Definitions
- Prelabor rupture of membranes (PROM): rupture of membranes before the onset of labor at ≥ 37 weeks'gestation
- Preterm prelabor rupture of membranes (PPROM): rupture of membranes before the onset of labor and before 37 weeks' gestation
- Prolonged rupture of membranes: rupture of membranes > 18 hours before the onset of labor
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Epidemiology and Prevalence
- PROM: ∼ 8% of pregnancies
- PPROM: ∼ 2–3% of pregnancies
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Risk factors for preterm labor and birth
- Prior OB/GYN history
- Prior PTB (especially multiple PTBs or PTB at an early gestational age)
- Prior cervical surgery (eg, cone biopsy, LEEP)
- Multiple D&Es
- Uterine anomalies
- Maternal demographics
- <17 or >35 years of age
- Non-Hispanic Black race, Indigenous women
- Lower educational level (eg, <12 grades)
- Single marital status
- Lower socioeconomic status
- Short interpregnancy interval (eg, <18 months)
- Other social factors (eg, poor access to medical care, physical abuse, acculturation)
- Nutritional status/physical activity
- BMI <18.5 kg/m2 or prepregnancy weight <50 kg (<120 lb)
- Poor nutritional status
- Long working hours (eg, >80 hours/week)
- Hard physical labor (eg, shift work, standing >8 hours)
- Current maternal/pregnancy characteristics
- Conception by assisted reproductive technology (eg, IVF)
- Multiple gestation
- Fetal disorder (eg, chromosome anomaly, structural abnormality, growth restriction, death, etc)
- Vaginal bleeding (eg, 1st and 2nd trimester, placenta previa, abruption)
- Poly- or oligohydramnios
- Maternal medical conditions (eg, hypertension, diabetes, thyroid disease, asthma, etc)
- Maternal abdominal surgery during pregnancy
- Psychological issues (eg, stress, depression, unplanned pregnancy)
- Substance use:
- Smoking (eg, tobacco)
- Heavy alcohol consumption
- Cocaine
- Heroin
- Infection:
- Bacterial vaginosis
- Trichomoniasis
- Chlamydia
- Gonorrhea
- Syphilis
- Urinary tract (eg, asymptomatic bacteriuria, pyelonephritis)
- Severe viral infection
- Intrauterine infection
- Short cervical length between 14 and 28 weeks
- Positive fFN between 22 and 34 weeks
- Uterine contractions
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Clinical Presentation
- Presentation: PPROM often presents with a sudden gush of clear or pale yellow fluid from the vagina or as a continuous/intermittent leak, sometimes described simply as a sensation of wetness.
- Physical Exam:
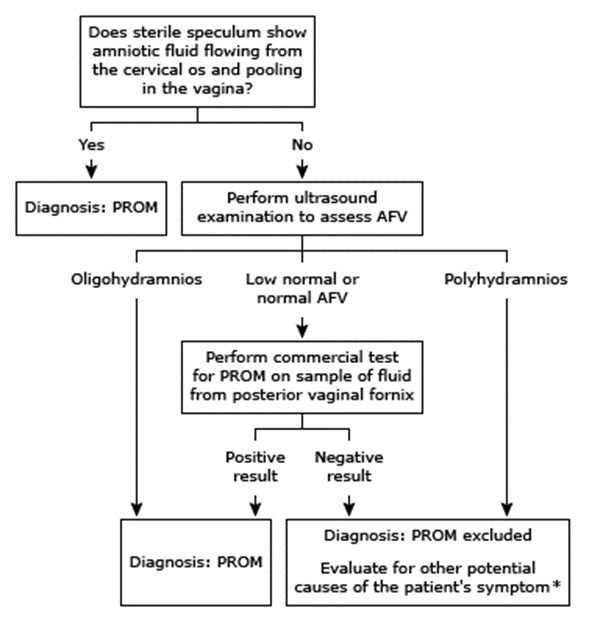
- Use a sterile speculum to examine the cervix and vagina; avoid digital exams to reduce infection risk.
- Diagnosis is indicated by amniotic fluid leaking from the cervical os or pooling in the vaginal vault.
- The cervix may be dilated or effaced; in rare cases, fetal parts or the umbilical cord may prolapse.
- Ultrasonography:
- Commonly shows reduced amniotic fluid volume (oligohydramnios), with an amniotic fluid index (AFI) ≤5 cm or a maximum vertical pocket (MVP) <2 cm.
- Laboratory Tests:
- Normal hematology and chemistry unless infection or other complications are present.
- Specific tests are available to identify amniotic fluid.
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Complications
| Pregnancy complication | Potential consequences for offspring | Potential maternal consequences |
| Intrauterine infection |
|
|
| Umbilical cord compression |
|
|
| Oligohydramnios |
|
|
| Fetal malpresentation |
|
|
| Umbilical cord prolapse |
|
|
| Placental abruption |
|
|
| Preterm birth |
|
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Assessments to consider after confirmation of membrane rupture
- Complete blood count
- Rectovaginal culture for group B Streptococcus
- Ultrasound examination for residual amniotic fluid volume; fetal growth, position, and anatomy; biophysical profile
- Cardiotocography to monitor fetal heart rate (including a nonstress test) and frequency of uterine contractions
- Testing for Neisseria gonorrhoeae, Chlamydia trachomatis, Trichomonas vaginalis, and bacterial vaginosis by standard methods in women with risk factors for acquiring an ST
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Management of Preterm Prelabor Rupture of Membranes (PPROM)
- Management Considerations: Factors include gestational age, neonatal care level, infection presence, labor or placental abruption, fetal presentation, fetal heart rate, and cervical status.
- Immediate Delivery for Unstable Patients: Indicated for intrauterine infection, placental abruption, nonreassuring fetal tests, or high cord prolapse risk.
- Delivery for Stable Patients ≥34 Weeks: Suggested over expectant management for accurately dated pregnancies. For uncertain dates, consider expectant management until 36-37 weeks.
- Expectant Management for Stable Patients <34 Weeks:
- Antenatal Corticosteroids: Administered to pregnancies between 23+0 and 33+6 weeks of gestation to significantly reduce neonatal morbidity and mortality. Consideration for use extends to those at 34+0 to 36+6 weeks if delivery is anticipated within a week and no prior course has been given.
- Infection Screening: Perform third-trimester STI screening and manage positive cases appropriately. Screen for Group B Streptococcus (GBS) upon admission and treat if positive.
- Prophylactic Antibiotic Therapy: A seven-day course of prophylactic antibiotics is recommended for women with PPROM <34+0 weeks to reduce maternal and fetal infection risks, thereby delaying labor. Preferred regimen includes azithromycin plus ampicillin followed by amoxicillin.
- Tocolysis: Indicated primarily to delay delivery for up to 48 hours, allowing for corticosteroid administration. It's not recommended beyond this period, in advanced labor, or with signs of chorioamnionitis or other contraindications.
- Hospitalization vs. Home Care: Most clinicians hospitalize women with PPROM for continuous monitoring due to potential complications. Limited studies on outpatient management show no significant differences in outcomes, but hospitalization remains the standard due to safety concerns.
- Fetal Monitoring: Routine surveillance like nonstress tests (NST), biophysical profiles (BPP), and amniotic fluid volume assessments are employed, though their sensitivity for predicting fetal infection is low.
- Maternal Monitoring: Monitor for signs of infection through clinical parameters. Routine amniocentesis to screen for intra-amniotic infection is not standard but may be considered in uncertain cases.
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.
فيديوهات الشرح
بطاقات تفاعلية
أسئلة ممارسة
اشترك الآن