شرح المدرسين
Summary
Abnormal Uterine Bleeding (AUB) is a common gynecological condition characterized by deviations in menstrual frequency, regularity, duration, or volume, often seen in adolescents and perimenopausal women. The FIGO PALM-COEIN system classifies AUB into structural causes (polyps, adenomyosis, leiomyomas, malignancy) and non-structural causes (coagulopathies, ovulatory dysfunction, endometrial issues, iatrogenic factors, and unclassified etiologies). Clinical manifestations include heavy or irregular bleeding, postcoital or postmenopausal bleeding, and amenorrhea. Evaluation involves a detailed history, physical exam, lab tests (e.g., β-hCG, TSH, CBC), and imaging (especially transvaginal ultrasound), with biopsies or hysteroscopy when indicated. Management is typically medical—using hormonal or non-hormonal therapies—with surgical options reserved for refractory cases or specific structural pathologies. Age-specific considerations and a shift to standardized FIGO terminology enhance diagnostic accuracy and treatment planning.
Definition
Abnormal Uterine Bleeding (AUB) refers to any deviation from normal menstrual cycle parameters in terms of:
- Frequency: Normal cycle is 24-38 days
- Regularity: Variation of ≤2-20 days between cycles
- Duration: Normal bleeding lasts ≤8 days
- Volume: Normal menstrual blood loss <80 mL per cycle
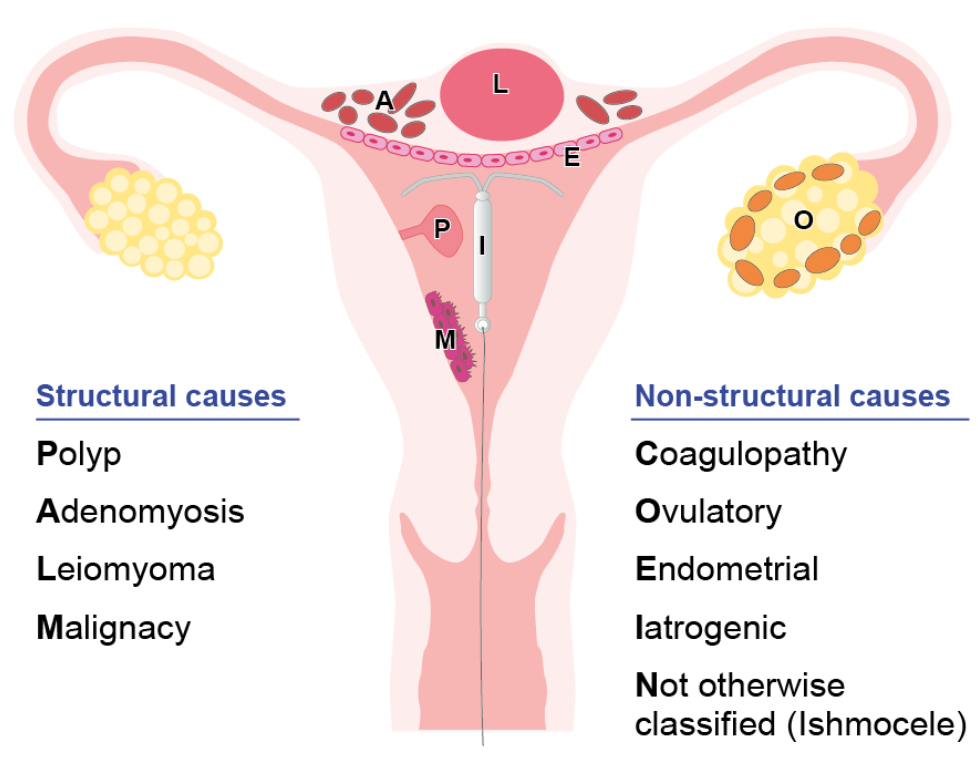
Causes - FIGO Classification of AUB (PALM-COEIN System)
Causes of AUB can be categorized into structural and nonstructural factors, which are classified using the PALM-COEIN system.
Structural causes: PALM- Polyp: endometrial or cervical polyps; typically causes intermenstrual bleeding
- Adenomyosis: endometrial glands and stroma within the myometrium; causes painful, heavy menses
- Leiomyoma (fibroids): benign smooth muscle tumors of the uterine myometrium; causes heavy, prolonged bleeding
- Malignancy and hyperplasia (endometrial hyperplasia/cancer): uncontrolled endometrial proliferation; causes irregular and/or heavy bleeding
- Coagulopathy (eg, von Willebrand disease, thrombocytopenia): results in heavy bleeding
- Ovulatory dysfunction: anovulation or irregular ovulation (eg, polycystic ovary syndrome [PCOS], thyroid disorder, hypothalamic amenorrhea); causes amenorrhea or irregular menses
- Endometrial: disorders that affect the endometrial lining (eg, endometritis, intrauterine adhesions); causes irregular bleeding
- Iatrogenic: medications that can cause abnormal bleeding (eg, contraceptive pills or devices, anticoagulants)
- Not yet classified: causes that do not fit into the previous categories
Clinical Manifestations
- Heavy menstrual bleeding (formerly menorrhagia)
- Intermenstrual bleeding (formerly metrorrhagia)
- Prolonged or shortened cycles (polymenorrhea, oligomenorrhea)
- Postcoital bleeding
- Amenorrhea followed by irregular bleeding
Evaluation and Diagnosis
- History and Physical Exam
- Menstrual, sexual, and reproductive history
- Medication and family history
- Systemic signs (e.g., fatigue, weight changes, hirsutism)
- Pelvic and thyroid examination
- Initial Laboratory Work-up
- Pregnancy test (β-hCG): Mandatory in reproductive-age patients
- CBC & Ferritin: Assess anemia and iron deficiency
- TSH & Prolactin: Evaluate thyroid and pituitary function
- Hormonal profile: FSH, LH, estradiol, androgens if indicated
- Coagulation profile: If bleeding disorder suspected
- Imaging and Procedures
- Transvaginal Ultrasound (TVUS): First-line imaging for structural abnormalities
- Endometrial Biopsy: For women ≥ 45 or younger with risk factors (e.g., obesity, diabetes, anovulation, persistent AUB)
- Hysteroscopy: Direct visualization and management of intrauterine pathology
- Advanced Imaging (MRI, CT): For suspected pituitary or adrenal pathology
Biopsy
An endometrial biopsy () is not indicated in all cases of AUB, but it is performed in patients with suspected endometrial hyperplasia and/or cancer. Indications include:
- Age ≥45 with AUB (ie, the risk of endometrial cancer increases with age)
- Age <45 with AUB plus:
- Unopposed estrogen (eg, obesity, PCOS)
- Failed medical management
- Lynch syndrome
- Age ≥35 with atypical glandular cells on Pap test (ie, the atypical cells can be of endocervical or endometrial origin)
Management
- Medical Therapy (First-line for Most Patients)
- Hormonal:
- Combined Oral Contraceptives (COCs)
- Progestins (oral, depot, or IUD)
- Levonorgestrel-releasing IUD (LNG-IUS)
- GnRH agonists for short-term use in severe cases
- Non-Hormonal:
- NSAIDs (e.g., ibuprofen, mefenamic acid)
- Tranexamic Acid
- Iron supplementation
- Hormonal:
- Surgical Interventions
- Polypectomy/Myomectomy: For symptomatic polyps or fibroids
- Endometrial Ablation: For refractory AUB not desiring fertility
- Dilation and Curettage (D&C): Diagnostic and therapeutic in acute cases
- Uterine Artery Embolization (UAE): For fibroid-related bleeding
- Hysterectomy: Definitive management when all other measures fail
Special Considerations by Age Group
- Newborns: Maternal estrogen withdrawal—self-limited
- Children: Precocious puberty, foreign bodies, rare tumors
- Adolescents: Often due to anovulation or coagulopathies (e.g., von Willebrand disease)
- Reproductive age: Pregnancy-related causes, DUB, contraceptive side effects
- Perimenopausal/Postmenopausal: Must rule out malignancy (e.g., endometrial carcinoma, cervical cancer)
Terminology Update by FIGO
Old terms such as menorrhagia, metrorrhagia, and dysfunctional uterine bleeding have been replaced by more precise FIGO nomenclature. AUB is now categorized by:
- Bleeding pattern: Frequency, regularity, duration, volume
- Etiology: Via PALM-COEIN classification
- Chronicity: Acute vs. chronic AUB
- Ovulatory status: Ovulatory vs. anovulatory AUB.
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.