شرح المدرسين
Summary
Polyhydramnios, characterized by an excess of amniotic fluid, poses unique challenges and risks in pregnancy. This condition can arise from various etiologies, often linked to fetal disorders, maternal diabetes, multiple gestations, or fetal anemia, with decreased fetal swallowing or increased urination typically underlying the increased amniotic fluid volume (AFV).
Pathogenesis and Etiology
Polyhydramnios may be idiopathic or stem from conditions affecting fetal swallowing or urination. Commonly associated issues include fetal malformations, genetic disorders, maternal diabetes, multiple gestation, fetal anemia, and, rarely, Bartter syndrome.
| Conditions associated with polyhydramnios | |
| Idiopathic 70% of cases | |
|
Fetal structural anomaly that impedes swallowing
|
|
|
Genetic syndromes
|
|
|
High fetal cardiac output state
|
|
| Twin-twin transfusion syndrome | |
| Maternal diabetes mellitus | |
| Macrosomia | |
| Hydrops fetalis |
Diagnosis
A quantitative measurement is recommended for those with a qualitative impression of polyhydramnios, utilizing the single deepest pocket (SDP) ≥8 cm or amniotic fluid index (AFI) ≥24 cm criteria. These indices, while not perfect, allow for standardized tracking over time.
| Criteria for mild, moderate, and severe polyhydramnios | |||
| Mild | Moderate | Severe | |
| Single deepest pocket | 8.0 to 11.9 cm | 12.0 to 15.9 cm | ≥16.0 cm |
| Amniotic fluid index | 24.0 to 29.9 cm | 30.0 to 34.9 cm | ≥35.0 cm |
Postdiagnostic Evaluation
- Detailed sonographic evaluation is crucial to identify potential fetal anomalies or hydrops.
- Laboratory tests might include screening for gestational diabetes, fetomaternal hemorrhage, and infectious agents, depending on sonographic findings.
- Fetal microarray analysis is advised in severe cases or when anatomic anomalies are present.
Outcome
The prognosis varies with the polyhydramnios' severity and root cause.
Risks include maternal respiratory issues, preterm labor, membrane rupture, fetal malposition, and possibly fetal or neonatal death.
Initial Management
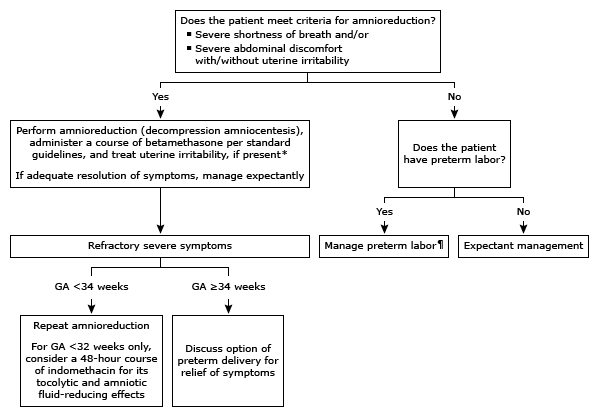
Treatment primarily targets severe idiopathic polyhydramnios in singleton pregnancies, where symptoms significantly impact daily life. Options include:
- Asymptomatic or Mild Symptoms: Intervention is generally not recommended unless symptoms are intolerable.
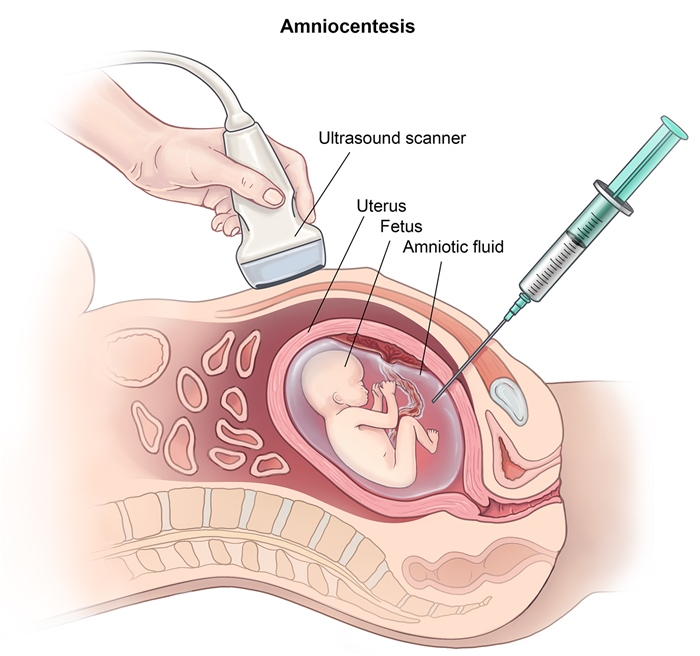
- Severe Symptoms: Amnioreduction is preferred over indomethacin due to potential fetal risks. Antenatal betamethasone is also administered. For those under 32 weeks experiencing uterine contractions, a short indomethacin course may be beneficial.
Timing of Delivery
For mild idiopathic polyhydramnios, delivery is suggested between 39+0 to 40+0 weeks. The timing for other scenarios should be based on the specific etiology and severity of the condition.
Intrapartum Management
During labor, the increased fetal mobility due to excess fluid necessitates frequent checks of fetal position to mitigate risks associated with sudden uterine decompression, such as cord prolapse or abruption. Prophylactic amnioreduction may be considered to prevent these complications.
Conclusion
Polyhydramnios, while challenging, can be managed effectively through a comprehensive approach that includes accurate diagnosis, careful monitoring, and targeted interventions. Understanding the condition's underlying causes and potential risks enables clinicians to tailor management strategies, ensuring the best possible outcomes for both mother and child.
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.