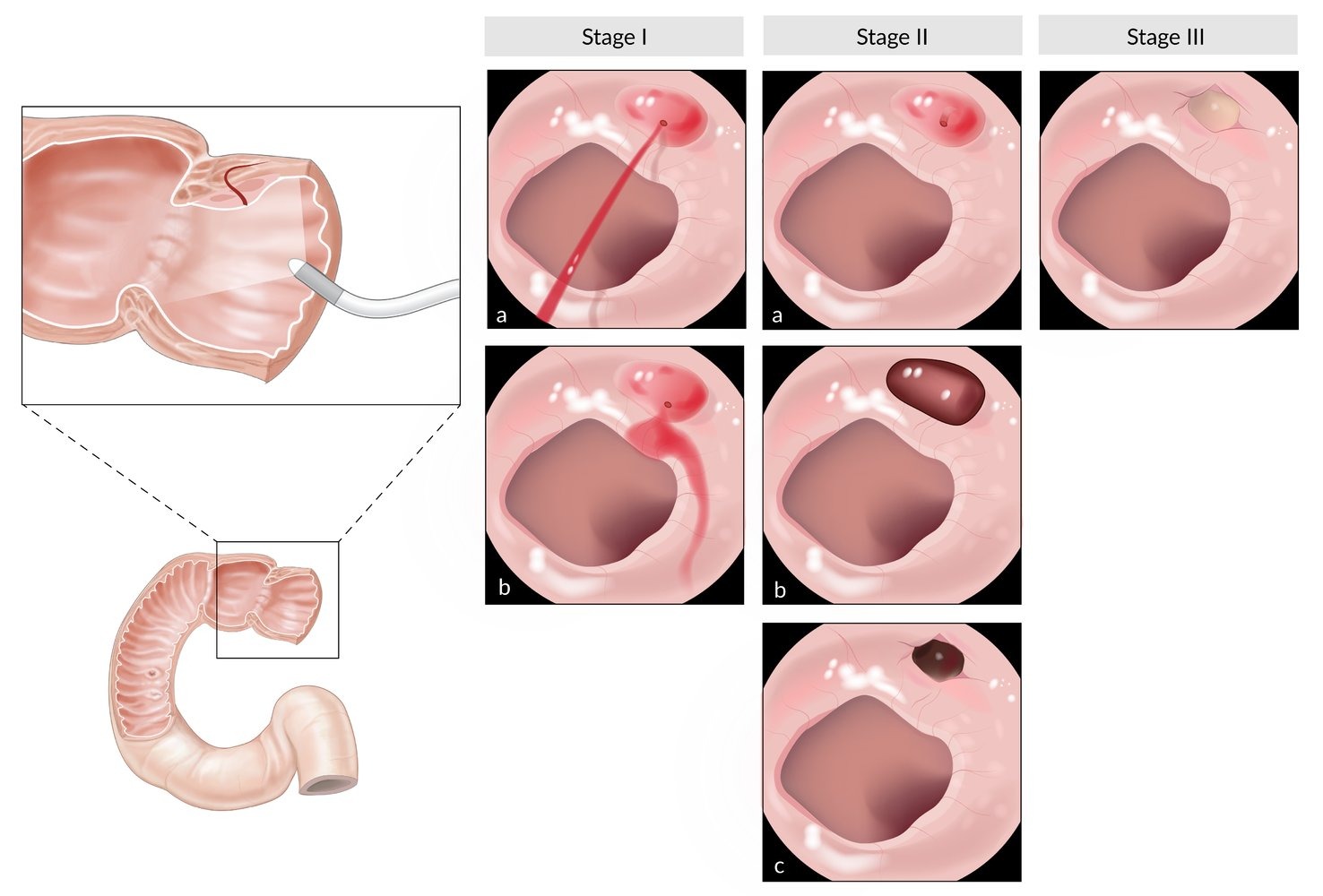
Forrest Classification (Upper GI Hemorrhage)
| Stage | Description | Rebleeding Risk | Management |
| Ia | ★ Spurting arterial hemorrhage | 90% | Urgent endoscopic therapy |
| Ib | Oozing hemorrhage | 50% | Endoscopic therapy |
| IIa | ★ Visible vessel (non-bleeding) | 40-50% | Endoscopic therapy |
| IIb | Adherent clot | 20-30% | Consider endoscopic therapy |
| IIc | Flat pigmented spot (hematin) | 10% | Medical therapy only |
| III | ★ Clean base | <5% | Medical therapy only |
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Differential diagnosis
- Gastric malignancy (confirmed by biopsy)
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Differential Diagnosis - v2
| Condition | Key Distinguishing Features | Test to Differentiate | Classic Patient |
| GERD |
|
24-hour pH monitoring | Obese patient with heartburn after large meals |
| Gastric cancer |
|
EGD with biopsy | Elderly Asian male with new dyspepsia |
| Chronic pancreatitis |
|
CT scan, fecal elastase | Alcoholic with recurrent epigastric pain |
| Biliary colic |
|
RUQ ultrasound | Obese female with RUQ pain after fatty meal |
| Functional dyspepsia |
|
Diagnosis of exclusion | Young woman with chronic symptoms, normal workup |
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Treatment
- Conservative management
- Smoking and alcohol cessation
- Stop NSAIDs
- Proton pump inhibitor
- Triple therapy for helicobacter pylori
Algorithm for treatment following biopsy A biopsy shows signs of NSAIDs use - Stop NSAIDs
A biopsy shows cancer - Stage and treat accordingly
A biopsy shows H. Pylori - Triple therapy
- Surgical management
- Selective vagotomy
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Treatment - v2
Medical Management
★ FIRST-LINE TREATMENT ALGORITHMS:
1. H. pylori-positive PUD:
1. H. pylori-positive PUD:
- Triple therapy (14 days):
- PPI (omeprazole 20mg BID or equivalent)
- Clarithromycin 500mg BID
- Amoxicillin 1g BID (or metronidazole 500mg BID if PCN allergy)
- Quadruple therapy (if clarithromycin resistance >15%):
- PPI BID
- Bismuth subsalicylate 525mg QID
- Metronidazole 250mg QID
- Tetracycline 500mg QID
2. NSAID-induced PUD:
- ★ Discontinue NSAIDs (most important)
- PPI therapy for 8 weeks
- If NSAID must continue: PPI prophylaxis indefinitely
3. H. pylori-negative, NSAID-negative PUD:
- PPI therapy for 4-8 weeks
- Investigate for rare causes (Zollinger-Ellison, Crohn's)
PPI Dosing (Equivalents)
- Omeprazole: 20-40mg daily
- Esomeprazole: 20-40mg daily
- Lansoprazole: 15-30mg daily
- Pantoprazole: 40mg daily
- Rabeprazole: 20mg daily
Surgical Management
Indications (rare in PPI era):
- ★ Perforation
- Uncontrolled bleeding despite endoscopic therapy
- Gastric outlet obstruction
- Refractory ulcers (rule out malignancy)
Procedures:
- Perforation: Graham patch (omental patch)
- Bleeding: Oversewing of vessel ± vagotomy
- Obstruction: Gastrojejunostomy or pyloroplasty
- Refractory: Selective vagotomy + drainage
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Complications
| Ulcer complications | |
| Haemorrhage |
|
| Obstruction |
|
| Perforation |
|
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Complications - v2
| ⚠️ COMPLICATIONS OF PUD | |
| Hemorrhage (15%) |
|
| Perforation (5%) |
|
| Penetration (rare) |
|
| Obstruction (2%) |
|
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
HIGH-YIELD FACTS BOX - v2
- ★ Most common cause overall: H. pylori infection (90% of duodenal ulcers, 70% of gastric ulcers)
- ★ Second most common cause: NSAIDs
- ★ Classic presentation: Epigastric burning pain
- ★ Best initial test: Urea breath test or stool antigen (for H. pylori)
- ★ Most accurate test: EGD with biopsy
- ★ First-line treatment: Triple therapy (PPI + clarithromycin + amoxicillin)
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Memory Aids & Mnemonics - v2
📚 HIGH-YIELD MEMORY AIDS:
1. "GUDA" - Gastric vs Duodenal Ulcers:
1. "GUDA" - Gastric vs Duodenal Ulcers:
- Gastric = Greater with meals (pain)
- Ulcer
- Duodenal = Decreases with meals (pain)
- Also occurs at night (duodenal)
2. "NSAID" - Complications of NSAIDs:
- Nephropathy
- Stomach ulcers
- Asthma exacerbation
- Interstitial nephritis
- Dyspepsia
3. Alarm symptoms = "VBAD NEWS":
- Vomiting (persistent)
- Bleeding/Black stools
- Anemia
- Dysphagia
- New onset >55 years
- Early satiety
- Weight loss
- Swallowing difficulty
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Clinical Pearls - v2
💡PEARLS:
- ★ Duodenal ulcers almost never malignant (<0.5%) - biopsy not routine
- ★ Gastric ulcers require biopsy - 3-5% are malignant
- ★ Pain relief with antacids suggests PUD but doesn't differentiate gastric from duodenal
- ★ NSAIDs can cause ulcers without H. pylori
- ★ Stop PPI 2 weeks before H. pylori testing to avoid false negatives
- ★ Posterior duodenal ulcers → hemorrhage; Anterior → perforation
- ★ Zollinger-Ellison: Think when ulcers in unusual locations (jejunum) or multiple ulcers
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Quick Review Box -v2
✅ MUST-KNOW FOR EXAMS:
- Most common cause of PUD: H. pylori (90% duodenal, 70% gastric)
- Classic duodenal ulcer: Young male, pain relieved by food, nocturnal pain
- Classic gastric ulcer: Elderly, pain worsened by food, weight loss
- Best initial H. pylori test: Urea breath test or stool antigen
- Triple therapy: PPI + clarithromycin + amoxicillin × 14 days
- Most common complication: Hemorrhage (gastroduodenal artery for duodenal)
- Perforation sign: Free air under diaphragm on CXR
- Always biopsy: Gastric ulcers (malignancy risk 3-5%)
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.
فيديوهات الشرح
بطاقات تفاعلية
أسئلة ممارسة
اشترك الآن