Summary
Amenorrhea is the absence of menstrual periods and is classified as either primary, or secondary. It can result from physiological causes such as pregnancy; structural abnormalities like imperforate hymen; ovulatory dysfunction including ovarian insufficiency or hypothalamic issues; central nervous system disorders affecting the hypothalamic-pituitary axis; endocrine conditions like hyperprolactinemia or thyroid disease; and hyperandrogenic states such as PCOS or adrenal tumors. Evaluation involves ruling out pregnancy, assessing hormone levels, and performing targeted imaging. Management depends on the underlying cause and may include lifestyle modification, hormonal therapy, or surgical intervention, with goals focused on restoring menstrual function, supporting fertility, and preventing complications like osteoporosis.
Definition
Definition: Failure to menstruate by age 15 years in the presence of normal secondary sexual characteristics, or by age 13 years in the absence of secondary sexual characteristics. It is categorized into:
- Primary Amenorrhea: The absence of menarche (first menstrual period) by age 15, or more than 5 years after thelarche (breast development), whichever comes first.
- Secondary Amenorrhea: The cessation of menstruation for:
- More than 3 months in individuals with previously regular cycles
- More than 6 months in individuals with previously irregular cycles
Causes
Etiology: Amenorrhea can result from a wide range of causes, grouped broadly into physiological, structural, hormonal, and functional origins.
- Physiological Causes: These are normal life-stage processes that result in amenorrhea:
- Pregnancy (most common cause)
- Lactation
- Menopause
- Constitutional delay of growth and puberty
- Structural/Reproductive Tract Abnormalities: Obstruction or malformation of the genital tract may lead to amenorrhea:
- Imperforate hymen
- Transverse vaginal septum
- Agenesis of the lower vagina
- Müllerian agenesis (MRKH syndrome)
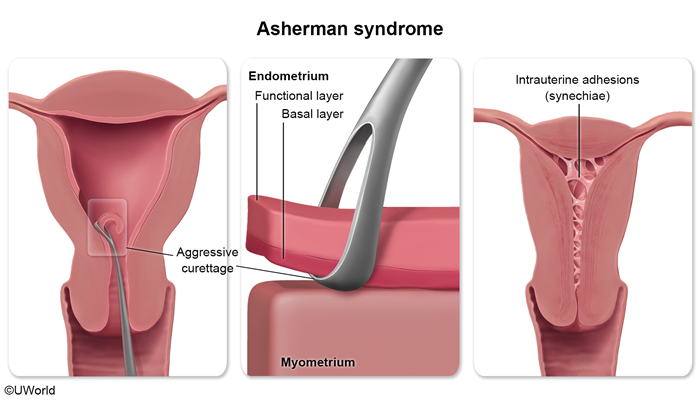
- Uterine adhesions (e.g., Asherman syndrome)
- Cervical stenosis
- Disorders of sex development in individuals with 46,XY karyotype:
- Androgen insensitivity syndrome (AIS)
- 5α-reductase deficiency
- 17α-hydroxylase deficiency
- Ovulatory Dysfunction: Amenorrhea may occur when ovulation is irregular or absent:
- Primary ovarian insufficiency (hypergonadotropic hypogonadism)
- Secondary ovarian insufficiency (hypothalamic or pituitary dysfunction → hypogonadotropic hypogonadism)
- Functional hypothalamic amenorrhea due to:
- Stress
- Weight loss
- Excessive exercise
- Eating disorders
- Central Nervous System (CNS) Disorders: Pathologies affecting the hypothalamus or pituitary may impair GnRH, LH, or FSH secretion:
- Injury (e.g., TBI, radiation)
- Infiltrative diseases (e.g., sarcoidosis, hemochromatosis)
- Infections (e.g., meningitis, tuberculosis)
- Ischemic events (e.g., Sheehan syndrome)
- Congenital disorders (e.g., Kallmann syndrome with anosmia)
- Endocrine Disorders:
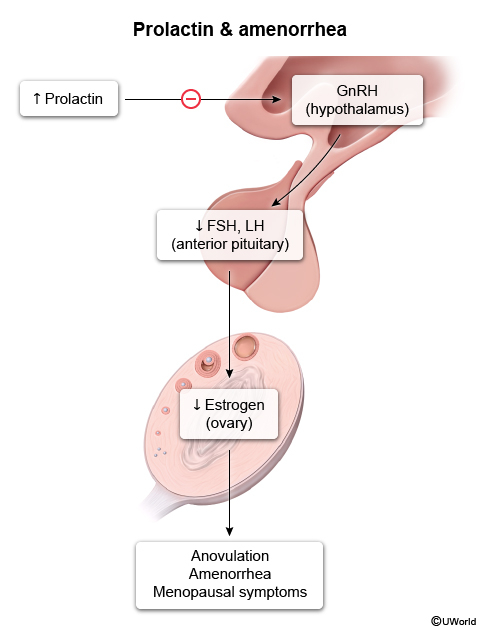
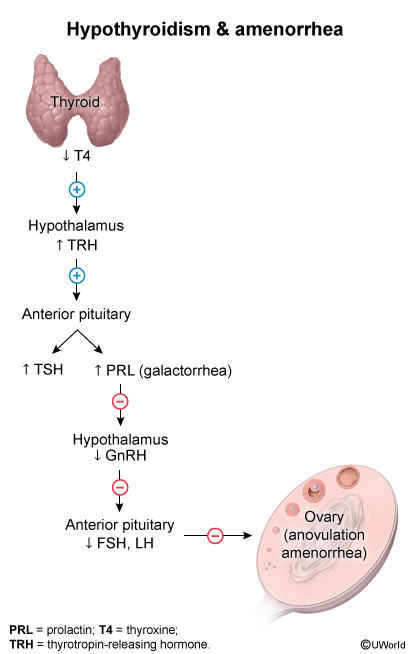
- Hyperprolactinemia (e.g., pituitary adenoma, antipsychotics, hypothyroidism, CKD)
- Cushing syndrome
- Thyroid dysfunction (hypo- or hyperthyroidism)
- Chronic liver disease
- Medication-related amenorrhea (e.g., hormonal contraceptives)
- Hyperandrogenic Conditions:
- Polycystic ovary syndrome (PCOS)
- Congenital adrenal hyperplasia
- Androgen-secreting tumors
- Obesity, which may exacerbate hormonal imbalances
Diagnostic Approach
- Step 1: Rule Out Pregnancy
- A pregnancy test should be the first investigation in all cases of secondary amenorrhea
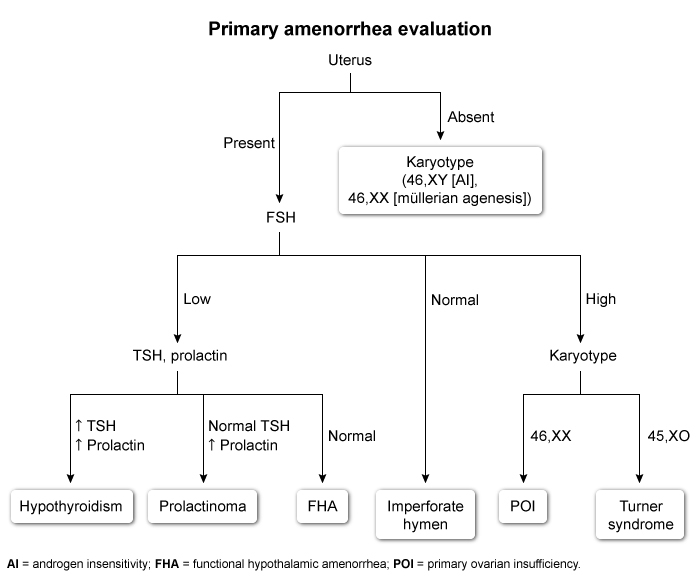
- Primary Amenorrhea Workup
- Pelvic exam:
- Cervix present (uterus visualized): Measure FSH ± estradiol
- FSH ↓ or normal:
- Absent breasts → consider constitutional delay or GnRH deficiency (e.g., Kallmann syndrome)
- Present breasts → evaluate as secondary amenorrhea
- FSH ↑: Perform karyotyping (e.g., Turner syndrome)
- FSH ↓ or normal:
- Blind/absent vagina: Perform pelvic ultrasound
- If uterus absent → check karyotype and testosterone levels
- If uterus present → consider outflow tract anomalies (e.g., imperforate hymen)
- Cervix present (uterus visualized): Measure FSH ± estradiol
- Pelvic exam:
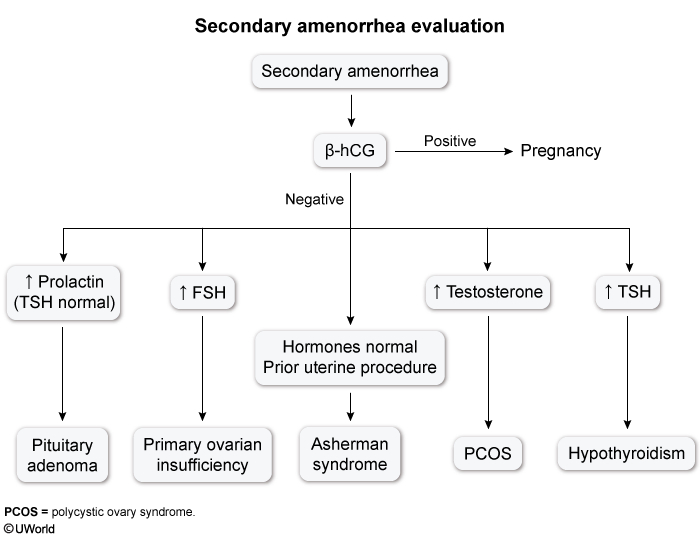
- Secondary Amenorrhea Workup
- Initial labs:
- FSH, LH
- Estradiol, ± AMH
- Prolactin
- TSH
- Targeted testing (based on clinical signs):
- Hyperandrogenism: Total/free testosterone, DHEA-S, 17-hydroxyprogesterone
- Estrogen deficiency: FSH, LH, estradiol
- Hyperprolactinemia: Prolactin
- Adrenal/Cushing: Cortisol, dexamethasone suppression test
- Chronic illness: CBC, ESR/CRP, metabolic panel
- GI/weight loss: Celiac disease serologies
- Imaging:
- Pelvic ultrasound: Assess ovaries, uterus (PCOS, uterine anomalies)
- Brain MRI: For suspected pituitary tumors or hyperprolactinemia
- Adrenal imaging: If androgen-secreting tumor suspected
- Initial labs:
- Hormonal Challenge Tests
Used in secondary amenorrhea if initial workup is inconclusive.
- Progestin Challenge Test:
- Administer progestin for 5–10 days
- Withdrawal bleeding → suggests anovulation (e.g., PCOS)
- No bleeding → suggests hypoestrogenism or outflow obstruction
- Estrogen-Progestin Challenge Test:
- Estrogen given for 21–25 days; progestin added during final 5–10 days
- Withdrawal bleeding → suggests hypoestrogenism
- No bleeding → suggests outflow tract issue or endometrial scarring (e.g., Asherman syndrome)
- Progestin Challenge Test:
Management
- Goals
- Initiate and complete puberty (in primary amenorrhea)
- Prevent long-term complications (e.g., osteoporosis)
- Address fertility and reproductive health
- Treat the underlying cause
- Treatment Options
- Lifestyle modification: Nutritional support, reduce exercise/stress (functional hypothalamic amenorrhea)
- Hormonal therapy:
- Combined oral contraceptives (for PCOS or hypoestrogenism)
- Hormone replacement therapy (HRT) for premature ovarian insufficiency
- Dopamine agonists (e.g., bromocriptine, cabergoline) for prolactinoma
- Surgery: For structural anomalies, tumors, or outflow tract obstruction
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.