Summary
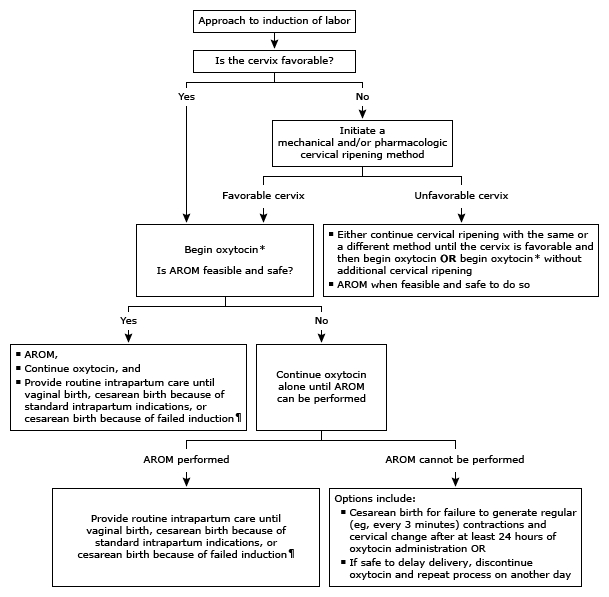
Induction of labor is a critical procedure aimed at stimulating uterine contractions before spontaneous labor begins, with the goal of achieving a vaginal birth. The decision to induce labor involves assessing the cervical status to determine the appropriate approach, whether it involves cervical ripening or direct initiation of oxytocin.
Indications for induction of labor
- Post-term pregnancy (≥ 42 weeks of pregnancy or gestation)
- PPROM after 34 weeks
- PROM at term
- Hypertension during pregnancy, preeclampsia, eclampsia, HELLP syndrome
- Maternal diabetes to avoid post-term pregnancy (risk of macrosomia)
- Maternal request at term
- Intrauterine fetal demise
Contraindications for induction of labor
- History of uterine rupture; previous classical cesarean incision
- Complete placenta previa
- Vasa previa
- Transverse fetal lie
- Cord prolapse
- Active maternal genital herpes
- Nonreassuring fetal heart rate
Bishop score
- Definition: a scoring system used to assess the cervix and the likelihood of successful induction of labor
- Interpretation
- Bishop score ≥ 8: favorable cervix (ready for vaginal delivery)
- Bishop score ≤ 6: unfavorable cervix (not ready for vaginal delivery)
- Alternative: simplified Bishop score
- Considers only fetal station, cervical dilation, and cervical effacement
- A score of ≥ 5 indicates a favorable cervix.
| Bishop scoring system | ||||
| 0 | 1 | 2 | 3 | |
| Dilation, cm | Closed | 1 to 2 | 3 to 4 | ≥5 to 6 |
| Effacement, % | 0 to 30 | 40 to 50 | 60 to 70 | ≥80 |
| Station | -3 | -2 | -1, 0 | +1, +2 |
| Cervical consistency |
Firm | Medium | Soft | |
| Position of the cervix | Posterior | Midposition | Anterior | |
Choice of Cervical Ripening Agent
The selection between a balloon catheter and prostaglandins (E2 or E1) for cervical ripening depends on various factors, including institutional protocols, physician and patient preferences, and considerations of convenience, cost, and side effects. Each method has its specific contraindications and administration guidelines.
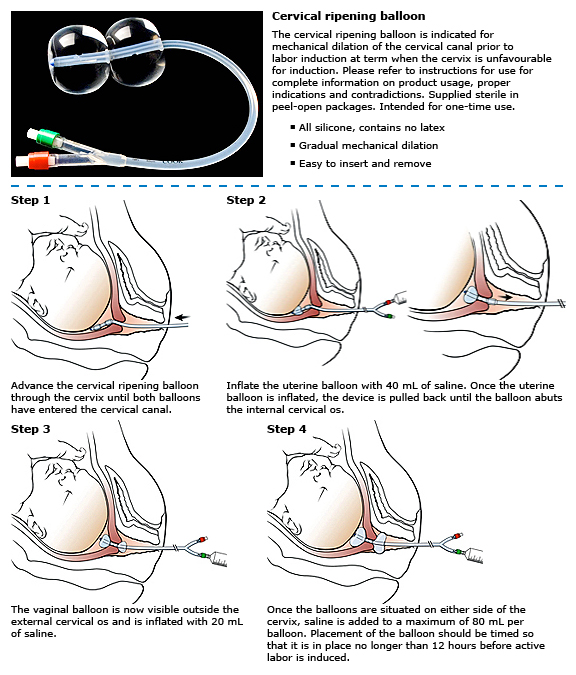
- Balloon Catheter
- Contraindications include a low-lying placenta and, variably, ruptured membranes.
- The catheter is placed using aseptic technique, with oxytocin starting concurrently or after removal.
- It boasts no systemic side effects and a lower rate of tachysystole compared to prostaglandins.
- Prostaglandins
- Contraindications include a history of cesarean birth or major uterine surgery for misoprostol and regular painful uterine activity.
- Administration methods vary, including vaginal and oral routes for misoprostol and endocervical or vaginal inserts for dinoprostone, with specific dosing schedules.
- Side effects can include tachysystole, fever, and gastrointestinal symptoms, with management strategies outlined for discomfort and contractile abnormalities.
Conclusion
The induction of labor is a complex process that requires careful consideration of the patient's cervical status, the most appropriate cervical ripening agent, and the overall induction protocol. By adhering to a structured approach and considering the benefits and risks of different methods, healthcare providers can optimize outcomes for both the mother and the fetus. Collaboration between the patient and the healthcare team is crucial to tailor the induction plan to meet individual needs and preferences, ultimately aiming for a safe and effective delivery.
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.