Summary
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Introduction
- Intestinal atresia is the most common cause of obstruction in the neonatal period.
- Incidence is approximately 1 in 10,000 births (male predominance).
- Etiology is unknown but thought to occur during weeks 8-10 of development.
- This condition is associated with Down syndrome (20-30% of Down syndrome cases), and other birth anomalies.
- Intestinal Atresias include: Duodenal atresia, Jejunoileal atresia, and colonic atresia.
| Intestinal Atresias | |||
|---|---|---|---|
| Duodenal | Jejunum/Ileum | Colonic | |
| Pathophysiology |
|
|
|
| Clinical Findings |
|
|
|
| Associations |
|
|
|
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Duodenal Atresia
Introduction
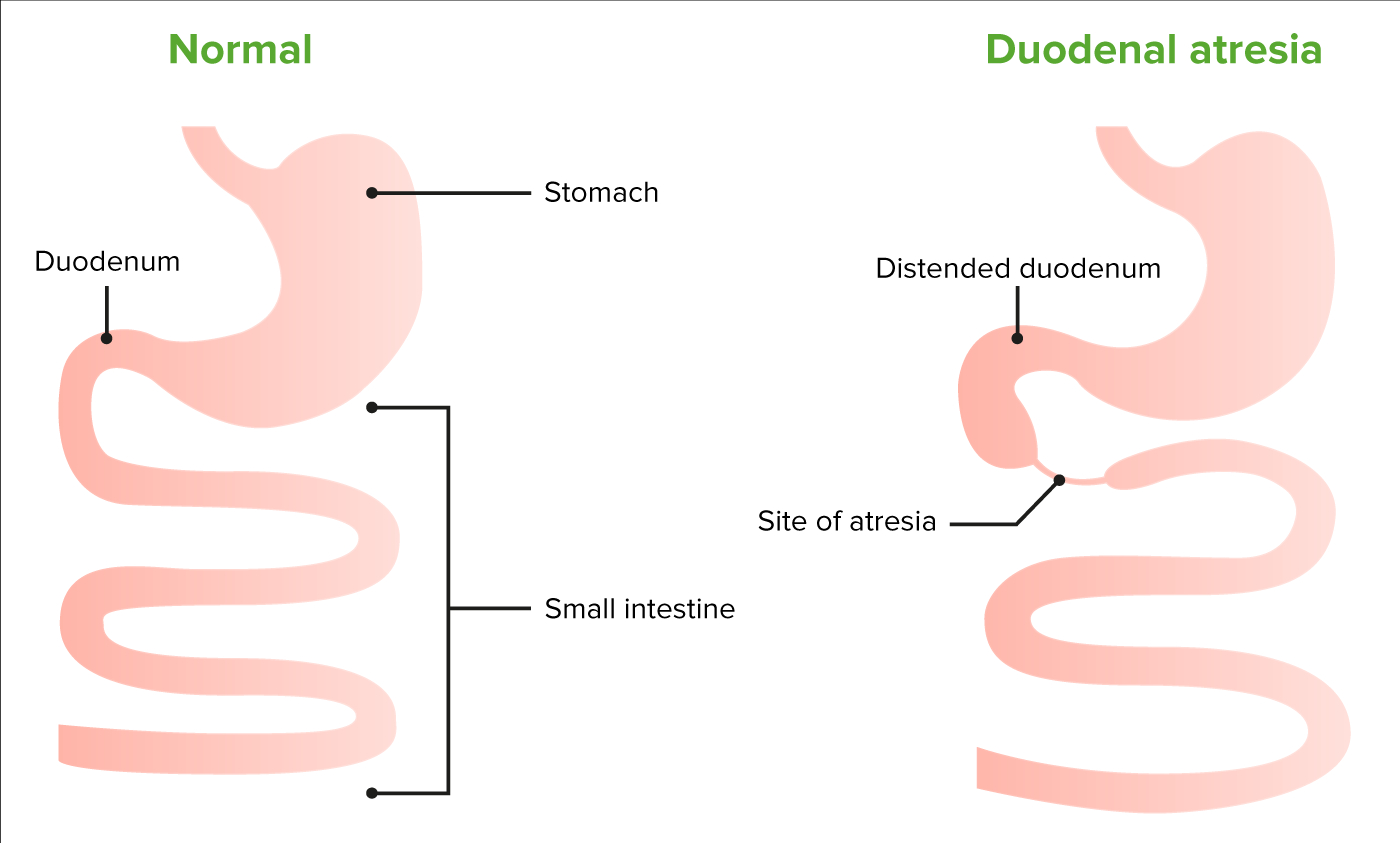
- Duodenal atresia and stenosis is a congenital (mechanical) obstruction of the duodenum caused by failure of the lumen to recanalize at 8-10 weeks gestation (gastric outlet obstruction).
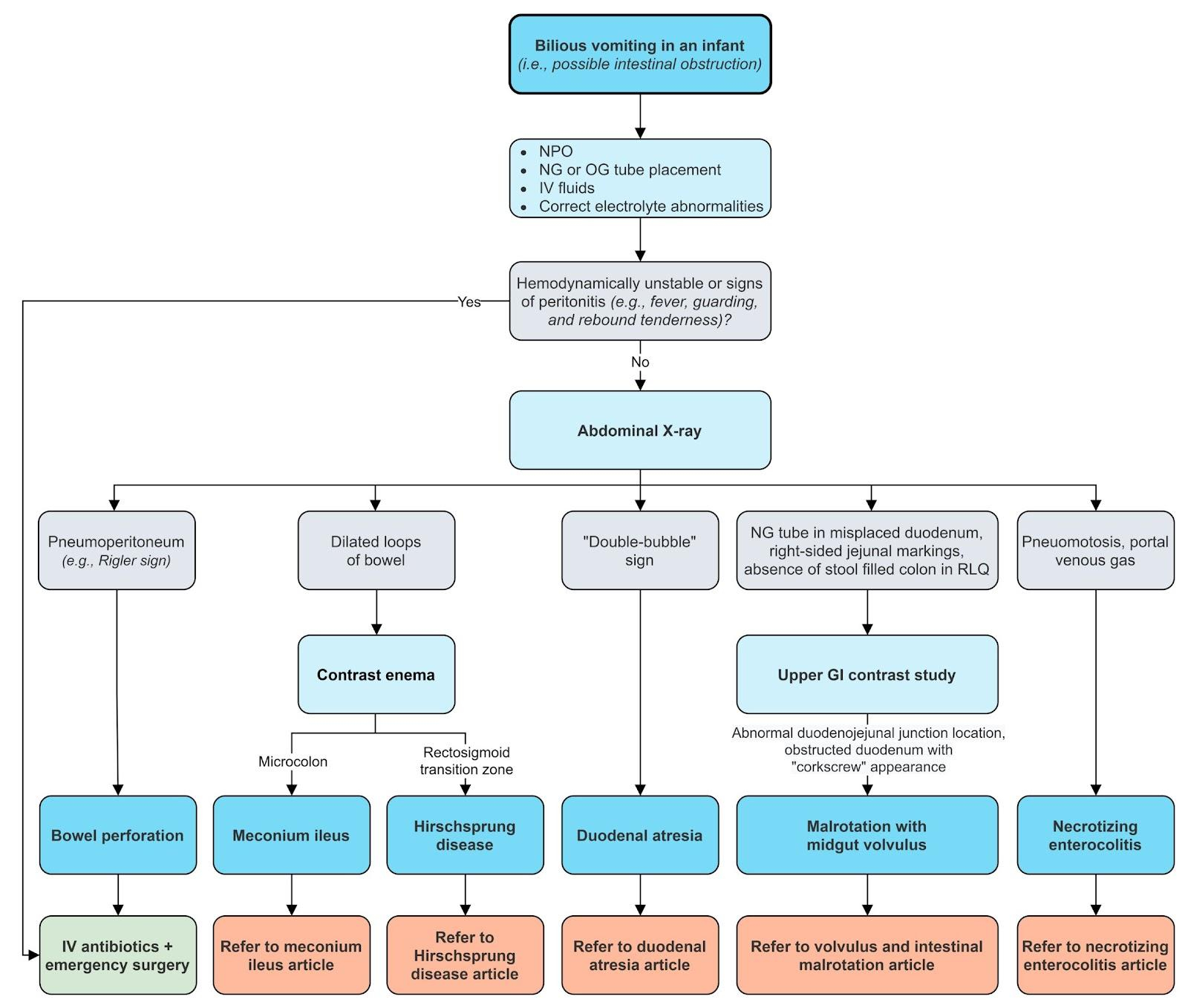
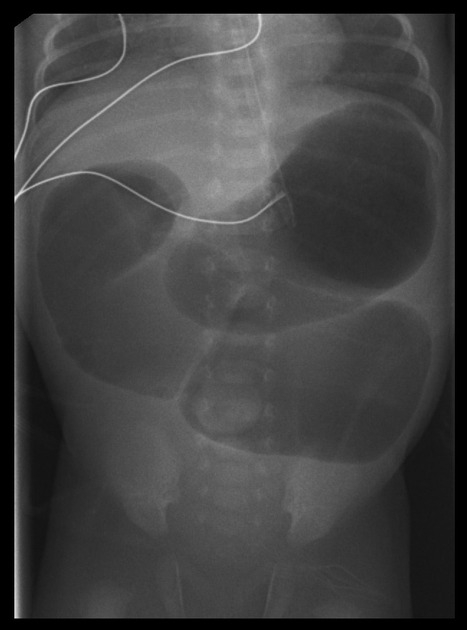
- Clinical features include; polyhydraminos (prenatal), distention of stomach, blind loop of duodenum (double-bubble sign), and bilious vomiting.
- This condition is associated with multiple congenital anomalies including; Down syndrome.
- Treatment is surgical correction (duodenoduodenostomy)
Presentation
- Physical examination of patients with duodenal atresia may reveal scaphoid abdomen with epigastric distention.
- Duodenal stenosis may present with emesis, weight loss, and failure to thrive.
Diagnosis
- Diagnosis may be suspected if prenatal ultrasound demonstrates gastric dilation with polyhydraminos.
- Abdominal X-ray shows air in the stomach, and proximal duodenum (double-bubble sign) with no distal bowel gas.

Differential diagnosis
- Pyloric stenosis.
- Small intestinal volvulus due to malrotation.
- Tracheoesophageal fistula.
Treatment
- Nasogastric decompression to deflate the stomach.
- Hydration, and correction of electrolytes (typically hypochloremic metabolic alkalosis).
- Duodenal atresia is surgically corrected by duodenoduodenostomy.
Complications
- Without treatment, this condition is fatal.
- Most frequent long term complications include blind-loop syndrome, megaduodenum with altered duodenal motility, and gastritis with duodenal-gastric reflux.
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
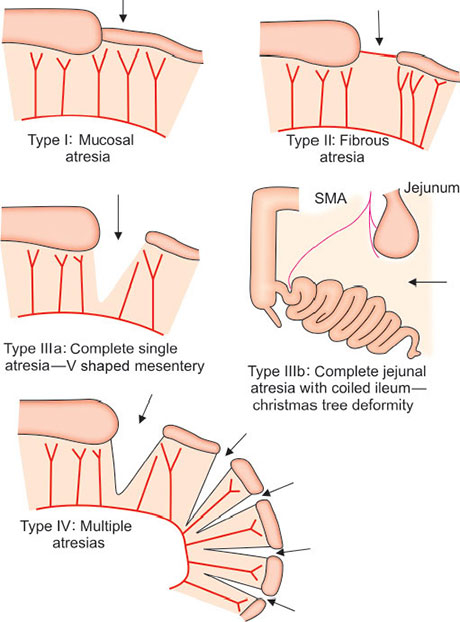
Jejunoileal Atresia
| Jejunoileal Atresia | |
|---|---|
| Definition |
|
| Epidemiology |
|
| Clinical Features |
|
| Diagnosis |
|
| Management |
|
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
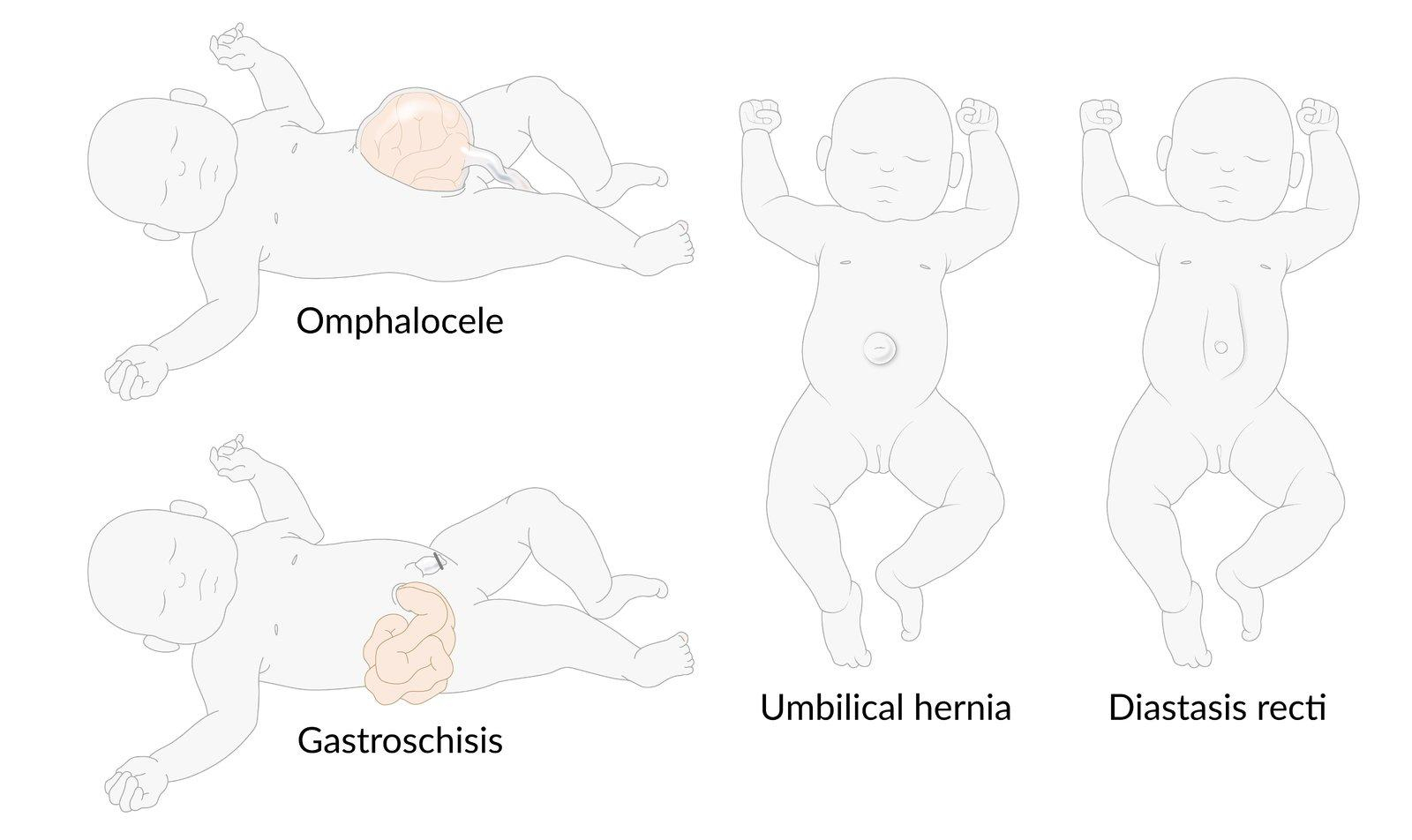
Pediatric Abdominal Wall Defects
Introduction
- Abdominal wall defects in pediatric patients are congenital anomalies characterized by incomplete closure or structural abnormalities of the abdominal wall, leading to herniation of abdominal contents.
- The two most common types are gastroschisis and omphalocele.
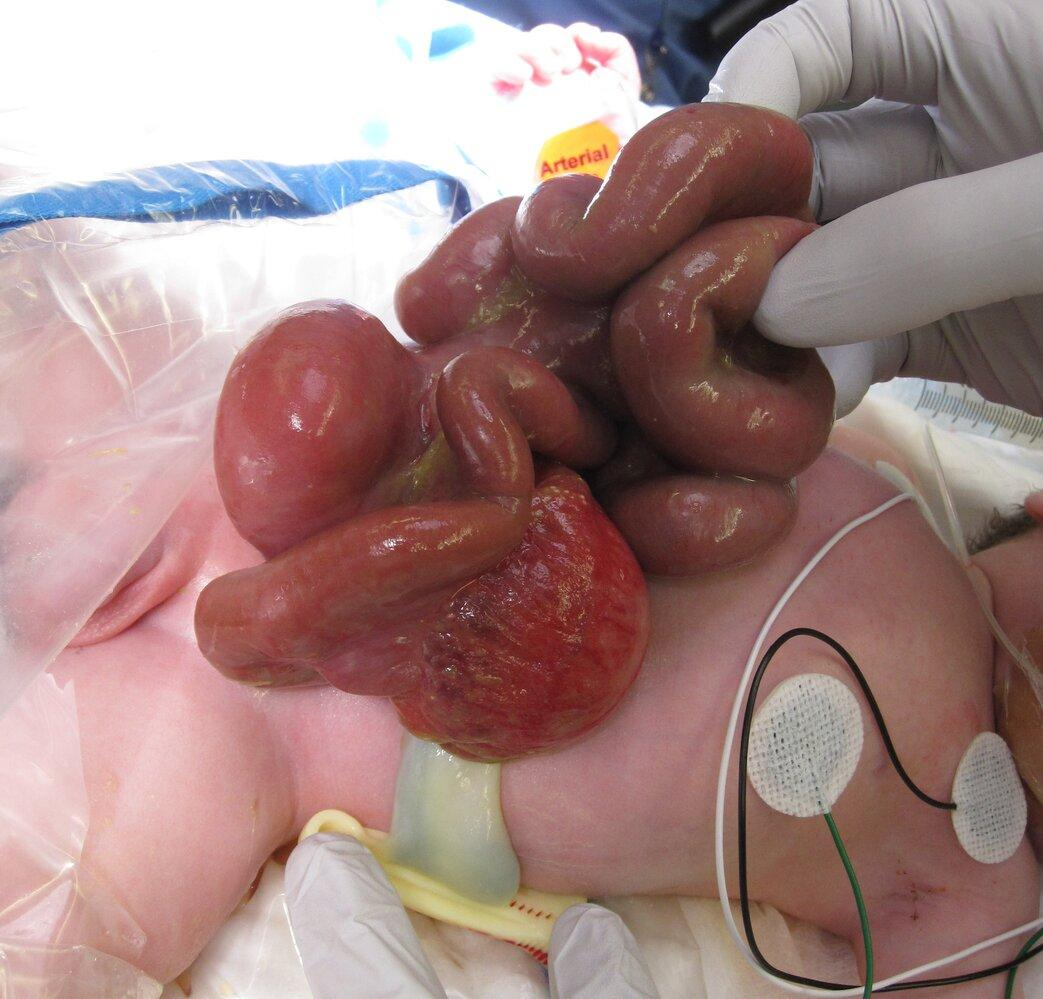
- Gastroschisis: an open defect typically to the right of the umbilicus, with exposed intestines lacking a protective membrane.
- Omphalocele: a midline defect covered by a sac, often associated with other congenital syndromes.
- These conditions are often diagnosed prenatally via ultrasound.
- These conditions can lead to life-threatening complications such as infection, bowel ischemia, and respiratory compromise.
| Pediatric Abdominal Wall Defects | |
|---|---|
| Diagnosis | Clinical Features |
| Umbilical hernia |
|
| Gastroschisis |
|
| Omphalocele |
|
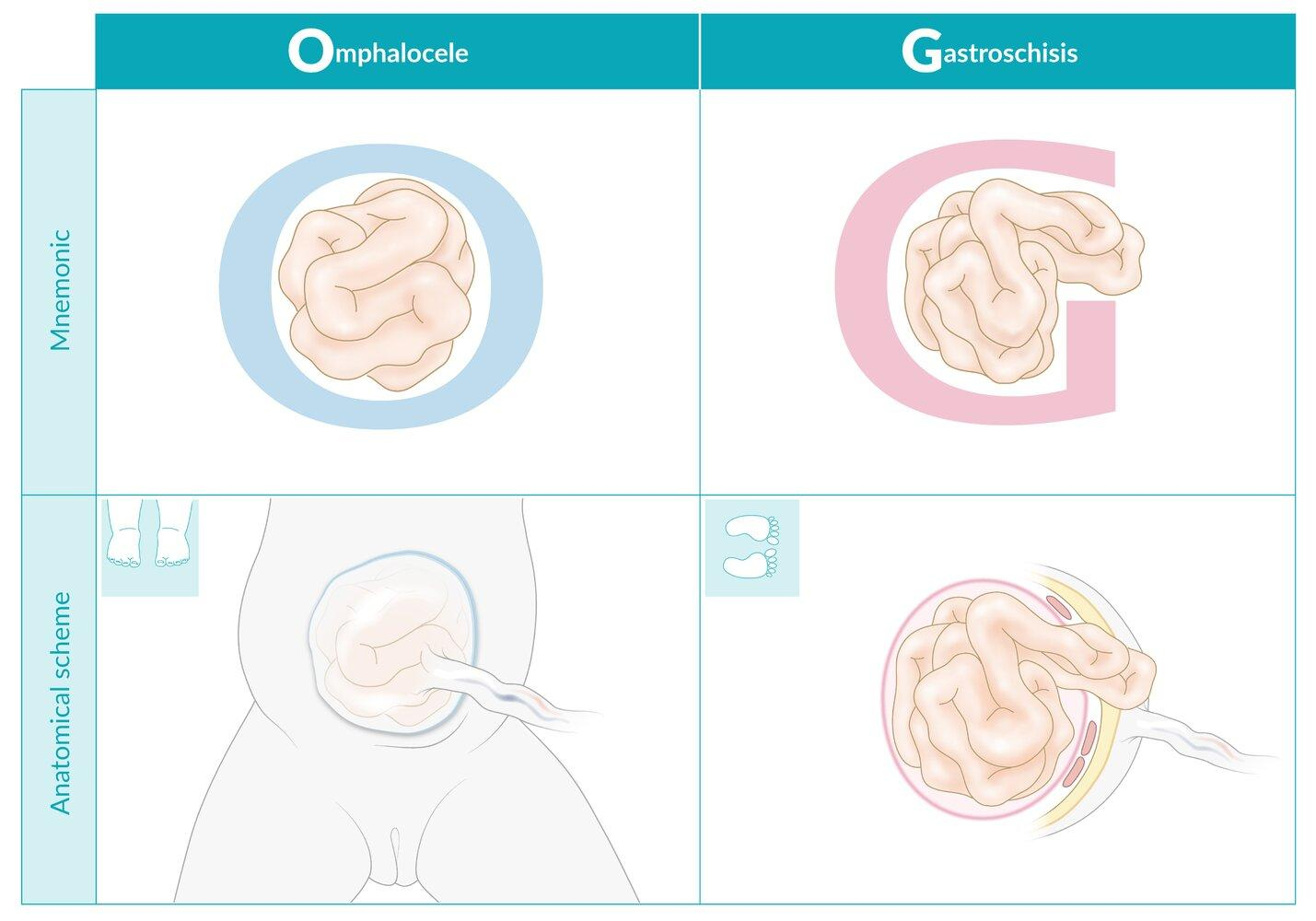
| Gastroschisis | Omphalocele | |
|---|---|---|
| Location | Right side | Center |
| Covering | Content not covered by membrane | Presence of peritoneum-amniotic membrane |
| Cord relation | No umbilical cord | Umbilical cord inserted in caudal area of the hernial sac |
| Content | Intestine, colon, bladder, gonads (occasionally) | Intestine, liver (in most cases), spleen, colon, bladder (occasionally) |
| Associations | Rarely associated with other congenital anomalies (15%) | Frequently associated with other congenital anomalies (40–80%) |
Comparison between Gastroschisis and Omphalocele

Management of Gastroschisis and Omphalocele
Gastroschisis Management
- Prenatal Care:
- Serial ultrasounds monitor fetal growth and bowel condition.
- Delivery is often via vaginal delivery unless obstetric complications arise.
- Immediate Postnatal Care:
- Protect exposed bowel with a sterile, non-adhesive wrap (e.g., saline-soaked gauze and plastic bag).
- Nasogastric decompression and IV fluids to prevent third-space losses.
- Broad-spectrum antibiotics to reduce infection risk.
- Surgical Repair:
- Primary closure if possible.
- Staged closure (silo placement with gradual reduction) for larger defects, followed by delayed fascial closure.
- Postoperative Care:
- Parenteral nutrition until bowel function resumes, with gradual enteral feeds.
- Complications include: necrotizing enterocolitis, bowel dysfunction
Omphalocele Management
- Prenatal Care:
- Assess for associated anomalies (e.g., cardiac, chromosomal).
- Delivery planning depends on defect size and comorbidities, with cesarean section considered for giant omphaloceles.
- Initial Stabilization:
- Cover the sac with a moist, non-adherent dressing.
- Evaluate for associated syndromes (e.g., Beckwith-Wiedemann, trisomies).
- Surgical Approach:
- Primary closure for small defects.
- Staged repair (e.g., mesh reinforcement, tissue expanders) for giant omphaloceles.
- Postoperative Care:
- Monitor for pulmonary hypertension, feeding difficulties, and recurrent herniation.
- Long-term follow-up for growth and developmental delays is essential.
Prognosis
- Gastroschisis has high survival rates (>90%) but may have long-term bowel motility issues.
- Omphalocele outcomes depend on associated anomalies, with higher mortality in syndromic cases.
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.
فيديوهات الشرح
بطاقات تفاعلية
أسئلة ممارسة
اشترك الآن