Introduction
Uterine rupture is a critical obstetric complication that poses a significant threat to both mother and child. This life-threatening condition occurs in roughly 1 in 4000 births, predominantly during labor, especially in women with a history of cesarean delivery.
Epidemiology
- Incidence: Approximately 1 in 4000 births
Etiology
Uterine rupture is chiefly induced by extensive uterine distention, often during active labor due to the substantial contractions. Contributing factors include:
- Uterine Distention: Prominent during labor due to intense contractions.
- Fetal Macrosomia: Large fetal size contributing to excessive stretching.
- Multiple Gestations: Increasing uterine stretch due to multiple fetuses.
- Oxytocin Overdose: Excessive use leading to hyperstimulation.
- Prior Uterine Surgery: Scar tissue from previous surgeries like cesarean deliveries or myomectomies enhances rupture risk.
- Additional Risk Factors: Advanced maternal age, short interdelivery interval, postterm pregnancy, and history of labor induction.
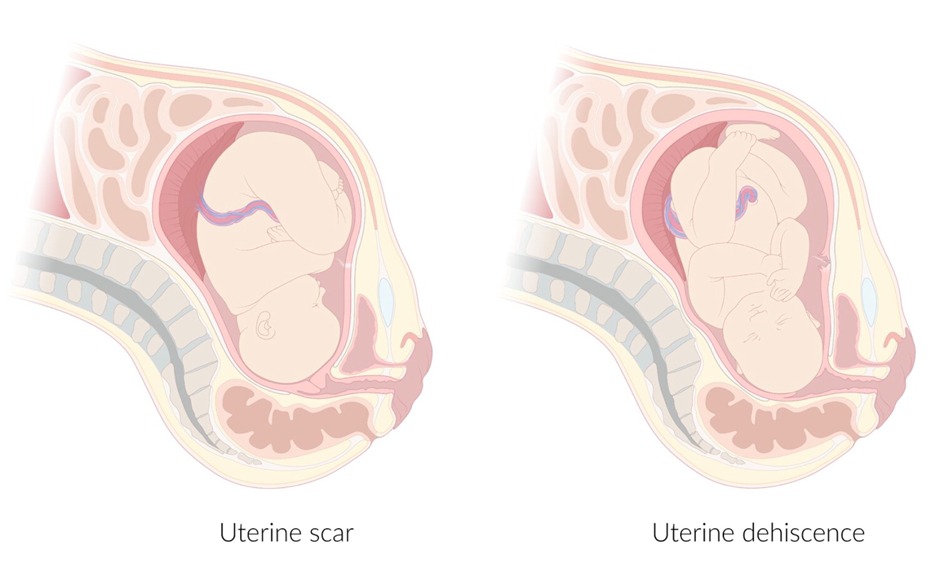
Classification
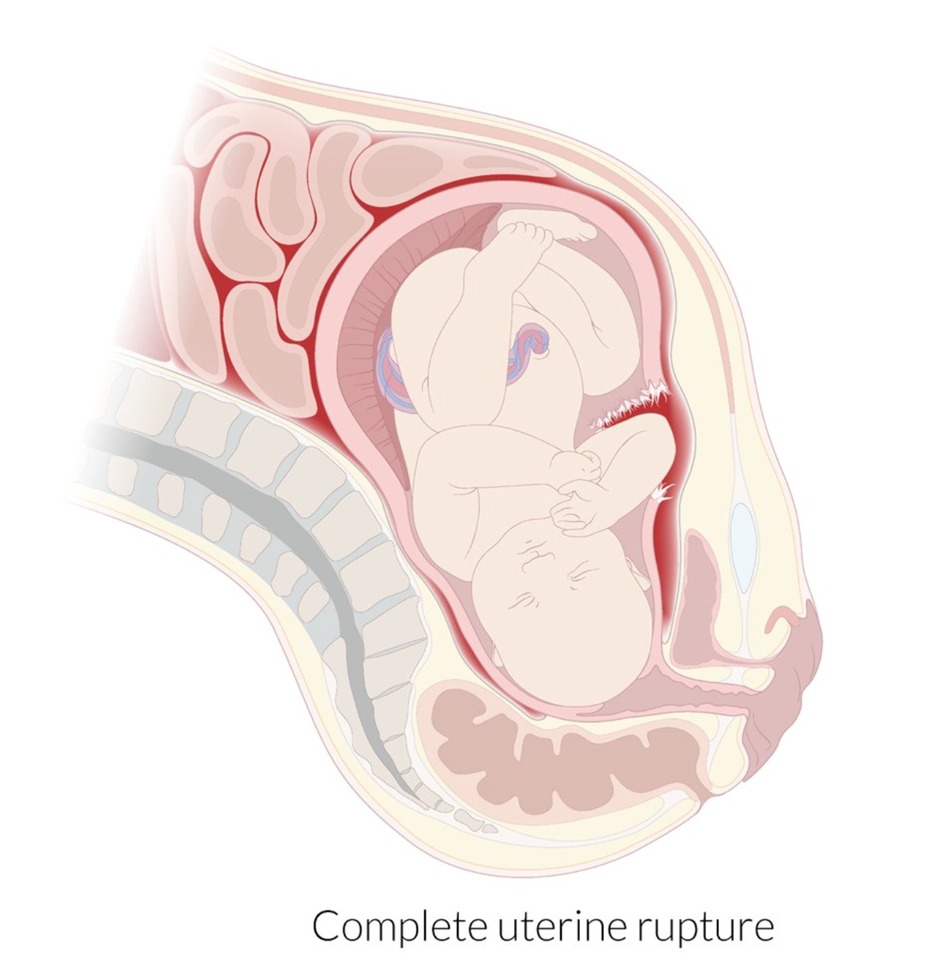
- Uterine Rupture: A complete disruption across all uterine layers, directly opening into the abdominal cavity.
- Uterine Dehiscence: Often termed a "closed rupture," it's a perforation that remains covered by the visceral peritoneum, typically discovered incidentally during cesarean delivery.
Clinical Features
Signs of imminent rupture include severe abdominal pain and hyperactive labor. Once rupture occurs, symptoms can include:
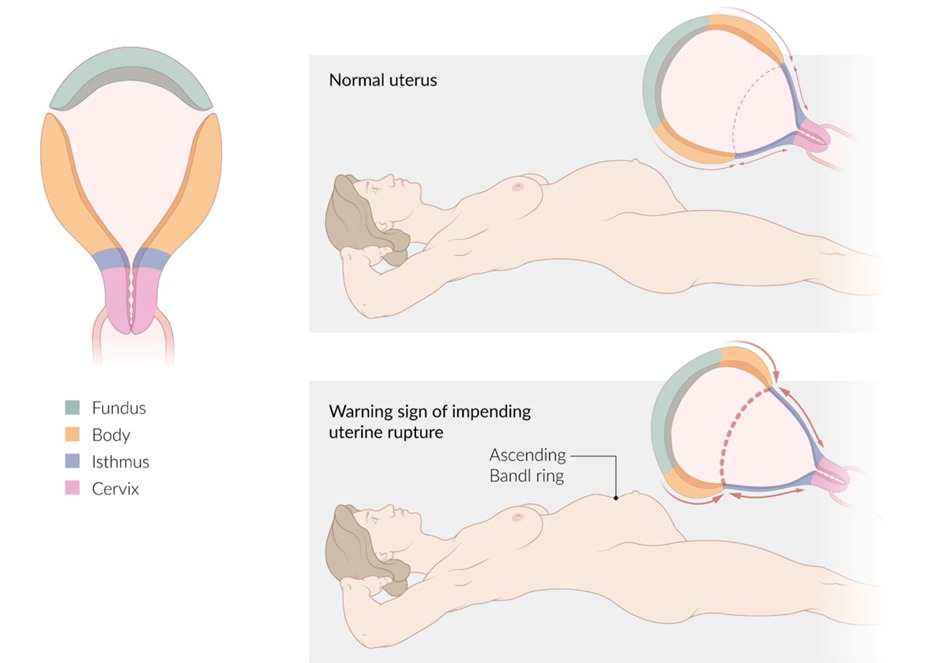
Signs of imminent uterine rupture
- Severe abdominal pain
- Increased contractions followed by hyperactive labor
- Bandl ring: muscular ring that can be seen above the belly button due to the powerful contractions of the upper uterine segment
Signs of uterine rupture
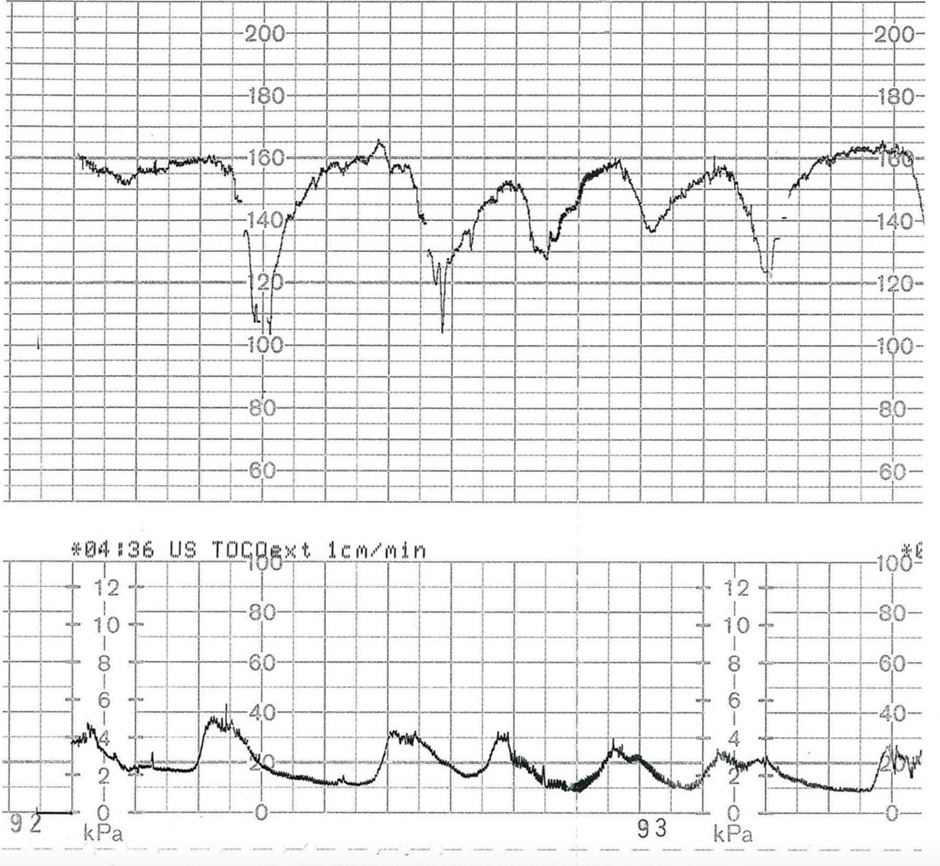
- Fetal distress (earliest and most sensitive sign)
- Severe abdominal pain
- Referred pain in the shoulder may be present.
- Sudden pause in contractions
- Light to moderate vaginal bleeding
- Hemodynamic instability (as a result of abdominal bleeding)
- Loss of fetal station (a specific but uncommon sign)
- Palpable fetal parts through the rupture (a specific but uncommon sign)
Diagnostics
- Uterine rupture diagnosis is primarily clinical, based on symptoms of fetal distress, severe pain, or vaginal bleeding. Immediate evaluation is critical, with bedside ultrasound as a supportive tool if needed, but not at the expense of delaying emergency care.
Differential Diagnoses
- The differential diagnoses include other causes of antepartum bleeding, emphasizing the unique presentation of uterine rupture.
Treatment
- Treatment involves the ABCDE approach with immediate hemodynamic support, consultation for emergency cesarean delivery, and avoidance of uterotonic agents.
- A hysterectomy may be considered if hemorrhage is uncontrollable.
Prognosis
- Both traumatic and spontaneous ruptures significantly elevate maternal and fetal mortality rates. Open ruptures, in particular, lead to hypovolemia and fetal hypoxia, increasing fetal mortality.
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.