Summary
The third trimester is a critical period for assessing fetal well-being and preparing for delivery. Fetal surveillance testing, typically initiated from 32 weeks' gestation onwards, aims to monitor fetal health and mitigate the risk of adverse outcomes.
Indications for Antepartum Fetal Surveillance
- High-risk pregnancies, such as those involving maternal medical conditions or fetal concerns that increase the risk of hypoxic injury or death.
- Decreased fetal movement as perceived by the mother.
Key Surveillance Methods
- Kick Counts:
- Mothers count fetal movements within a set period, usually 1 or 2 hours. A reduction in movement might necessitate further testing. However, the effectiveness of kick counts in predicting adverse outcomes is debated due to varying monitoring standards and limited evidence of impact.
- Nonstress Test (NST):
- It's a noninvasive procedure designed to assess fetal well-being by monitoring the fetal heart rate (FHR) response to spontaneous fetal movements. A healthy fetus is expected to have a temporary increase in heart rate with movements.
- Methodology of NST
- Monitoring Duration: The test involves continuous electronic fetal heart rate monitoring for a minimum of 20 minutes.
- Assessment: The FHR tracing is evaluated for the presence of accelerations ( ≥ 15 beats/minute above baseline and last ≥ 15 seconds ) and decelerations ( ≥ 15 beats/minute below baseline and last ≥ 15 seconds ) . Accelerations are a reassuring sign, indicating fetal well-being.
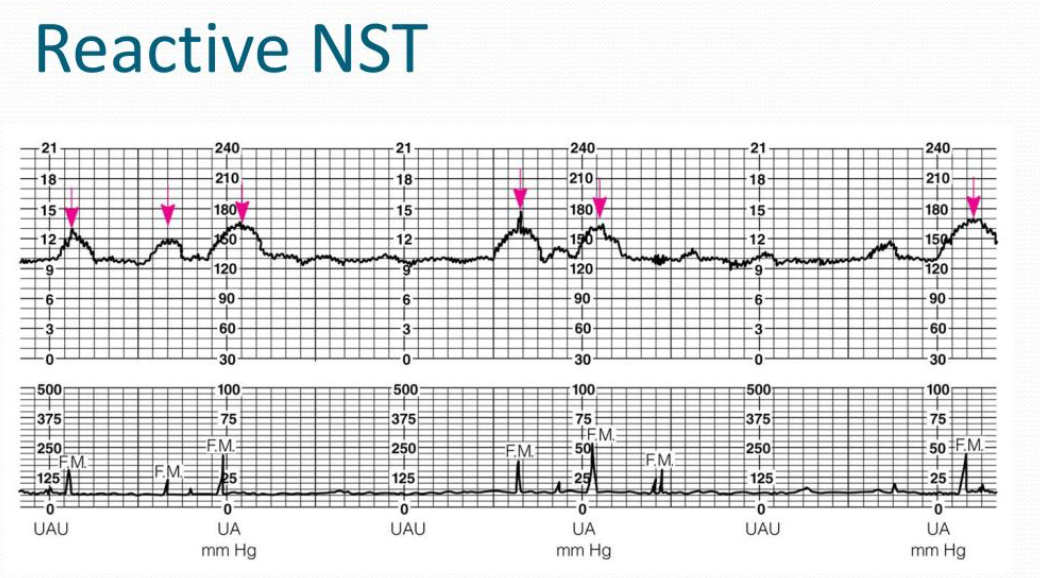
- Interpretation of NST Results
- Reactive NST: Characterized by at least two FHR accelerations within a 20-minute period, this outcome is considered normal and reassuring. No further testing is needed if the initial concern for testing is resolved. However, if concerns persist, NSTs may be repeated, typically at weekly intervals.
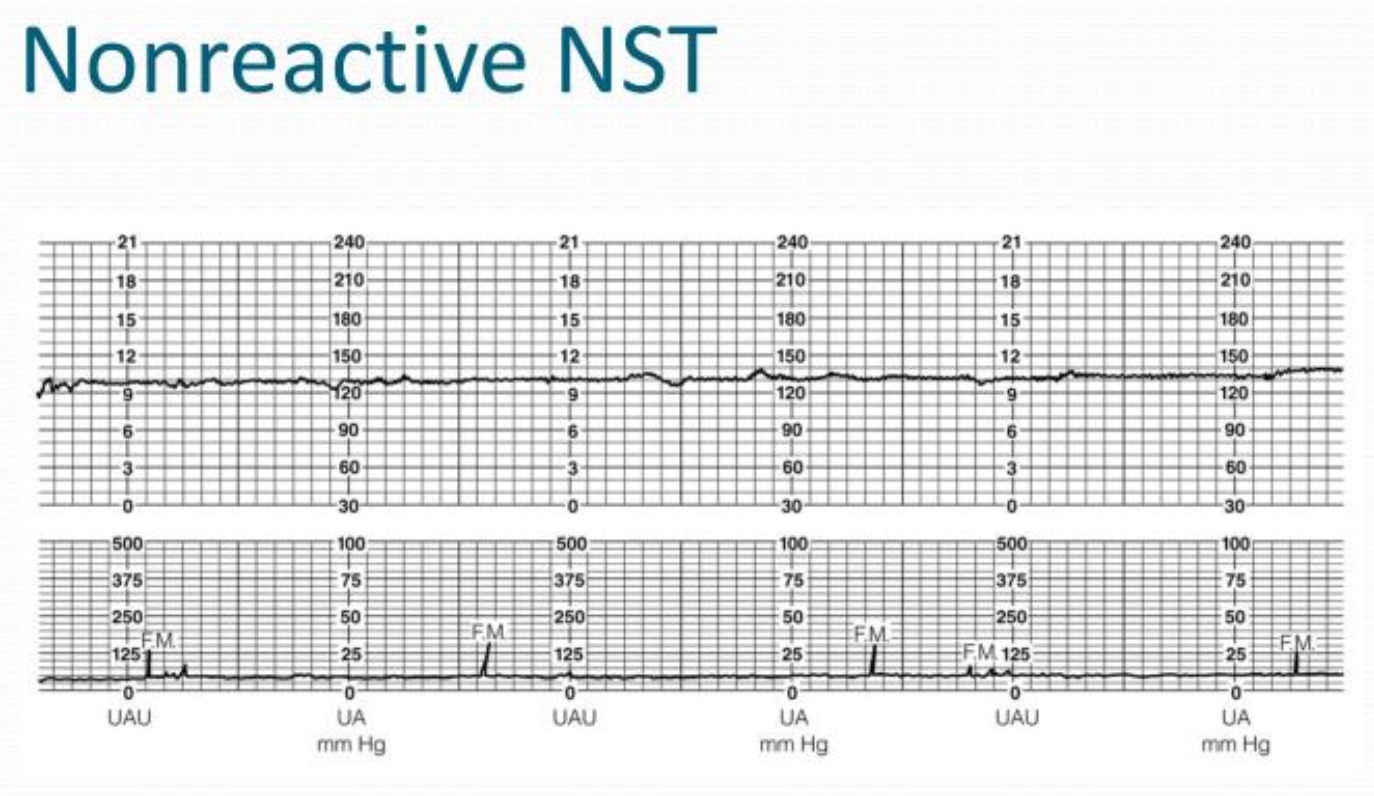
- Nonreactive NST: Defined by fewer than two FHR accelerations over a 40-minute monitoring period, a nonreactive NST may signal potential issues. Causes for a nonreactive result can include fetal sleep, hypoxemia, acidemia, neurologic or cardiac abnormalities, fetal immaturity, or maternal drug use.
- Reactive NST: Characterized by at least two FHR accelerations within a 20-minute period, this outcome is considered normal and reassuring. No further testing is needed if the initial concern for testing is resolved. However, if concerns persist, NSTs may be repeated, typically at weekly intervals.
- Next Steps After a Nonreactive NST
Following a nonreactive Nonstress Test (NST), it's crucial to undertake further assessment to evaluate fetal well-being comprehensively- Repeat NST: Sometimes, an initial nonreactive result may be due to temporary factors such as fetal sleep. Repeating the NST after a short interval (typically 30 minutes) can provide additional information.
- Vibroacoustic Stimulation: This technique involves using sound stimulation to awaken or provoke a response from the fetus. If no Fetal Heart Rate (FHR) accelerations are observed within the first 20 minutes of NST, vibroacoustic stimulation may be employed to elicit accelerations.
- Biophysical Profile (BPP): The BPP combines an ultrasound assessment with an NST to give a more comprehensive picture of fetal health.
- Contraction Stress Test (CST): The CST assesses how the fetal heart rate responds to uterine contractions. It's performed by monitoring the FHR in response to naturally occurring or induced contractions. A CST can be considered if the BPP is not available or if additional information on uteroplacental function is required.
- Address Potential Modifiable Factors: If there are identifiable factors that could contribute to a nonreactive NST (such as maternal smoking close to the test time), efforts should be made to modify these factors before retesting.
- Contraction Stress Test (CST)
- It is an antepartum evaluation designed to measure fetal heart rate (FHR) responses to uterine contractions, providing insight into fetal oxygenation and well-being. The CST is deemed safe when there are no contraindications to labor or vaginal delivery.
- Methodology OF CST
- Cardiotocography is utilized to simultaneously monitor FHR and uterine contractions.
- If fewer than three contractions of at least 40 seconds' duration occur within 10 minutes, contractions may be induced using nipple stimulation or intravenous (IV) oxytocin administration.
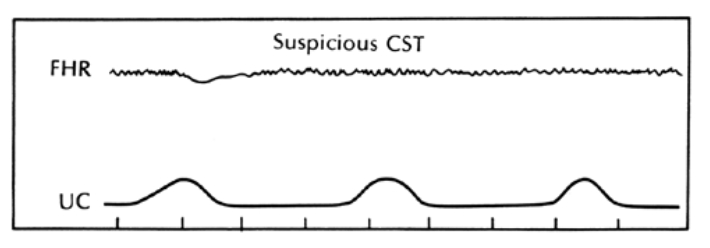
- Interpretation
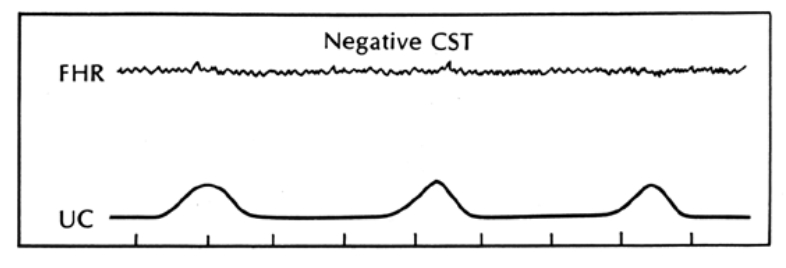
- Negative CST: Indicates the absence of late FHR decelerations or significant variable decelerations with uterine contractions, suggesting a low risk of fetal hypoxia.
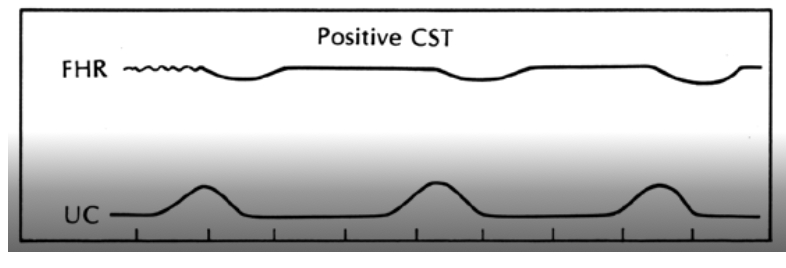
- Positive CST: Characterized by late decelerations following 50% or more of contractions, signifying potential uteroplacental insufficiency and a higher risk of fetal distress. This result may necessitate repeat testing or considerations for delivery.
- Equivocal CST: Occurs when there are intermittent variable decelerations or late decelerations, or when decelerations are noted with uterine tachysystole. This ambiguous outcome warrants a repeat CST within 24 hours.
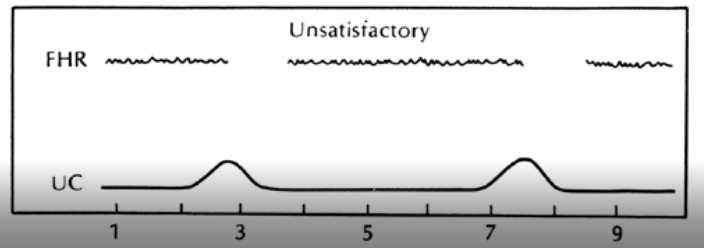
- Unsatisfactory CST: Results when the FHR tracing is uninterpretable or if an insufficient number of contractions (less than three in 10 minutes) are generated. In such cases, a repeat CST with an alternative method of contraction induction is recommended.
- Negative CST: Indicates the absence of late FHR decelerations or significant variable decelerations with uterine contractions, suggesting a low risk of fetal hypoxia.
- Biophysical Profile (BPP):
- It is a comprehensive fetal assessment that combines an ultrasound evaluation with a Nonstress Test (NST) to gauge fetal well-being. This noninvasive test, performed typically in the third trimester, offers valuable insights into fetal health, particularly in pregnancies considered at high risk.
- Methodology
- The BPP is conducted through an ultrasound examination lasting about 30 minutes, focusing on specific fetal parameters: movement, tone, breathing movements, and amniotic fluid volume.
- Following the ultrasound, an NST is performed to monitor fetal heart rate in response to fetal movements. However, if the ultrasound parameters are all normal, the NST might be skipped.
- Components of the full biophysical profile test
Biophysical profile scoring criteria Parameter Normal results (= 2 points) Fetal movement - 2 points if ≥ 3 body or limb movements in 30 minutes
Fetal tone - 2 points if ≥ 1 episodes within 30 minutes of either:
- Fetal extremity extension with return to flexion
- Opening or closing of a hand
Fetal breathing - 2 points if ≥ 1 rhythmic breathing episode(s) lasting ≥ 30 seconds in 30 minutes
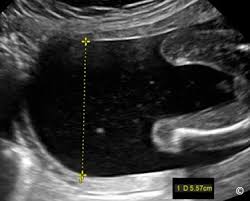
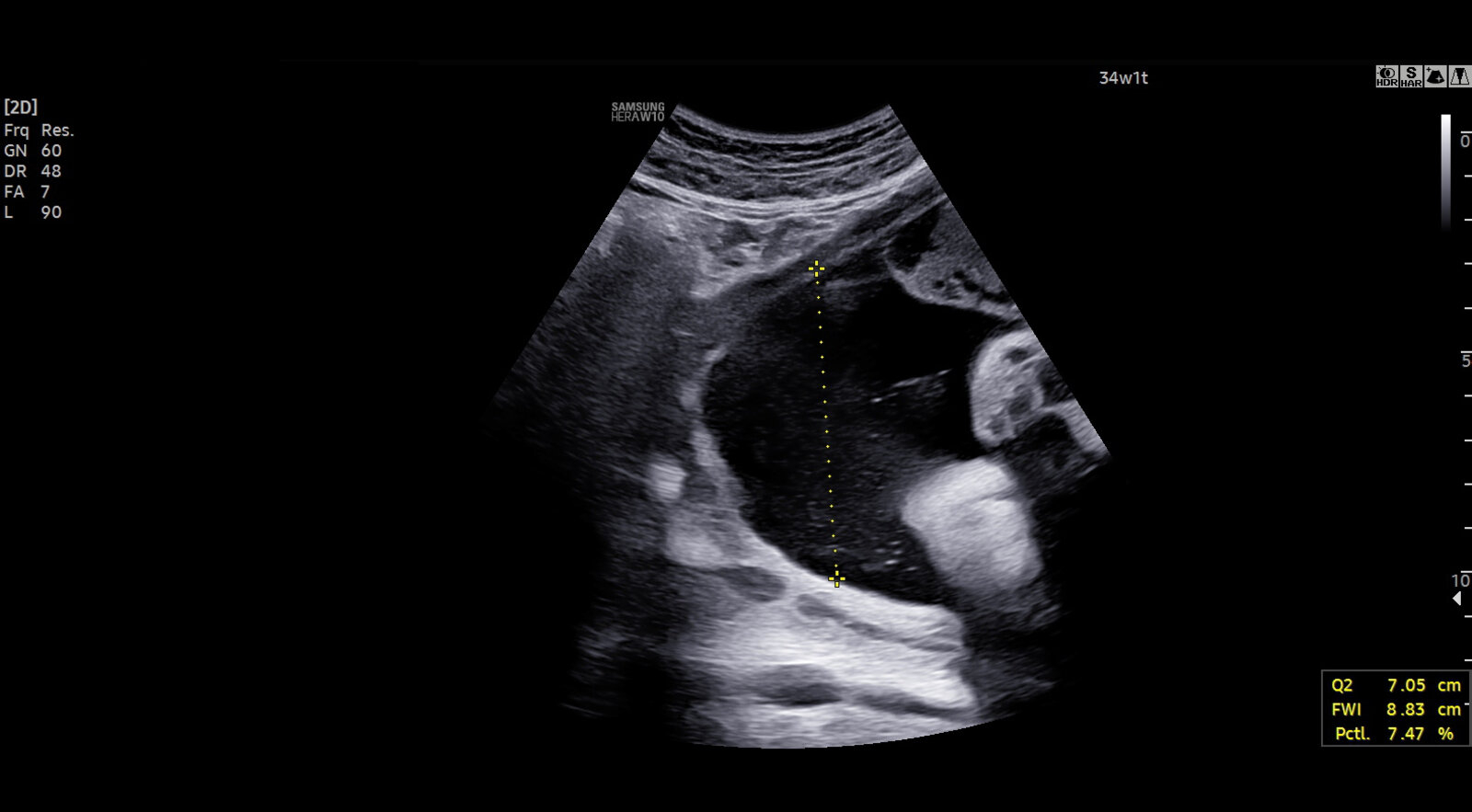
Amniotic fluid volume - 2 points if a single deepest vertical pocket > 2 cm with a horizontal dimension ≥ 1 cm
Nonstress test - Reactive nonstress test
- 2 points if reactive, defined as at least 2 episodes of FHR accelerations of at least 15 bpm and at least 15 seconds duration from onset to return associated with fetal movement.
- Follow-Up Recommendations
- The follow-up actions based on the BPP scores are tailored to whether oligohydramnios is present and the total score obtained:
- ≥ 8 Points (Without Oligohydramnios): Indicates a normal or reassuring result, suggesting no immediate fetal compromise. No further testing might be required if the indication for testing has resolved. If the indication persists, consider weekly testing. For gestational ages ≥ 36 weeks, delivery is often advised. Below 36 weeks, surveillance or delivery is considered based on the clinical context.
- 6 Points: Represents an equivocal result, implying an unclear risk of fetal compromise. It's advisable to consult with an obstetric or maternal-fetal medicine specialist. The options may include repeating the BPP within 24 hours or proceeding to delivery, depending on the specific case and clinical judgment.
- ≤ 4 Points: Signals an abnormal result, raising concerns for potential fetal compromise. Immediate consultation with an obstetric or maternal-fetal medicine specialist is crucial. Delivery is usually recommended, though close monitoring might be an option if gestation is below 32 weeks.
- Oligohydramnios: The presence of oligohydramnios, regardless of the BPP score, may necessitate delivery or close monitoring due to the increased risk of fetal compromise.
- The follow-up actions based on the BPP scores are tailored to whether oligohydramnios is present and the total score obtained:
- The Modified Biophysical Profile
- It simplifies fetal well-being assessment by combining a Nonstress Test (NST) with ultrasound measurement of amniotic fluid volume
- Normal Results: A reactive NST (indicative of fetal well-being) combined with a DVP > 2 cm
- Abnormal Results: A nonreactive NST or a DVP ≤ 2 cm
- Further Evaluation: Abnormal MBPP results necessitate additional assessments to more comprehensively evaluate fetal health. This may involve a full Biophysical Profile (BPP) or a Contraction Stress Test (CST), depending on the clinical context and specific findings.
- Doppler Velocimetry: Specifically used in cases of suspected intrauterine growth restriction (IUGR), it assesses blood flow in the umbilical artery to evaluate fetal health.
Conclusion
Third-trimester fetal surveillance is a vital component of prenatal care, particularly in high-risk pregnancies. By employing various monitoring techniques, healthcare providers can better assess fetal health, make timely decisions to prevent adverse outcomes, and prepare for delivery.
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.