-
Definition: Inflammatory Bowel Disease (IBD) is an idiopathic, chronic inflammatory disorder of the gastrointestinal tract. It is primarily composed of two conditions:
- Ulcerative Colitis (UC)
- Crohn’s Disease (CD)
-
Pathophysiology: IBD arises from a dysregulated immune response to intestinal microflora in genetically susceptible individuals. Three key factors drive IBD pathogenesis:
- Genetic predisposition
- Altered (dysregulated) immune response
- Abnormal response to gut microorganisms
-
Extraintestinal Manifestations: UC and CD share many common extraintestinal manifestations, including musculoskeletal (e.g., arthritis), ocular (e.g., uveitis, episcleritis), and dermatologic (e.g., erythema nodosum, pyoderma gangrenosum) findings.
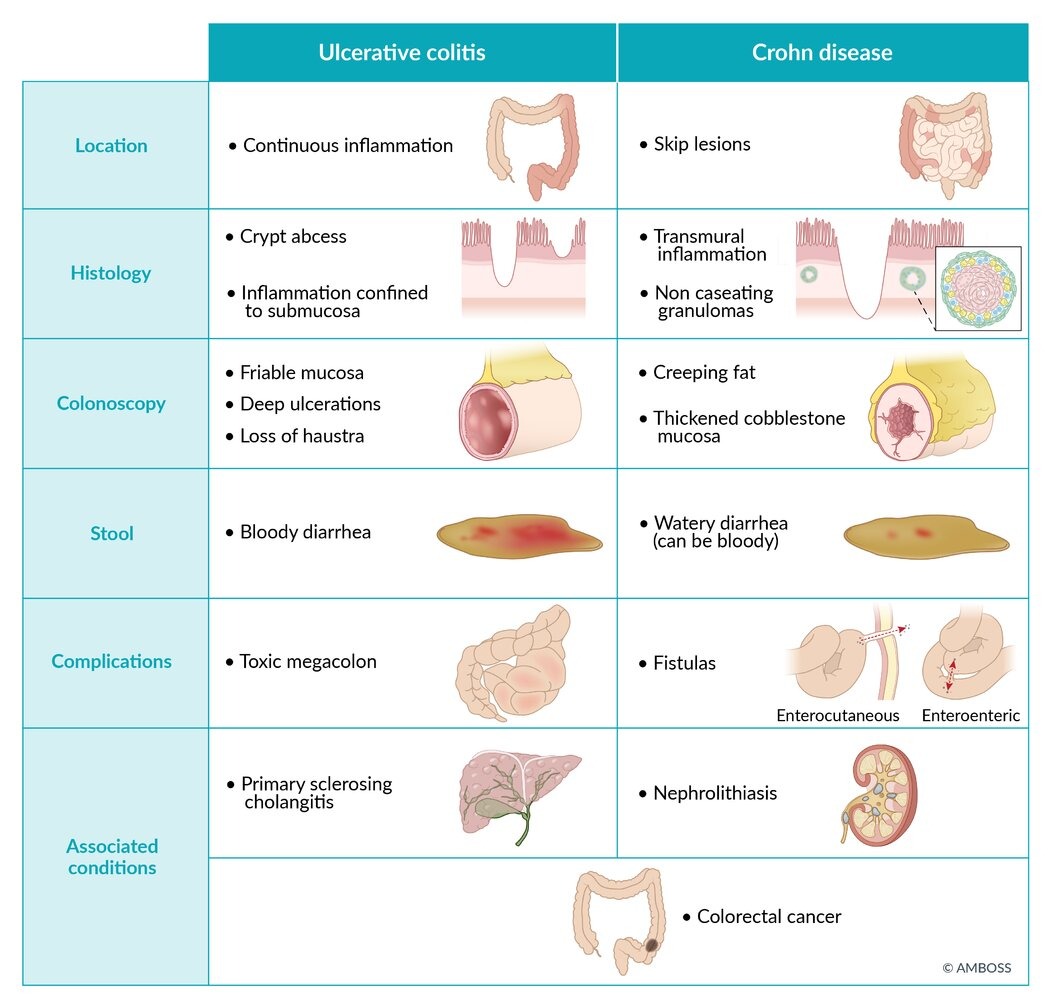
Comparison: Ulcerative Colitis vs. Crohn’s Disease
| Ulcerative Colitis | Crohn’s Disease | |
| Incidence |
|
|
| Involvement |
|
|
| Endoscopy |
|
|
| Microscopy |
|
|
| Clinical Presentation |
|
|
| Risk of Malignancy |
|
|
| Intestinal Complications |
|
|
| Mutual Extraintestinal Manifestations |
|
|
| Role of Surgery |
|
|
Ulcerative Colitis
Background and Pathophysiology
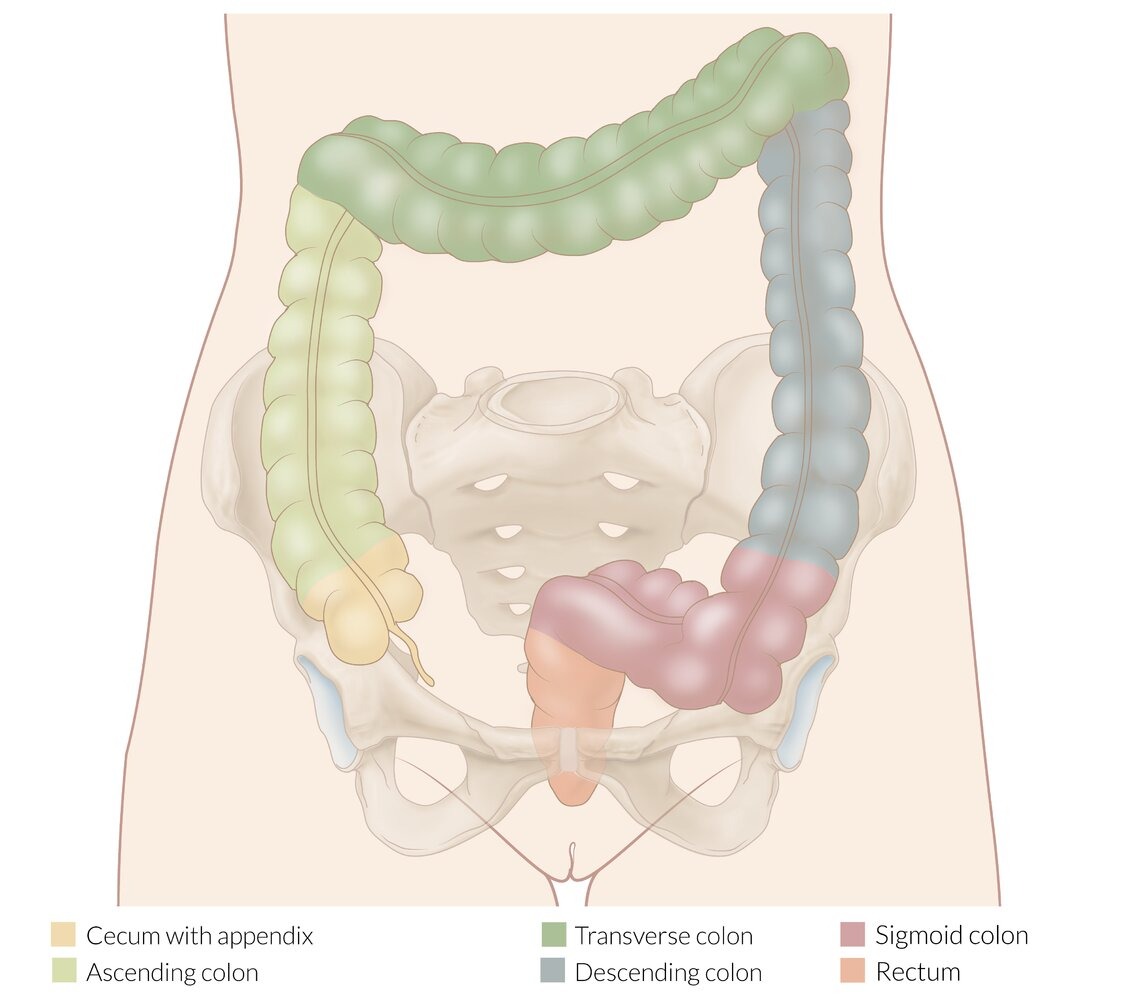
- Chronic inflammatory disease of the colon and rectum
- Inflammation is limited to the mucosa and submucosa
Clinical Findings
- GI symptoms: Bloody diarrhea, abdominal pain, tenesmus, urgency
- Systemic signs: Weight loss, fever
Laboratory Findings
- Leukocytosis
- Iron deficiency anemia
- Reactive thrombocytosis
- Elevated inflammatory markers (e.g., CRP, ESR)
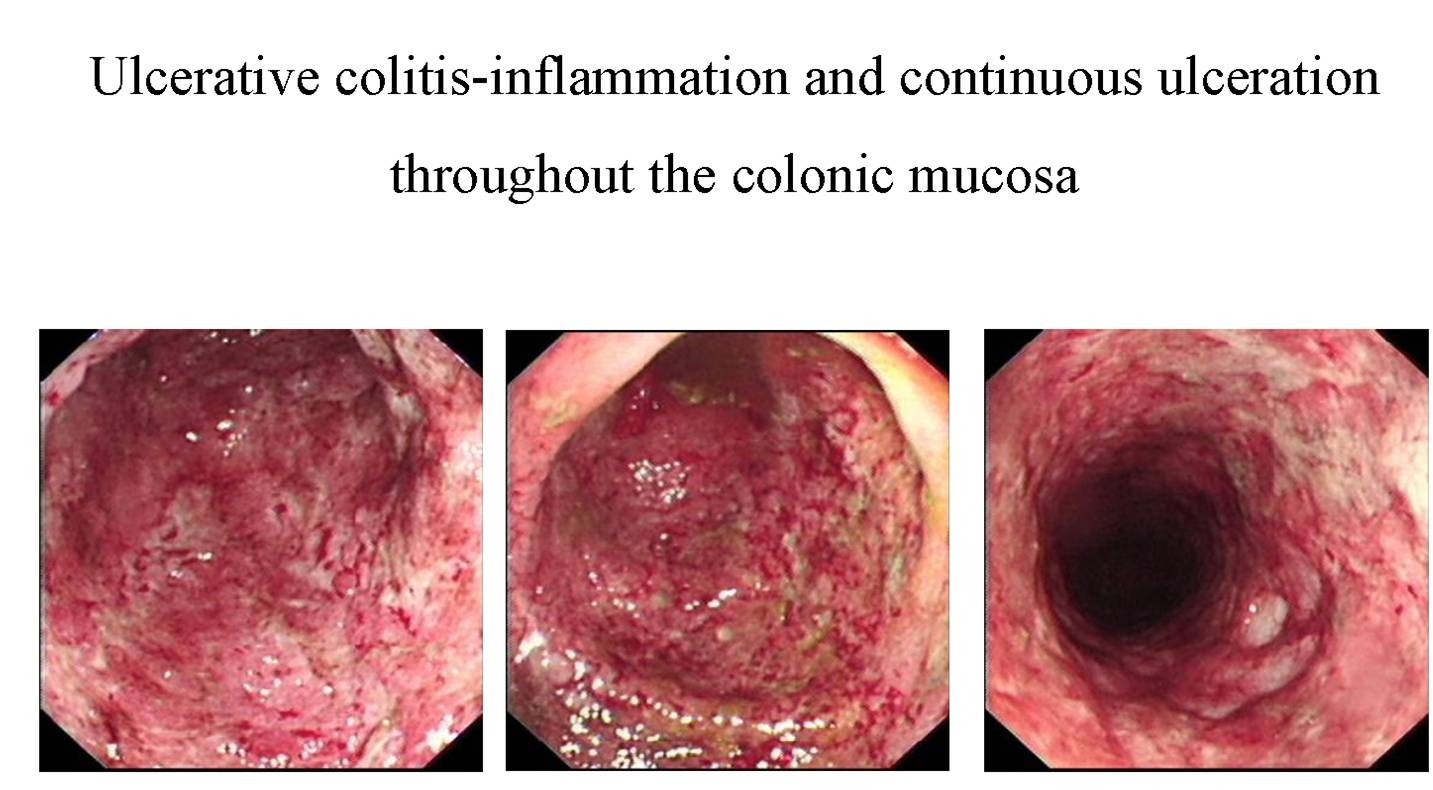
Endoscopy
- Continuous colonic involvement, always including the rectum
- Erythematous, friable mucosa
- Pseudopolyps (areas of regenerating mucosa surrounded by ulceration)
Biopsy
- Mucosal and submucosal inflammation
- Crypt abscesses, crypt distortion
Complications
- Toxic megacolon (risk increases with severe disease)
- Primary sclerosing cholangitis
- Colorectal cancer (risk increases with disease duration and severity)
- Extraintestinal manifestations (e.g., erythema nodosum, pyoderma gangrenosum, spondyloarthritis)
Management
- 5-Aminosalicylic acid (5-ASA) agents (e.g., mesalamine, sulfasalazine)
- Corticosteroids for acute flares
- Immunomodulators (e.g., azathioprine)
- Biologics (e.g., anti-TNF agents) in moderate-to-severe disease
- Colectomy is curative
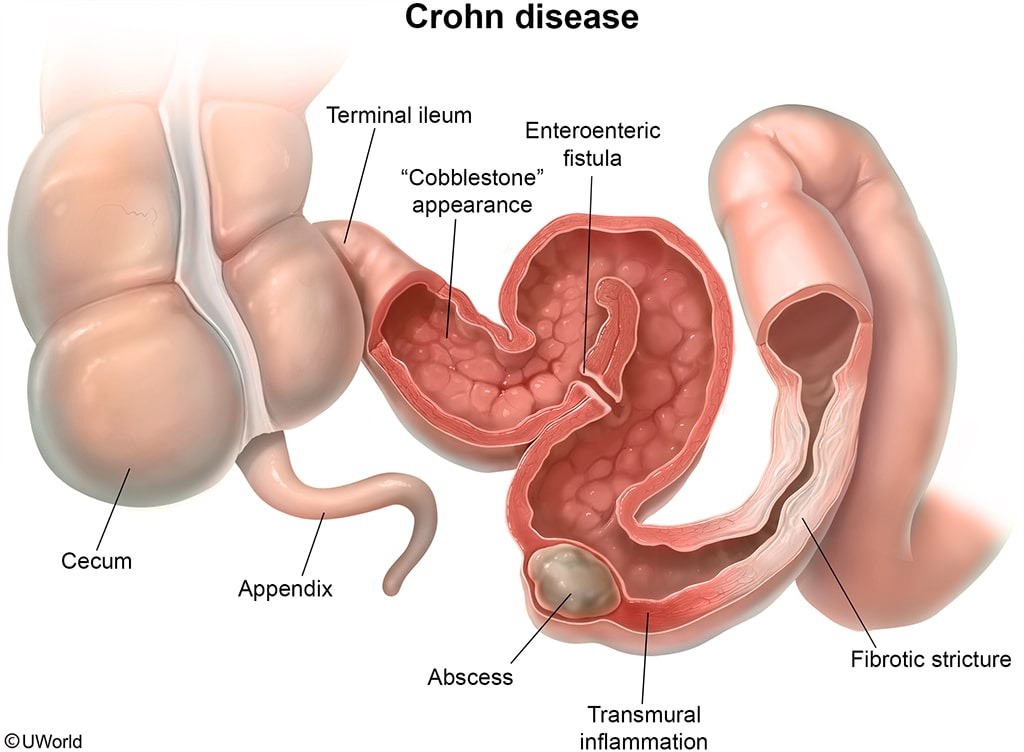
Crohn’s Disease
Background and Pathophysiology
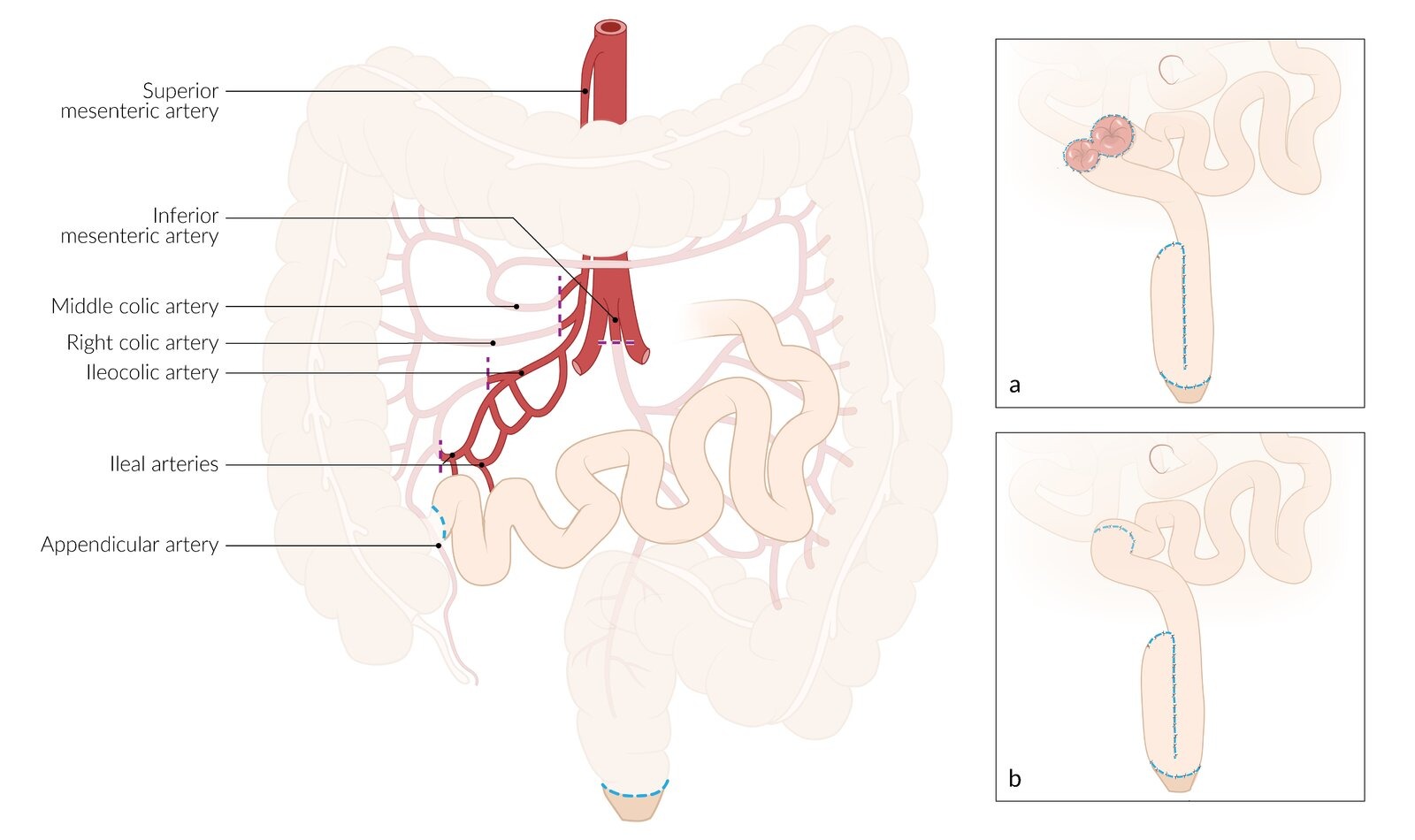
- Chronic, transmural inflammation that may affect any part of the GI tract (mouth to anus)
- Skip lesions and noncaseating granulomas are characteristic
Clinical Findings
- GI symptoms: Abdominal pain, diarrhea (often watery, can be bloody), oral ulcers, malabsorption, weight loss
- Complications: Fistulas (enteroenteric, cutaneous, vesical), strictures, abscess formation
- Extraintestinal manifestations: Arthritis, uveitis, erythema nodosum, pyoderma gangrenosum
Diagnosis
- Laboratory Tests: Leukocytosis, iron deficiency anemia, elevated inflammatory markers (CRP, ESR)
- Endoscopy: “Cobblestone” appearance with skip lesions
- Radiography/CT: Bowel wall thickening, strictures
Management
- Medical therapy:
- 5-ASA agents (mild disease)
- Corticosteroids (acute flares)
- Immunomodulators (azathioprine)
- Anti-TNF therapies (moderate-to-severe disease)
- Lifestyle: Smoking cessation is crucial as smoking exacerbates Crohn’s Disease
- Surgery: Reserved for complications (e.g., fistulas, strictures), not curative
Additional Complications
- Gallstones due to decreased enterohepatic circulation of bile acids
- Bile salt diarrhea with terminal ileal disease
- Nephrolithiasis (calcium oxalate stones) due to hyperoxaluria
Differential Diagnosis: Irritable Bowel Syndrome (IBS)
Overview
- Functional disorder characterized by abdominal pain and altered bowel habits without a clear structural abnormality
Rome IV Diagnostic Criteria
- Recurrent abdominal pain/discomfort at least 1 day/week for the past 3 months with ≥2 of the following:
- Related to defecation (improvement or worsening)
- Change in stool frequency
- Change in stool form (appearance)
Classifications
- Diarrhea predominant (IBS-D)
- Constipation predominant (IBS-C)
- Mixed type (IBS-M)
Colonoscopy Findings
- Typically normal mucosa; no structural lesions
Diagnosis
- Previously considered a diagnosis of exclusion, but in patients who fulfill Rome IV criteria and lack alarming features (e.g., significant weight loss, GI bleeding, family history of IBD or colon cancer), extensive workup is often not required.
Management
- Lifestyle modification (diet, exercise, stress management)
- Low FODMAP diet (fermentable oligosaccharides, disaccharides, monosaccharides, polyols)
- Symptomatic relief: Loperamide (for diarrhea), laxatives or fiber (for constipation)
- Alarm features (e.g., older age of onset >50, nocturnal diarrhea, iron deficiency anemia) warrant further investigation.
Associations
- Fibromyalgia
- Mood disorders (anxiety, depression)
| Clinical Features of Irritable Bowel Syndrome | |
| Rome IV Diagnostic Criteria |
|
| Classifications |
|
| Colonoscopy Findings |
|
| Diagnosis |
|
| Management |
|
| Alarm Features |
|
| Associations |
|
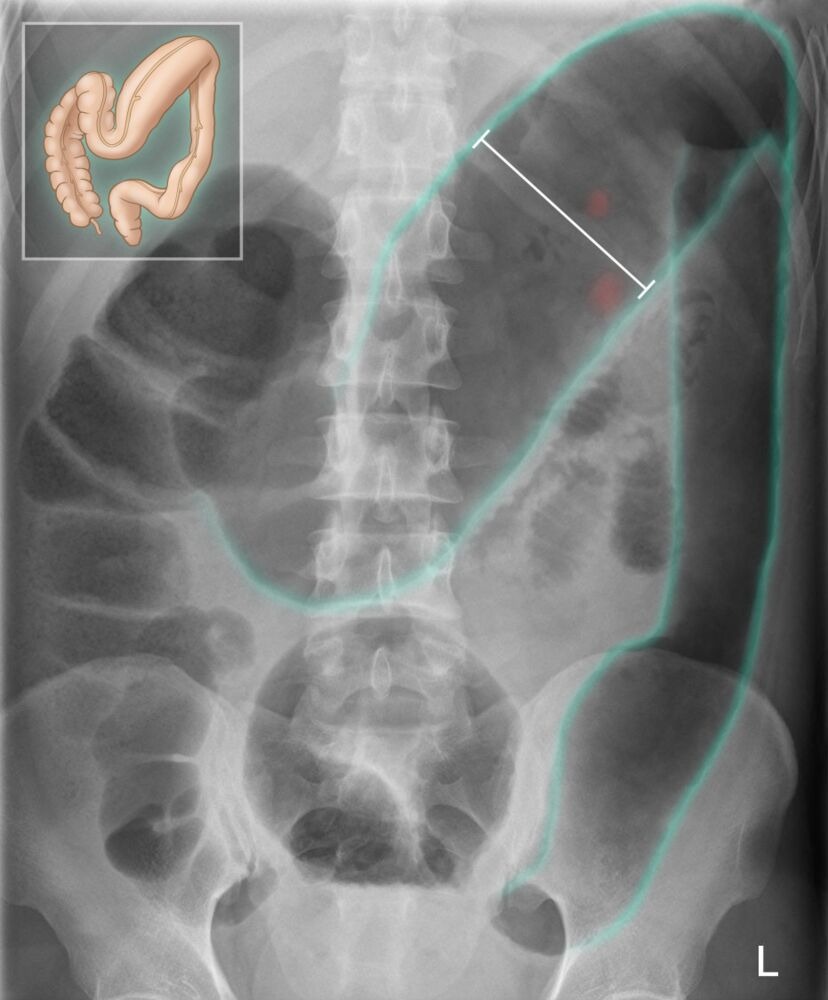
Key Complication: Toxic Megacolon
Etiology
- Extreme colonic distention (>6 cm dilation in the right colon or >9 cm in the cecum) due to inflammation involving the smooth muscle layer, causing paralysis and dilation.
- Most commonly associated with:
- Ulcerative colitis
- Crohn’s disease
- Infectious colitis (C. difficile)
- Ischemic colitis
- Obstructive colon cancer or volvulus
Clinical Presentation
- Systemic toxicity (fever, tachycardia, hypotension)
- Bloody diarrhea
- Abdominal distention, signs of peritonitis
Diagnosis
- Plain X-ray or CT scan showing marked colonic dilation, loss of haustra, and possible mucosal ulceration
Management
- Conservative: Bowel rest, NG suction if ileus is present, IV corticosteroids, antibiotics
- Surgery: Indicated if no improvement within 72 hours or in cases of perforation
Note: Barium enema is contraindicated due to the risk of perforation.
| Toxic Megacolon | |
| Etiology |
|
| Risk Factors |
|
| Clinical Presentation |
|
| Diagnosis |
|
| Management |
|

Pyoderma Gangrenosum
Clinical Features
- Begins as a small papule or pustule
- Rapidly progresses to a painful ulcer with a purulent base and a violaceous border
- Pathergy phenomenon: minor trauma can precipitate new ulceration
Epidemiology
- Peak onset age 40–60
- More common in women
- Strong association with IBD, rheumatoid arthritis, and malignancies
Diagnosis
- Clinical exclusion of other ulcerative conditions (e.g., infections)
- Biopsy: Neutrophilic infiltrates without pathogenic organisms
Treatment
- Local or systemic glucocorticoids (mainstay)
- Adjunctive immunosuppressants in refractory cases
| Pyoderma Gangrenosum | |
| Clinical Features |
|
| Epidemiology |
|
| Diagnosis |
|
| Treatment |
|

احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.