شرح المدرسين
Summary
The menstrual cycle is a complex, hormonally regulated process involving the hypothalamus, pituitary gland, and ovaries that prepares the female body for potential pregnancy. It typically lasts about 28 days. The cycle is divided into the ovarian (follicular, ovulation, and luteal phases) and uterine (menstrual, proliferative, and secretory phases) components. Physiological signs such as basal body temperature rise and cervical mucus changes accompany these phases. Mittelschmerz, or ovulation pain, is a common benign mid-cycle symptom experienced by many women, characterized by unilateral lower abdominal pain due to follicle rupture or peritoneal irritation. Diagnosis is clinical, and treatment is usually supportive with NSAIDs or hormonal suppression if needed.
Definition and Normal Parameters
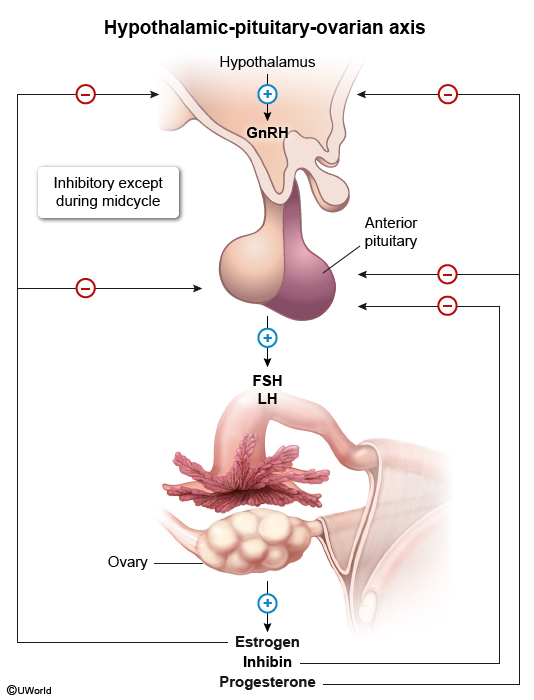
Definition: The menstrual cycle is a physiological process controlled by the hypothalamic-pituitary-ovarian (HPO) axis, designed to prepare the female reproductive system for pregnancy through coordinated hormonal regulation and tissue changes.
Normal Menstrual Cycle Parameters:
| Normal Menstrual Cycle Parameters - المعايير الطبيعية للدورة الشهرية | |
|---|---|
| Parameter | Normal Range |
| Cycle Length | 21–35 days (average 28 days) |
| Menstrual Flow Duration | 3–7 days (average 5 days) |
| Menstrual Volume | 5–80 mL per cycle (average 30–40 mL) |
| Cycle Variability | ≤ 7–9 days variation between cycles |
| Age of Menarche | 9–15 years (average 12–13 years) |
| Age of Menopause | 45–55 years (average 51 years) |
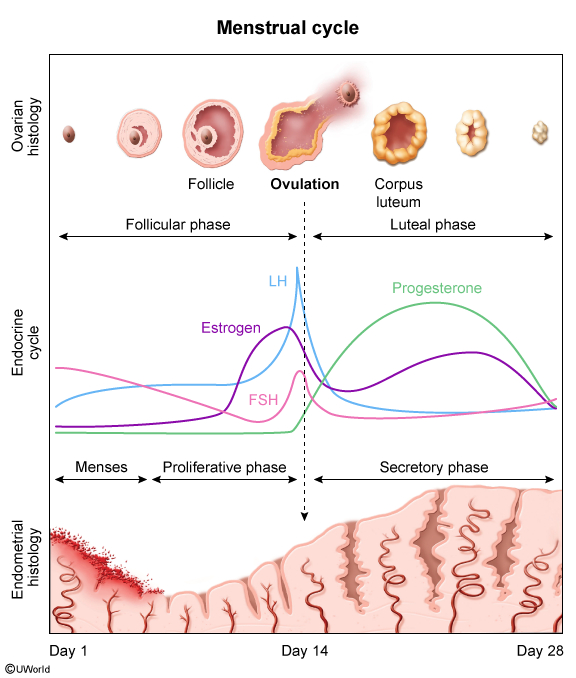
Hormonal Regulation
Hypothalamic-Pituitary-Ovarian (HPO) Axis:
- Hypothalamus
- Releases GnRH (Gonadotropin-Releasing Hormone) in pulsatile fashion
- GnRH pulse frequency determines FSH vs LH predominance
- Subject to positive and negative feedback from ovarian hormones
- Anterior Pituitary
- FSH (Follicle-Stimulating Hormone): Stimulates follicular development and estradiol production
- LH (Luteinizing Hormone): Triggers ovulation and corpus luteum formation
- LH surge occurs 24-36 hours before ovulation
- Ovaries
- Estradiol: Produced by granulosa cells, promotes endometrial proliferation
- Progesterone: Produced by corpus luteum, stabilizes endometrium
- Inhibin: Suppresses FSH secretion (negative feedback)
- Anti-Müllerian Hormone (AMH): Regulates follicular recruitment
| Hormonal Changes Throughout the Cycle - التغيرات الهرمونية | ||
|---|---|---|
| Phase | Dominant Hormone | Key Function |
| Early Follicular | ↑ FSH | Follicular recruitment and development |
| Late Follicular | ↑ Estradiol | Endometrial proliferation, LH surge trigger |
| Ovulation | ↑↑ LH | Follicle rupture, oocyte release |
| Luteal | ↑ Progesterone + Estradiol | Endometrial secretory changes |
| Menstrual | ↓ All hormones | Endometrial shedding |
Cycle Phases (Ovarian and Uterine)
Ovarian cycle:
- Follicular Phase (Day 1–13)
- This phase starts on the first day of menstruation and continues until ovulation, length of this phase may increase or decrease according to cycle length.
- The pituitary gland secretes follicle-stimulating hormone (FSH), prompting several ovarian follicles to begin developing; among these, usually only one follicle matures into a viable egg (oocyte).
- Estrogen levels begin to rise, promoting the regeneration of the uterine lining (endometrium).
- The hypothalamus releases gonadotropin-releasing hormone (GnRH) in pulses, which stimulates the anterior pituitary to secrete both FSH and luteinizing hormone (LH); which stimulate a group of antral follicles to grow.
- LH targets theca cells in the ovary to produce progesterone and androstenedione, which are converted into estradiol by granulosa cells under the influence of FSH; also FSH stimulates ovarian granulosa cells to produce inhibin.
- Estradiol and inhibin produced by granulosa cells provide negative feedback, reducing FSH secretion.
- As FSH levels drop, most follicles regress, leaving only the dominant follicle to continue maturing.
- This dominant follicle releases increasing amounts of estradiol, which eventually shifts the feedback loop in the hypothalamus and pituitary gland from negative to positive, causing a sharp rise in LH levels known as the LH surge.
- Ovulation Phase (Day 14)
- A surge in LH (luteinizing hormone) triggers the release of the mature egg from the ovary.
- Peak fertility period: 3 days before to 1 day after ovulation
- Luteal Phase (always 14 days after ovulation)
- After ovulation, the empty follicle transforms into the corpus luteum, which secretes progesterone and some estradiol.
- Progesterone stabilizes and thickens the endometrium, preparing it for potential embryo implantation.
- These hormones again suppress the release of FSH and LH through negative feedback.
- If fertilization does not occur, LH levels fall, leading to degeneration of the corpus luteum.
- As the corpus luteum breaks down, progesterone and estradiol levels decline; the drop in these hormones removes the suppression of GnRH, FSH, and LH, and the cycle restarts with the beginning of a new follicular phase and menstruation.
Uterinen cycle:
- Menstrual phase (day 1 to approximate day 5)
- This phase marks the beginning of the cycle and is when menstruation (bleeding) occurs.
- The uterus sheds the thickened endometrial lining from the previous cycle due to the absence of pregnancy.
- As the corpus luteum degenerates, the levels of progesterone and estradiol reach their lowest point.
- This hormonal decline causes vasoconstriction (narrowing) of the spiral arteries in the endometrium, leading to reduced blood flow (ischemia) and programmed cell death (apoptosis) in the functional layer of the endometrium.
- These processes result in the breakdown and shedding of the uterine lining, which exits the body as menstrual blood.
- Proliferative phase of the menstrual cycle (approx. day 5–14):
- Triggered by rising levels of estradiol produced by developing ovarian follicles.
- The endometrial lining begins to regenerate, rebuilding the tissue that was shed during menstruation.
- Uterine spiral arteries start to grow back, extending about two-thirds into the endometrium.
- Stromal cells (supporting cells of the uterus) multiply, enlarge, and store glycogen.
- Endometrial glands become long, straight, and tubular, lined with simple columnar epithelium.
- The functional zone of the endometrium is rebuilt through active cell proliferation and high mitotic activity.
- This phase typically lasts around 14 days, during which the endometrial tissue thickens and prepares for potential implantation.
- Secretory phase (approx. day 14–28):
- Begins after ovulation, as the corpus luteum forms and releases high levels of progesterone.
- Progesterone induces the differentiation of endometrial tissue, preparing it for possible implantation of a fertilized egg (blastocyst).
- Stromal cells become swollen with fluid (edematous), and spiral arteries now reach the full depth of the endometrium.
- Endometrial glands become more twisted (tortuous) and begin producing glycogen-rich secretions to nourish the potential embryo.
- Basal body temperature slightly increases during this phase.
- Cervical mucus becomes more abundant and protective, creating a barrier against foreign substances, including sperm.
| Important – فكرة سؤال | |
| The luteal phase is always 14 days in normal cycles. Cycle length variations occur due to changes in the follicular phase duration. This is crucial for exam questions about cycle timing and ovulation prediction. | تذكر |
Mittelschmerz
Definition: also known as ovulation pain, is a unilateral mild to moderate lower abdominal pain that occurs mid-cycle, typically between days 7 and 24 of the menstrual cycle, corresponding with ovulation. It is a benign condition and affects more than 40% of women of reproductive age, often recurring monthly.
Epidemiology:
- Occurs at least once in over 50% of premenopausal individuals.
- Most common in women with regular menstrual cycles
Etiology:
- Exact cause is unclear,
- Proposed etiologies include:
- Rupture of the dominant follicle or follicular cyst
- Spasms of the fallopian tubes or uterus
- Peritoneal irritation from the release of follicular fluid or a small amount of blood
Clinical Features
- Timing: Days 14-16 of 28-day cycle (can occur days 7-24)
- Location: Unilateral iliac fossa (alternates between ovaries)
- Character: Sharp, cramping, or dull aching pain
- Duration: Minutes to 48 hours (typically <24 hours)
- Severity: Mild to moderate intensity
- Associated symptoms:
- Light spotting or discharge
- Nausea (if severe)
- Bloating sensation
Diagnosis
- Primarily a clinical diagnosis based on timing, symptoms, and history
- If uncertain, lab tests or pelvic ultrasound may be used to exclude more serious conditions (e.g., appendicitis, ovarian torsion)
- Ultrasound may reveal:
- A small amount of free fluid in the pelvis
- Increased echogenicity in the ovary (suggesting recent ovulation)
Management and Treatment
- Most cases are self-limiting and require no specific treatment
- Non-opioid analgesics (e.g., NSAIDs) can relieve discomfort
- Hormonal suppression (for recurrent severe pain):
- Combined oral contraceptive pills
- Suppresses ovulation, prevents mittelschmerz
- Consider for women not trying to conceive
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.