سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Background
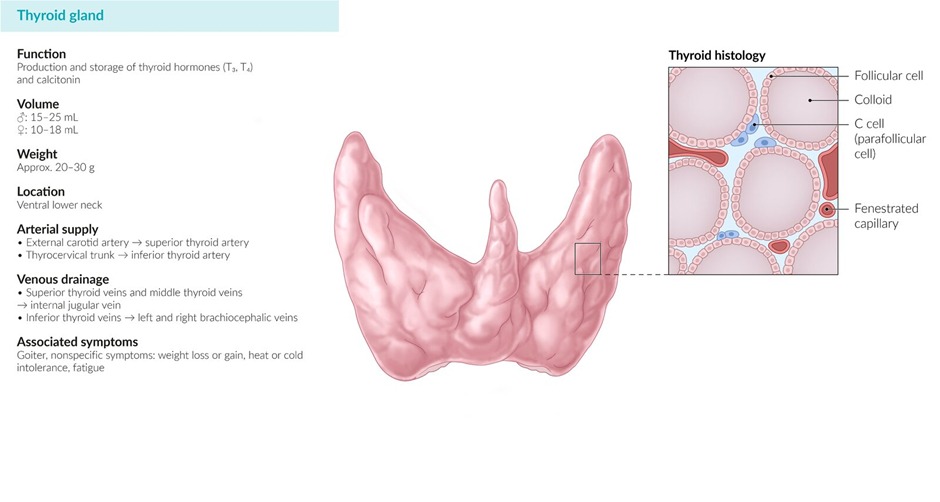
- Thyroid carcinomas are thyroid malignancies that can develop from the two cell types present in the thyroid gland (follicular and parafollicular cells)
- Thyroid carcinomas are more common in women (peaking in the third and fourth decades of life)
- Radiation exposure significantly increases the risk for malignancies arising from thyroid follicular cells; particularly papillary thyroid carcinoma
- Diagnosis is achieved through Fine needle aspiration (FNA) in most cases except in the case of follicular carcinoma
- Definitive management is achieved through thyroidectomy
Version 2
- Definition: Malignant tumors arising from thyroid follicular cells (papillary, follicular, anaplastic) or parafollicular C cells (medullary)
- Epidemiology:
- Incidence: ~13.5 cases per 100,000 per year
- Female predominance (3:1) for differentiated carcinomas
- Peak incidence: 30-50 years for papillary, 40-60 years for follicular
- Most common endocrine malignancy
- Risk factors:
- Radiation exposure (especially childhood) - strongest risk factor for papillary carcinoma
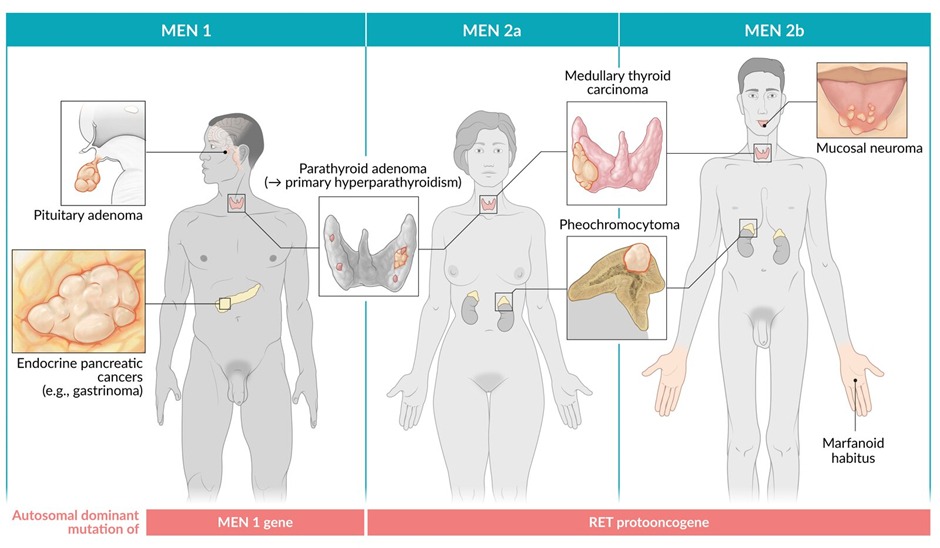
- Family history and genetic syndromes (MEN 2A/2B for medullary)
- Pre-existing thyroid disease (Hashimoto's for lymphoma)
- Female gender
- Prognosis varies by type: Papillary (>90% 5-year survival) to anaplastic (5-14% 5-year survival)
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Types
| Thyroid cancer | Notes |
| Papillary carcinoma |
|
| Follicular carcinoma |
|
| Medullary carcinoma |
|
| Anaplastic thyroid carcinoma |
|
| Lymphoma (typically diffuse large B-cell lymphoma) |
|
Version 2
| Type | Key Features |
| Papillary carcinoma |
|
| Follicular carcinoma |
|
| Medullary carcinoma |
|
| Anaplastic carcinoma |
|
| Primary thyroid lymphoma |
|
| Hürthle cell carcinoma |
|
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Clinical features
- Symptoms
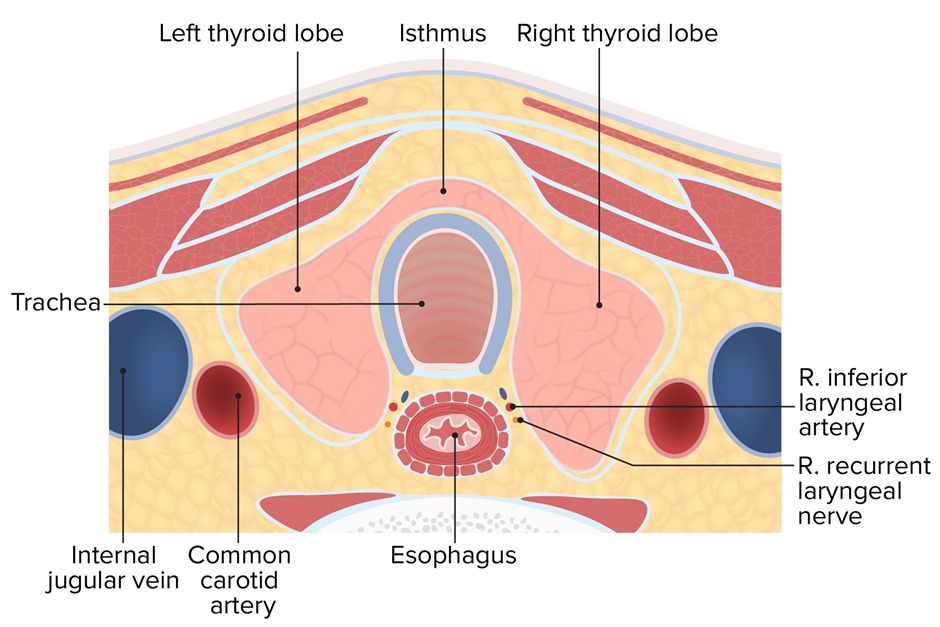
- Dysphagia and hoarseness (secondary to direct compression by the tumor)
- Physical exam
- Neck mass or palpable thyroid nodule (painless)
- Cervical lymphadenopathy might be present
Version 2
- Symptoms:
- Usually asymptomatic (incidental finding)
- Dysphagia (compression of esophagus)
- Hoarseness (recurrent laryngeal nerve involvement)
- Dyspnea (tracheal compression)
- Horner syndrome (rare - sympathetic chain involvement)
- Physical exam:
- Thyroid nodule: Firm to hard, fixed, painless
- Cervical lymphadenopathy (especially papillary)
- Pemberton sign (facial plethora with arm elevation - SVC obstruction)
- Red flags for malignancy:
- Fixed, hard nodule
- Rapid growth
- Associated lymphadenopathy
- Voice changes
- Age <20 or >60 years
- Male gender
- History of radiation exposure
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
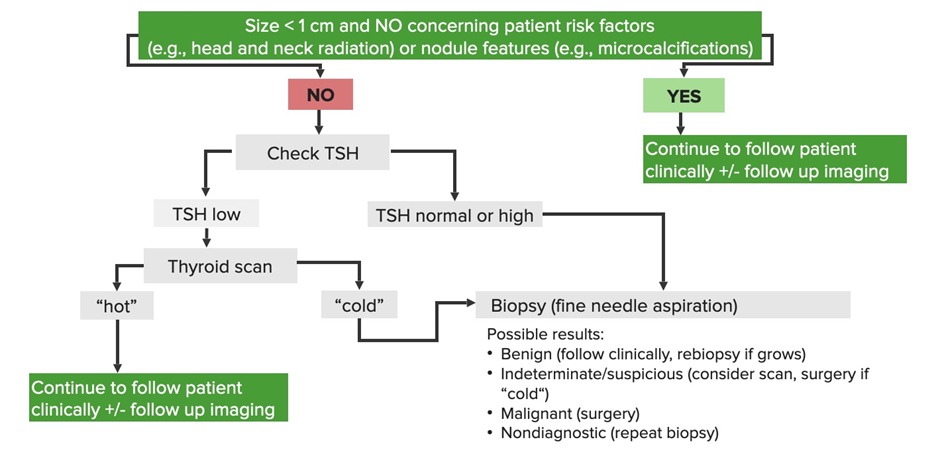
Diagnosis
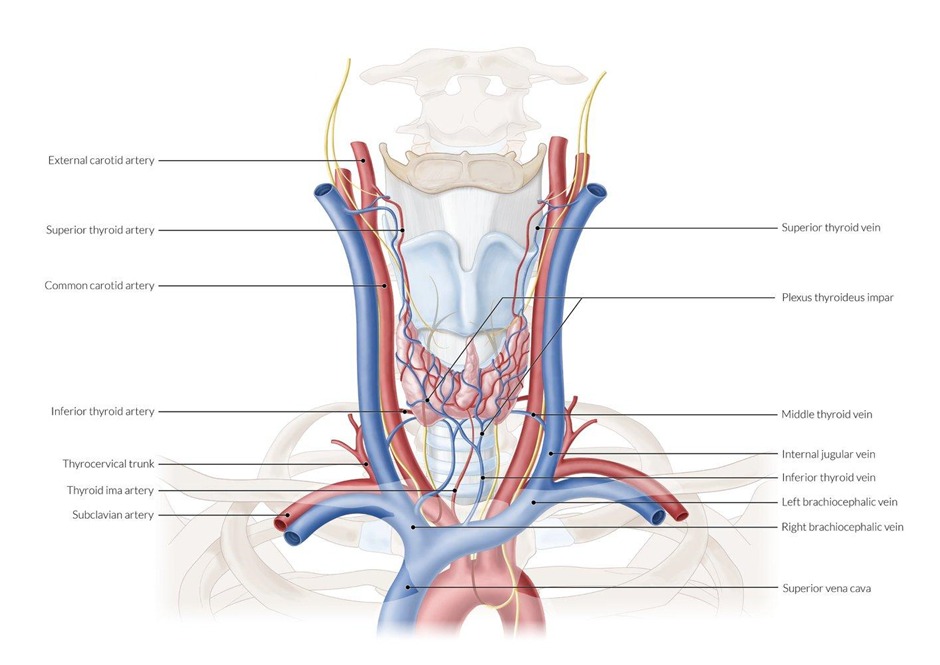
- Imaging
- Radioactive iodine uptake test
Radioactive Iodine Uptake Findings & Clinical Implications Hot thyroid nodules - Benign
- Do not require fine needle aspiration (FNA)
Cold thyroid nodules - Suspicion for malignancy
- Require fine needle aspiration (FNA)
- Ultrasonography (required for all thyroid nodules): hypoechoic lesions are concerning for malignancy
- Radioactive iodine uptake test
- Serum labs
- TSH levels (low TSH levels are more concerning for malignancy)
- Serum calcitonin (tumor marker for medullary thyroid cancer)
- Fine needle aspiration (FNA) is required for all cold nodules on radioactive iodine uptake scan
Version 2
- Initial evaluation:
- TSH: Usually normal; if low, perform radioiodine scan
- Thyroid ultrasound (all nodules):
- Suspicious features: Solid, hypoechoic, irregular margins, microcalcifications, taller than wide, extrathyroidal extension
- Radioiodine scintigraphy (if TSH low):
- Cold nodules: Higher malignancy risk → require FNA
- Hot nodules: Rarely malignant → usually no FNA needed
- Confirmatory test:
- Fine needle aspiration (FNA): Gold standard for diagnosis
- Exception: Cannot distinguish follicular adenoma from carcinoma
- Bethesda classification system for cytology reporting
- Fine needle aspiration (FNA): Gold standard for diagnosis
- Tumor markers:
- Thyroglobulin: For differentiated thyroid cancer (post-treatment monitoring)
- Calcitonin: For medullary carcinoma (diagnosis and monitoring)
- CEA: Additional marker for medullary carcinoma
- Staging: CT/MRI neck, chest imaging for metastases
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Differential diagnosis
- Benign thyroid nodule (typically a hot nodule on radioactive iodine uptake test)
Version 2
- Benign thyroid nodule (80-95% of all nodules)
- Thyroid cyst
- Multinodular goiter
- Thyroiditis (subacute, chronic)
- Riedel's thyroiditis (hard, fixed gland)
- Metastases to thyroid (rare)
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Treatment
- Medical management
- Iodine radiotherapy (possibly for cases of papillary thyroid cancer)
- Surgical management
- Thyroidectomy
Version 2
- Surgical management:
- Total thyroidectomy:
- Tumors ≥4 cm
- Extrathyroidal extension
- Nodal/distant metastases
- Medullary carcinoma
- Anaplastic carcinoma (if resectable)
- Hemithyroidectomy:
- Low-risk tumors <4 cm
- No extrathyroidal extension
- No metastases
- Neck dissection: As needed for nodal involvement
- Total thyroidectomy:
- Adjuvant therapy:
- Radioactive iodine ablation (RAI):
- For differentiated thyroid cancer post-thyroidectomy
- NOT effective for medullary or anaplastic carcinoma
- TSH suppression with levothyroxine:
- For differentiated thyroid cancer
- Target TSH based on risk stratification
- External beam radiation: For anaplastic or unresectable disease
- Chemotherapy: Limited role, mainly for anaplastic carcinoma
- Radioactive iodine ablation (RAI):
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Surgical complications
- Dysphagia and persistent hoarseness (due to injury to recurrent laryngeal nerve)
- Hypocalcemia (due to injury or removal of parathyroid glands)
- Loss of tenor; which is noticeable in professional voice users (due to injury to the external branch of the superior laryngeal nerve)
version 2
- Hypocalcemia (hypoparathyroidism from parathyroid injury/removal)
- Voice changes:
- Hoarseness (recurrent laryngeal nerve injury)
- Loss of vocal range (external branch of superior laryngeal nerve)
- Bleeding/hematoma
- Thyroid storm (rare)
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Supplementary tables
- Table 1: classification of multiple endocrine neoplasia
| Classification of multiple endocrine neoplasia | |
| Type 1 “the 3 P’s” |
|
| Type 2A |
|
| Type 2B |
|
Table: Multiple Endocrine Neoplasia (MEN) Syndromes
| MEN Type | Features |
| MEN 1 "3 P's" |
|
| MEN 2A |
|
| MEN 2B |
|
| Note | |
|
ملاحظة |
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.
فيديوهات الشرح
بطاقات تفاعلية
أسئلة ممارسة
اشترك الآن