شرح المدرسين
Summary
Dysmenorrhea, or painful menstruation, is one of the most common gynecological complaints among menstruating individuals, particularly adolescents and young women. It significantly impacts quality of life, school attendance, and work productivity. Dysmenorrhea is broadly classified into two types: primary and secondary, based on the presence or absence of underlying pelvic pathology.
Dysmenorrhea
Definition: Dysmenorrhea refers to crampy lower abdominal and pelvic pain associated with menstruation. It may be accompanied by systemic symptoms such as nausea, vomiting, fatigue, diarrhea, and headache. The pain is typically cyclic and occurs around the time of menstruation.
Types of Dysmenorrhea
- Primary Dysmenorrhea
- Definition: menstrual pain without an identifiable pelvic pathology. It is the most prevalent type and usually begins within 1–2 years of menarche, corresponding to the establishment of ovulatory cycles.
- Pathogenesis: It results from increased endometrial prostaglandin (especially PGF₂α) production during the late luteal phase, following the drop in progesterone. This leads to:
- Hyperactive uterine contractions
- Uterine vasoconstriction and ischemia
- Systemic symptoms such as GI disturbances due to smooth muscle stimulation
- Risk Factors:
- Early menarche
- Nulliparity
- Smoking
- High stress
- Family history
- Clinical Features:
- Crampy, midline lower abdominal pain
- Onset: 6–12 hours before menstruation
- Peak: First 24–48 hours of menstruation
- Duration: Typically lasts 8–72 hours
- Often improves after childbirth or with age
- Associated symptoms: Nausea, vomiting, diarrhea, fatigue, sleep disturbances, muscle cramps
- Secondary Dysmenorrhea
- Definition: menstrual pain caused by identifiable pelvic pathology, typically emerging after the age of 25 and increasing with age.
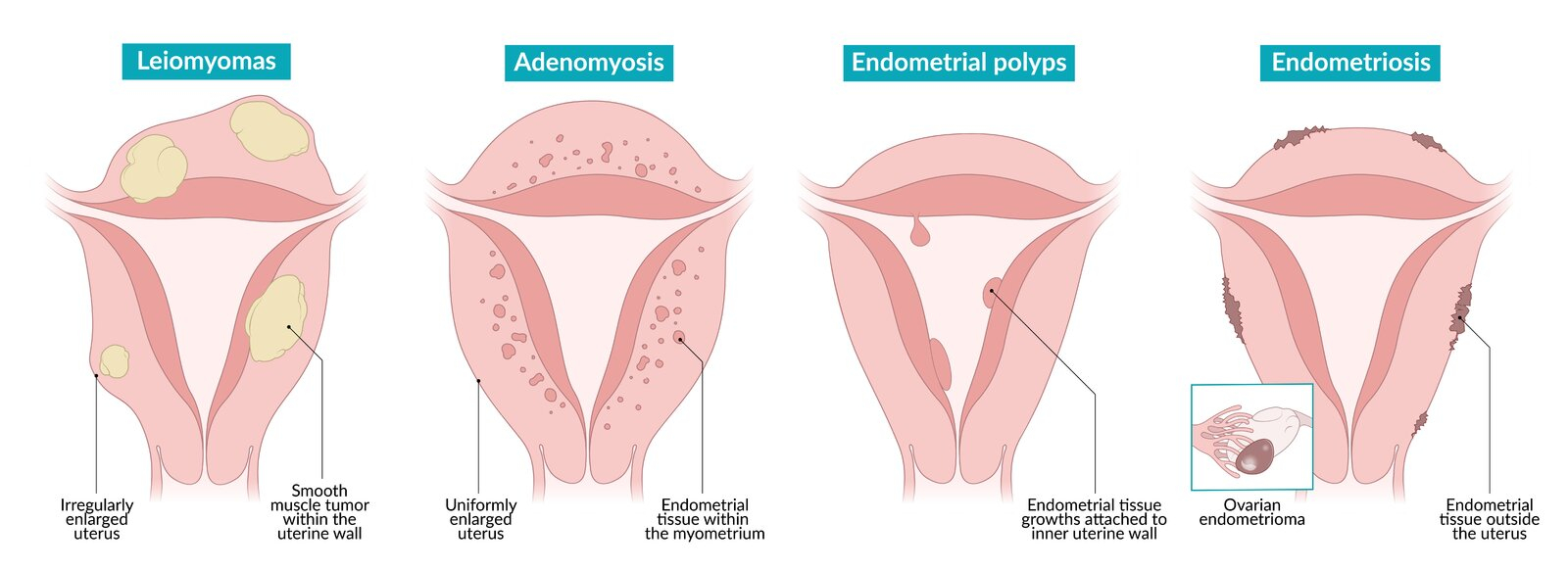
- Common Causes:
- Endometriosis (most common)
- Adenomyosis
- Uterine fibroids
- Chronic pelvic inflammatory disease (PID)
- Copper intrauterine device (IUD)
- Congenital anomalies (e.g., imperforate hymen, transverse vaginal septum)
- Pelvic adhesions or intrauterine adhesions (Asherman's syndrome)
- Clinical Features:
- Pain begins before menstruation and may persist throughout or after
- Not limited to menstruation
- Often unilateral and non-cyclic
- May include dyspareunia, infertility, or heavy menstrual bleeding
- Typically no GI symptoms such as nausea or vomiting
Differential Diagnosis of Menstrual-Related Pain
| Condition | Onset of Pain | Peak | Resolution |
|---|---|---|---|
| Primary Dysmenorrhea | Just before menstruation | Day 1–2 of menses | Within 2–3 days |
| Endometriosis | 1–2 weeks before menstruation | 1–2 days before menses | By day 2 of menses |
| Adenomyosis | 1 week before menstruation | During menses | At the end of menstruation |
| PMS/PMDD | 1–2 weeks before menstruation | Before menses | At onset or day 2 of menses |
Diagnostic Approach
Primary Dysmenorrhea
- Clinical diagnosis based on typical history in adolescents and young women
- No pelvic exam or imaging is required in classic presentations
- Rule out pregnancy with urine hCG test in those of reproductive age
Secondary Dysmenorrhea
- Detailed history and physical exam focusing on menstrual patterns, pain characteristics, and sexual history
- Pelvic ultrasound: First-line imaging to evaluate structural abnormalities
- STI screening: Especially in sexually active individuals (e.g., NAAT for Chlamydia/Gonorrhea)
- Laparoscopy: Gold standard for diagnosing endometriosis
- Additional tests as needed:
- CBC for suspected infection
- Urinalysis for urinary tract involvement
Management
- Primary Dysmenorrhea
- Initial Therapy:
- NSAIDs: First-line treatment (e.g., ibuprofen, naproxen); start 1–2 days before menses and continue for 2–3 days
- Hormonal contraception:
- Combined hormonal contraceptives (CHCs)
- Progestin-only methods (e.g., pills, IUDs, implants)
- Non-Pharmacologic Options:
- Local heat therapy (e.g., heating pads)
- Regular physical exercise
- TENS (Transcutaneous Electrical Nerve Stimulation)
- Note: Opioids are not recommended for primary dysmenorrhea
- Initial Therapy:
- Secondary Dysmenorrhea
- Treat the underlying condition
- If initial evaluation is inconclusive: referral to obstetrics/gynecology for further imaging or laparoscopy
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.