Background
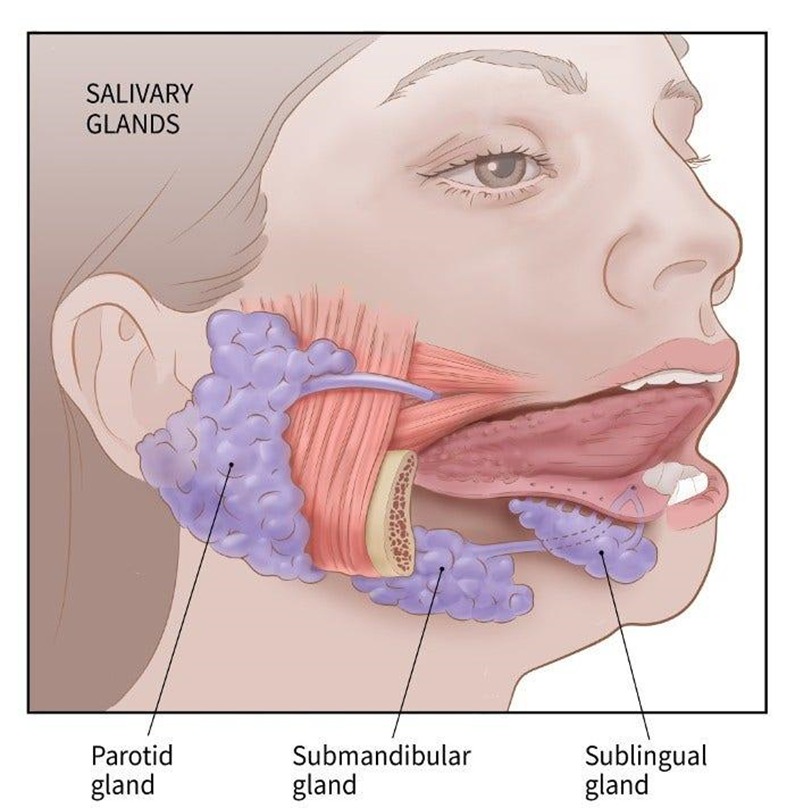
- Salivary gland cancers make up 6% of all head and neck tumors
- Most commonly arise in the parotid gland (80%)
- Among salivary gland neoplasms, 10-15% arise in the submandibular glands
- These tumors present usually in the 6th decade of life
- Salivary gland cancers are mostly benign
- Submandibular, sublingual and minor salivary gland tumors are more likely to be malignant
Version 2
Definition
Neoplasms arising from the major (parotid, submandibular, sublingual) or minor salivary glands, ranging from benign to malignant.
Epidemiology
- Incidence: 3-6% of all head and neck tumors
- Age: Peak incidence in 6th-7th decade
- Gender: Slight female predominance for benign tumors; equal distribution for malignant
- ★ Most common site: Parotid gland (80% of all salivary tumors)
- ★ Rule of 80s:
- 80% of salivary tumors occur in parotid
- 80% of parotid tumors are benign
- 80% of benign parotid tumors are pleomorphic adenomas
Risk Factors
- Radiation exposure (latency period: 15-20 years)
- Prior head/neck radiation therapy
- Occupational exposure (rubber manufacturing, hairdressing)
- Viral infections (EBV, HIV)
- Genetic syndromes (Li-Fraumeni)
Types
| Salivary gland tumor | Notes |
| Pleomorphic adenoma (benign mixed tumor) |
|
| Warthin’s tumor (papillary cystadenoma lymphoatosum) |
|
| Mucoepidermoid carcinoma |
|
Version 2
| Tumor Type | Frequency | Demographics | Key Features | Malignant Potential |
|---|---|---|---|---|
| ★ Pleomorphic adenoma (Benign mixed tumor) |
50-60% of parotid tumors ★ MOST COMMON overall |
F > M 30-50 years |
• Painless, slow-growing • Mobile mass • Chondromyxoid stroma + epithelium • "Rubbery" consistency |
• 2-5% malignant transformation • Risk ↑ with time • Carcinoma ex pleomorphic adenoma |
| Warthin tumor (Papillary cystadenoma lymphomatosum) |
5-10% of parotid tumors ★ 2nd most common benign |
M > F (4:1) 50-70 years ★ Smokers |
• Often bilateral (10-15%) • Cystic with germinal centers • "Hot" on technetium scan • Tail of parotid |
Virtually never malignant |
| ★ Mucoepidermoid carcinoma | 30% of malignant ★ MOST COMMON malignant |
Any age ★ Most common in children |
• Low/intermediate/high grade • Mucinous + squamous cells • t(11;19) translocation • Painful if high-grade |
Malignant by definition Grade determines prognosis |
| Adenoid cystic carcinoma | 10% of malignant ★ 2nd most common malignant |
40-60 years F = M |
• ★ "Swiss cheese" pattern • ★ Perineural invasion+++ • Slow but relentless growth • Late distant mets (lung) |
Highly malignant Poor long-term prognosis |
| Acinic cell carcinoma | 5-10% of malignant | 40-50 years F > M |
• Bilateral in 3% • Serous acinar cells • Usually low-grade |
Malignant Generally good prognosis |
Note
⚠️ HIGH-YIELD RULE: Location vs Malignancy Risk
ملاحظة
Clinical features
- Symptoms
- Solitary, mobile slow growing painless mass (may be present for many years)
- Dysphagia and hoarseness
- Difficult chewing
- Physical exam
- Painless, mobile mass found at the angle of the jaw (usually pleomorphic adenoma)
- Disturbance to facial nerve function (most commonly associated with invasive malignancy)
Version 2
Classic Presentation
**Malignant tumor**: Rapidly growing, fixed mass with pain and facial nerve involvement
Symptoms (in order of frequency)
- Palpable mass (>90%)
- Pain (suggests malignancy or infection)
- Facial nerve palsy
- Dysphagia/hoarseness (deep lobe involvement)
- Trismus (advanced disease)
Physical Examination Findings
- Benign features:
- Mobile, well-circumscribed
- Soft to rubbery consistency
- No facial nerve involvement
- No skin changes
- ★ Malignant features (RED FLAGS):
- Fixed to deep structures
- Hard consistency
- Facial nerve palsy (25% of malignant)
- Skin ulceration
- Cervical lymphadenopathy
- Rapid growth (doubling <6 months)
Diagnosis
- Imaging
- Ultrasound (hypoechoic mass)
- CT/MRI (necrosis or calcification can be visualized)
- Serum labs
- Fine needle aspiration (to assess for malignancy)
Diagnostic Algorithm
Laboratory Studies
- Fine Needle Aspiration (FNA):
- Sensitivity: 85-95%
- Specificity: 95-98%
- ★ Cannot distinguish follicular lesions
- Core needle biopsy if FNA non-diagnostic
Imaging Studies
- Ultrasound:
- First-line imaging
- Guides FNA
- Hypoechoic = suspicious
- MRI (preferred over CT):
- Best for deep lobe tumors
- Perineural spread assessment
- T1: intermediate signal
- T2: high signal (most tumors)
- CT scan:
- Stone detection (sialolithiasis)
- Bone involvement
- ★ Technetium-99m scan:
- "Hot" = Warthin tumor
- "Cold" = most others
Differential diagnosis
- Facial nerve schwannoma
Version 2
| Condition | Key Distinguishing Feature | Test to Differentiate |
|---|---|---|
| Lymphoma | B symptoms, multiple nodes | Flow cytometry |
| Metastasis | Known primary cancer | PET-CT |
| Sialolithiasis | Meal-related swelling | CT or sialography |
| Sjögren syndrome | Bilateral, dry eyes/mouth | Anti-SSA/SSB |
| HIV parotitis | Bilateral, cystic | HIV testing |
Treatment
- Surgical management
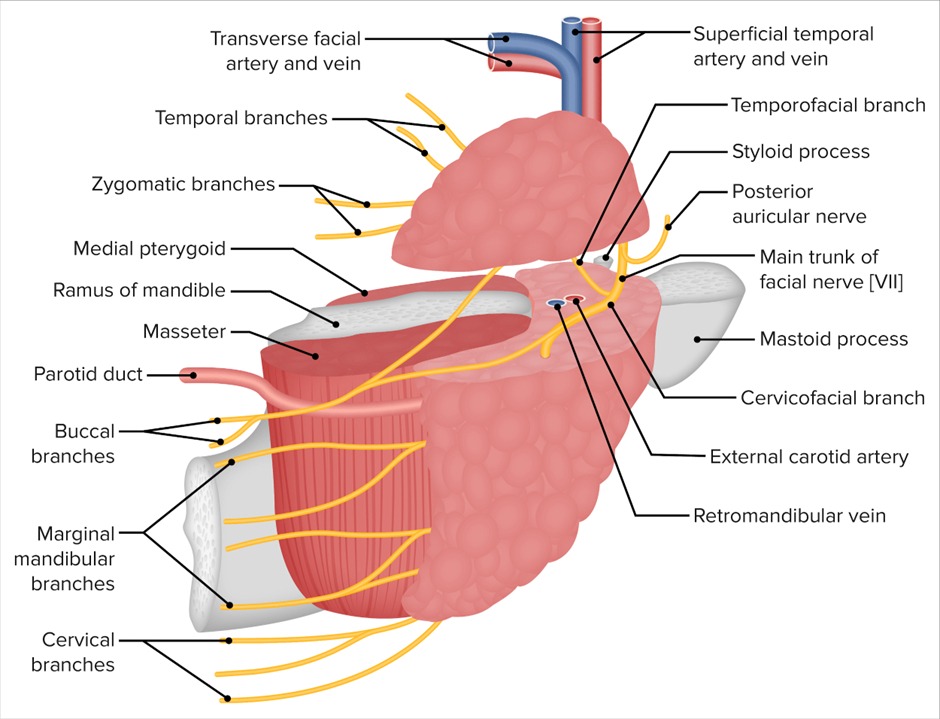
- Superficial or total parotidectomy (pleomorphic adenoma of the parotid gland)
- Tumor excision with preservation of nerve (pleomorphic adenoma of the submandibular and minor salivary glands)
Version 2
First-Line Treatment
**Malignant tumors**: Surgery + adjuvant radiation therapy
Surgical Management
- Parotid tumors:
- Superficial parotidectomy (lateral to facial nerve)
- Total parotidectomy (if deep lobe involved)
- ★ Facial nerve preservation unless invaded
- Submandibular tumors:
- Excision of entire gland
- Level I-II neck dissection if malignant
- Minor salivary gland tumors:
- Wide local excision
- Site-specific approach
Surgical complications
- Recurrence after resection
- Malignant transformation
Version 2
Most Common Complications
- ★ Frey syndrome (gustatory sweating)
- Incidence: 30-50% post-parotidectomy
- Aberrant parasympathetic reinnervation
- Treatment: Botulinum toxin
- Facial nerve injury
- Temporary: 20-30%
- Permanent: <5% (if nerve preserved)
- First bite syndrome
- Severe pain with first bite
- Sympathetic denervation
Surgical Complications Timeline
- Immediate: Hematoma, nerve injury
- Early: Salivary fistula, infection
- Late: Frey syndrome, numbness
Prognostic Factors
- Favorable: Small size, low grade, parotid location
- Poor: High grade, facial nerve involvement, distant mets
HIGH-YIELD FACTS
Must-Know Facts for Exams:
1. Most common benign: Pleomorphic adenoma
2. Most common malignant: Mucoepidermoid carcinoma
3. Bilateral tumors: Think Warthin (smokers) or lymphoma
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.