Summary
Amenorrhea, the absence of menstruation, can result from a variety of syndromic conditions involving genetic, endocrine, structural, or iatrogenic factors. This article reviews key syndromes associated with amenorrhea—including Turner Syndrome, Androgen Insensitivity Syndrome, Kallmann Syndrome, PCOS, Sheehan Syndrome, Asherman Syndrome, MRKH Syndrome, and others—highlighting their etiologies, clinical features, diagnostic approaches, and management strategies. Understanding these conditions is essential for accurate diagnosis, effective treatment, and fertility counseling, as many of these syndromes have significant implications for reproductive and overall health.
Overview
- Amenorrhea is defined as the absence of menstruation and can be classified as:
- Primary amenorrhea: Failure to menstruate by age 15 years in the presence of normal secondary sexual characteristics, or by age 13 years in the absence of secondary sexual characteristics
- Secondary amenorrhea: Absence of menses for 3 months in women with previously normal menstruation, or 6 months in women with previous oligomenorrhea
- Multiple syndromes can present with amenorrhea, each with distinct underlying pathophysiology
- Accurate diagnosis requires careful history, physical examination, hormonal evaluation, karyotyping when indicated, and imaging studies
- Understanding these syndromes is essential for proper management, fertility counseling, and addressing associated comorbidities
انقطاع الطمث يمكن أن يكون أولي أو ثانوي، وكل متلازمة لها خصائص مميزة. معرفة هذه المتلازمات مهمة جداً للامتحانات وللممارسة السريرية
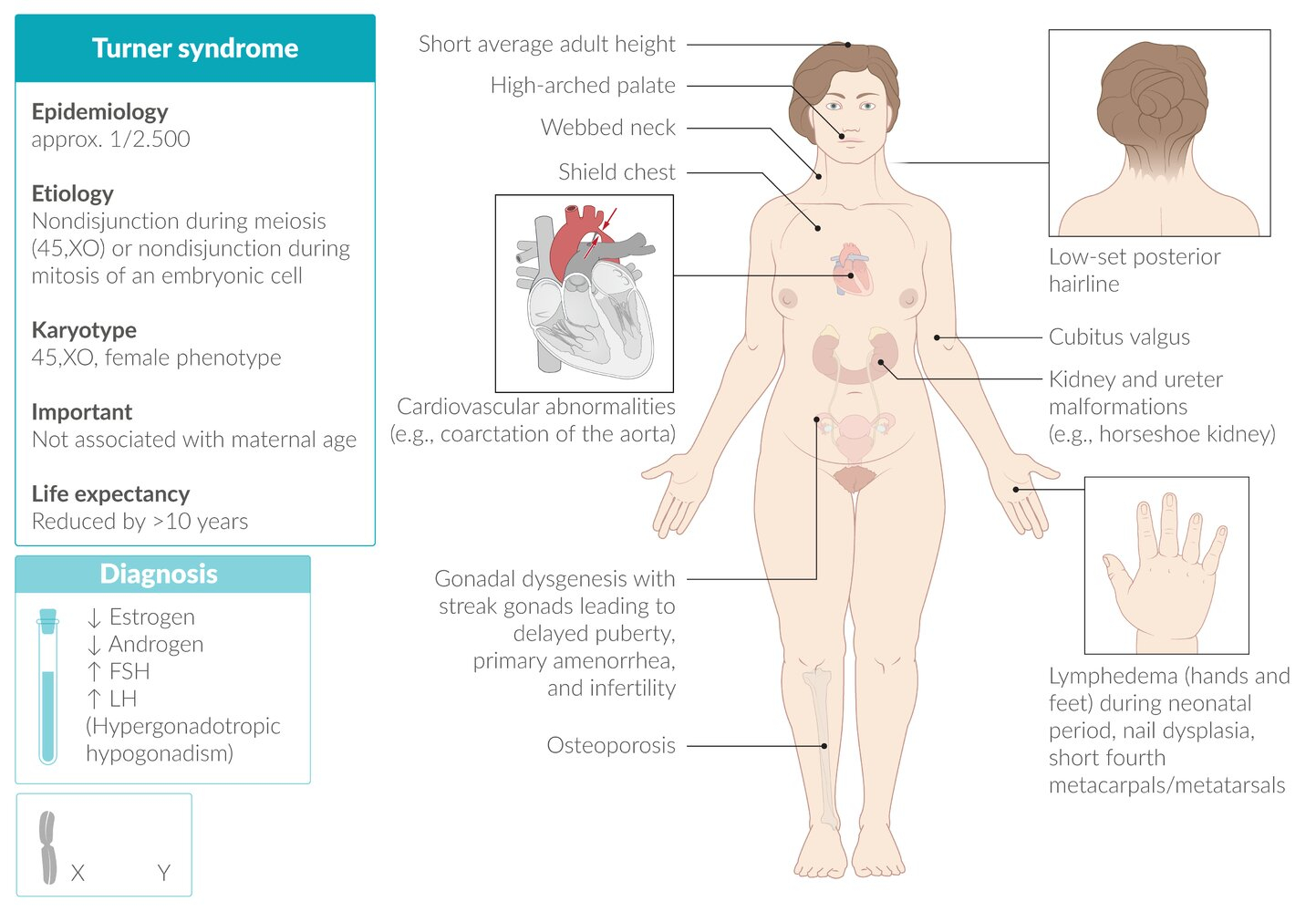
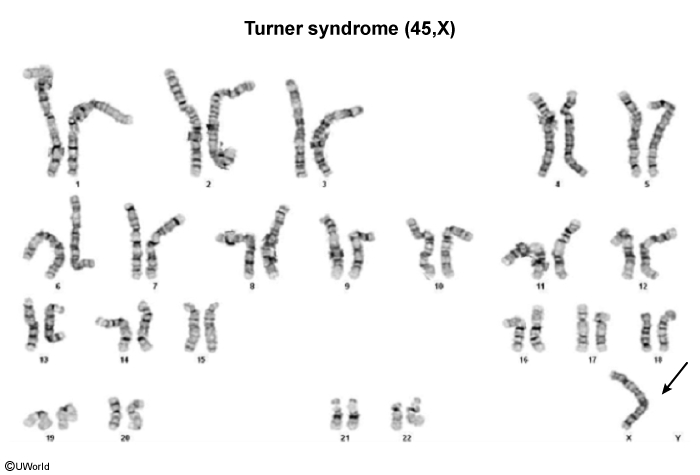
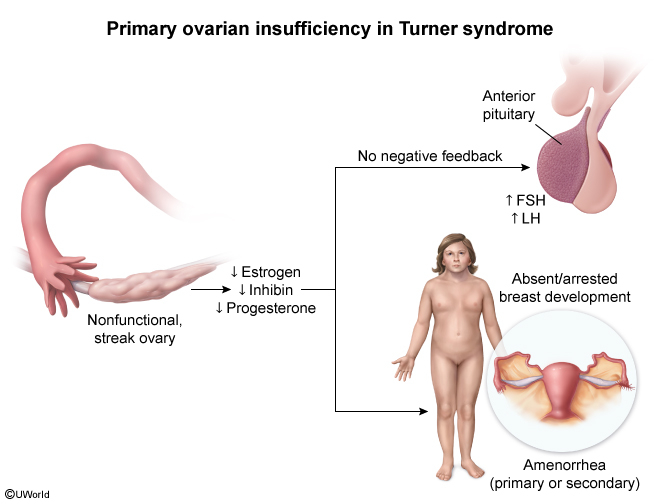
1. Turner Syndrome (45,X)
- Type: Primary amenorrhea
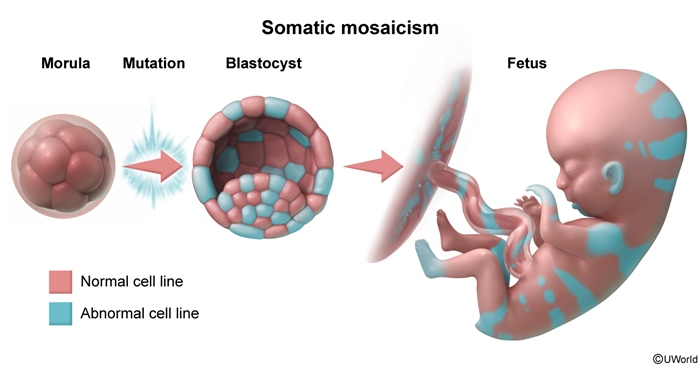
- Karyotype: 45,X (complete monosomy) or mosaic variants (45,X/46,XX)
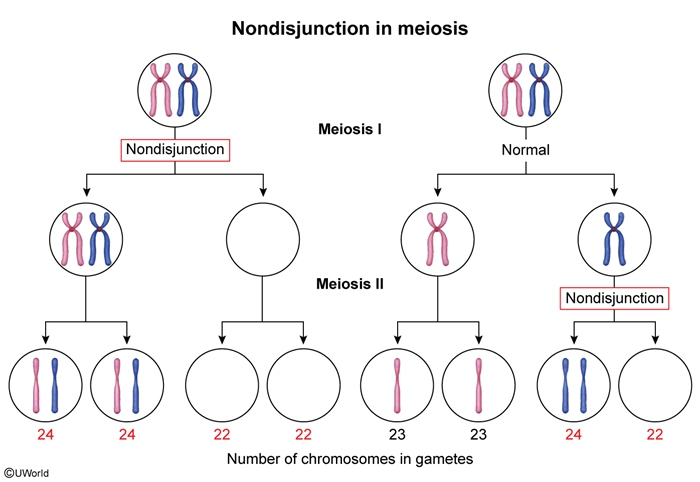
- Pathophysiology:
- Gonadal dysgenesis results in streak ovaries
- Absent or minimal estrogen production
- Leads to hypergonadotropic hypogonadism
Clinical Features
- Growth and stature:
- Short stature (most consistent feature) قصر القامة - من أهم العلامات
- Average adult height: 143-145 cm without treatment
- Neck abnormalities:
- Webbed neck (pterygium colli) رقبة مجنحة
- Low posterior hairline
- Chest abnormalities:
- Shield chest with widely spaced nipples
- Reproductive features:
- Primary ovarian insufficiency (streak ovaries) (figure)
- Delayed or absent puberty
- Primary amenorrhea
- Infertility
- Cardiovascular anomalies:
- Coarctation of the aorta (most common)
- Bicuspid aortic valve (figure)
- Aortic dilation
- Renal anomalies:
- Horseshoe kidney (figure)
- Renal agenesis
- Other features:
- Lymphedema of hands and feet in newborns (figure)
- Cubitus valgus (increased carrying angle) (figure)
- Multiple pigmented nevi
Diagnosis
- Hormonal profile:
- Elevated FSH and LH (hypergonadotropic hypogonadism) → مهم جداً
- Low estradiol
- Confirmatory test: Karyotyping showing 45,X (gold standard)
- Imaging studies:
- Echocardiogram: to evaluate cardiac anomalies
- Renal ultrasound: to detect renal malformations
- Pelvic ultrasound: streak ovaries, small uterus
Management
- Growth hormone therapy: Started in early childhood to improve final adult height
- Estrogen replacement:
- Initiated at age of puberty (11-12 years) to induce secondary sexual characteristics
- Low-dose estrogen initially, gradually increased
- Progesterone: Added cyclically after estrogen priming to induce withdrawal bleeding and protect endometrium
- Fertility: IVF with donor oocytes is the only option for pregnancy
- Regular monitoring:
- Cardiovascular surveillance
- Thyroid function (increased risk of hypothyroidism)
- Bone density
| Important – فكرة سؤال | |
|
A 15-year-old girl presents with short stature and absence of menstruation. On examination, she has a webbed neck and widely spaced nipples. The most likely diagnosis is Turner syndrome. The confirmatory test is karyotyping, and you will find elevated FSH and LH levels. السؤال النموذجي عن Turner syndrome: فتاة 15 سنة قصيرة القامة، لم تأتها الدورة الشهرية، رقبة مجنحة، تباعد الحلمات. الفحص التأكيدي هو الــ Karyotyping، وتكون الهرمونات FSH و LH مرتفعة |
تذكر |
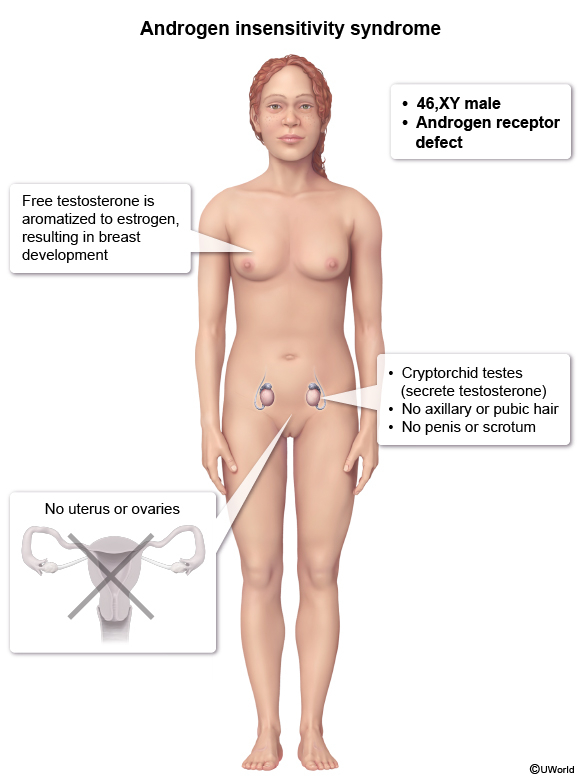
2. Androgen Insensitivity Syndrome (AIS)
Androgen Insensitivity Syndrome (AIS)
- Type: Primary amenorrhea in phenotypically female individuals
- Genetics: X-linked recessive mutation in androgen receptor gene
- Karyotype: 46,XY (genetically male)
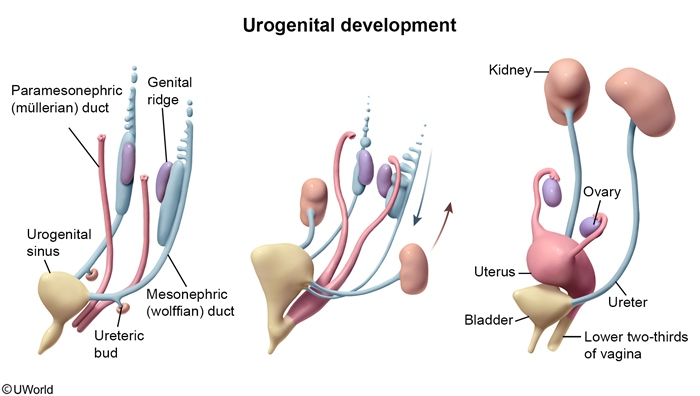
- Pathophysiology:
- End-organ resistance to androgens despite normal or elevated testosterone levels
- Testes produce testosterone and anti-Müllerian hormone (AMH)
- AMH causes regression of Müllerian structures (uterus, fallopian tubes, upper vagina)
- Due to androgen resistance, external genitalia develop along female lines
- Peripheral conversion of testosterone to estrogen leads to breast development
Clinical Features
- External appearance:
- Female external genitalia رغم أن الكروموسومات XY
- Blind vaginal pouch (vagina ends blindly) مهبل أعمى أو قصير
- Normal breast development at puberty (due to estrogen from peripheral conversion)
- Absent structures:
- No uterus, no cervix, no upper vagina
- No fallopian tubes
- Hair distribution:
- Sparse or absent pubic and axillary hair قلة شعر العانة وتحت الإبط - علامة مهمة
- Gonads:
- Undescended testes (located in inguinal canal or abdomen)
- May present as inguinal hernia in childhood or adolescence
- At presentation:
- Primary amenorrhea despite normal breast development
- Unable to have intercourse due to short vagina
Diagnosis
- Karyotype: 46,XY (diagnostic)
- Hormonal profile:
- Elevated or normal testosterone (male range)
- Elevated LH
- Normal or elevated estrogen (from peripheral conversion)
- Pelvic imaging (ultrasound or MRI):
- Absence of uterus and upper vagina
- May identify intra-abdominal or inguinal testes
- Physical examination: Blind vaginal pouch on speculum exam
Management
- Gonadectomy (removal of testes):
- Recommended after puberty is complete (to allow natural breast development)
- Reason: High risk of malignancy (gonadoblastoma, dysgerminoma) - around 30% if left in place
- Hormone replacement therapy:
- Estrogen therapy after gonadectomy to maintain secondary sexual characteristics and bone health
- Vaginal management:
- Vaginal dilation therapy (Frank method): non-surgical, gradual stretching
- Surgical reconstruction (vaginoplasty) if dilation fails or not desired
- Psychological support: Essential for gender identity and sexual health counseling
- Fertility: Not possible; patient is infertile
| Important – فكرة سؤال | |
|
A 16-year-old phenotypically female patient presents with primary amenorrhea. She has well-developed breasts but very little pubic and axillary hair. Pelvic ultrasound shows absence of uterus. Karyotype reveals 46,XY. Diagnosis: Androgen Insensitivity Syndrome. Key features: XY karyotype + female appearance + no uterus + sparse body hair. العلامات المميزة: فتاة بمظهر طبيعي، ثدي متطور، لكن شعر العانة قليل جداً، غياب الرحم، والكروموسومات 46,XY. يجب إزالة الخصيتين بعد البلوغ لتجنب السرطان |
تذكر |
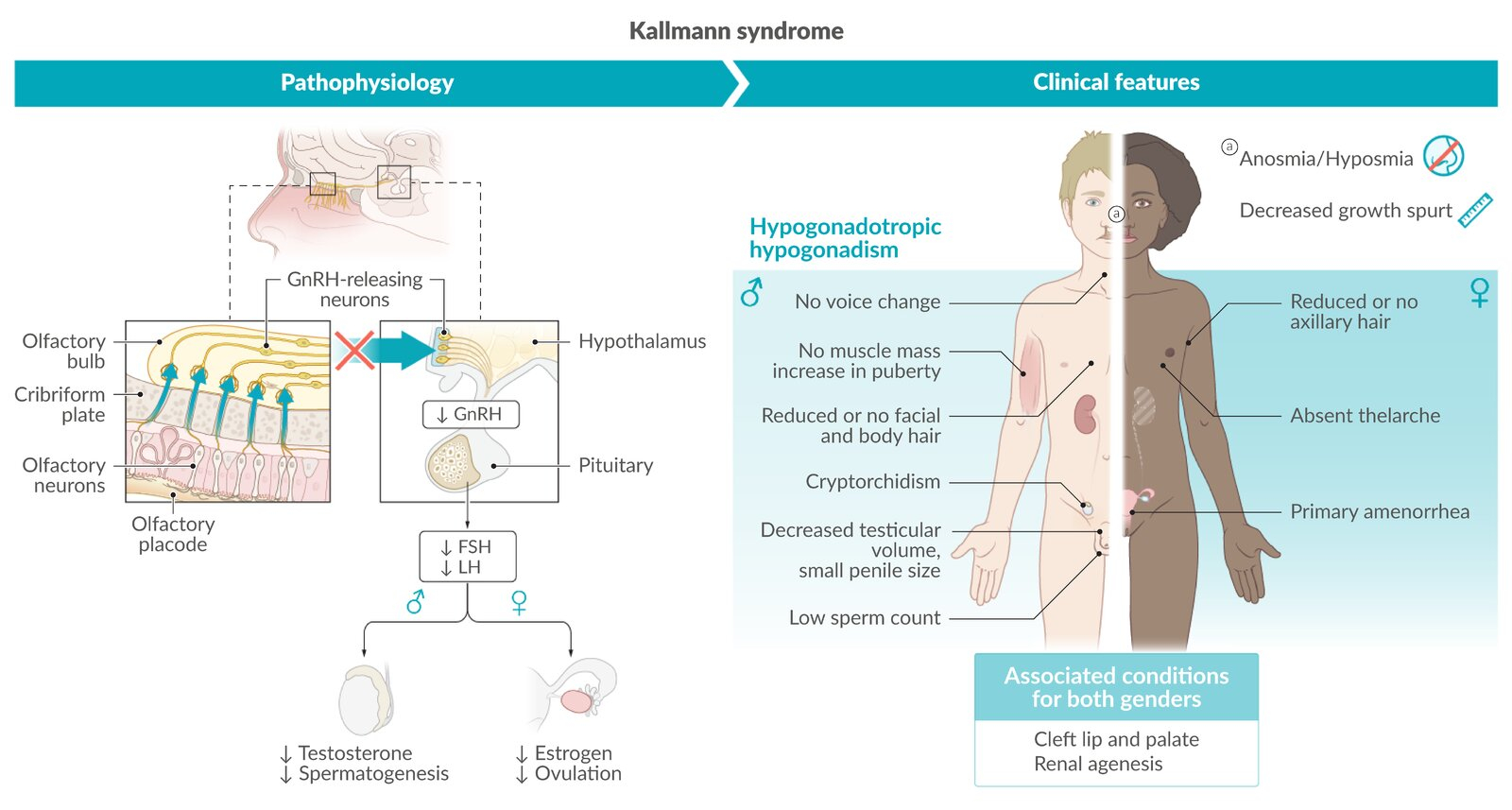
3. Kallmann Syndrome
Kallmann Syndrome
- Type: Primary amenorrhea (can present as delayed puberty)
- Etiology: Genetic disorder causing isolated GnRH deficiency
- Pathophysiology:
- Failure of GnRH neuron migration from olfactory placode to hypothalamus during embryonic development
- Olfactory bulb also fails to develop → anosmia
- Results in hypogonadotropic hypogonadism
Clinical Features
- Reproductive features:
- Delayed or absent puberty
- Primary amenorrhea in females
- Absence of secondary sexual characteristics
- Infertility
- In males: micropenis, cryptorchidism
- Olfactory features:
- Anosmia (complete loss of smell) or hyposmia (reduced sense of smell) → pathognomonic feature
- فقدان حاسة الشم - العلامة المميزة والأهم
- Associated features (variable):
- Renal agenesis
- Cleft lip/palate
- Hearing loss
- Mirror movements (synkinesis)
Diagnosis
- Clinical history: Delayed puberty + anosmia/hyposmia
- Hormonal profile:
- Low FSH and LH (hypogonadotropic hypogonadism)
- Low estradiol in females / low testosterone in males
- MRI brain: Absence or hypoplasia of olfactory bulbs and sulci
- Genetic testing: Multiple genes implicated (KAL1, FGFR1, others)
Management
- For pubertal induction and maintenance:
- Sex steroid replacement: estrogen + progesterone in females; testosterone in males
- For fertility:
- Pulsatile GnRH therapy (most physiological)
- Gonadotropin therapy (FSH + LH or hCG)
| Important – فكرة سؤال | |
|
A 17-year-old girl presents with primary amenorrhea and absent breast development. She mentions she has never been able to smell. Labs show low FSH, low LH, and low estradiol. Diagnosis: Kallmann Syndrome. The key clue is anosmia + hypogonadotropic hypogonadism. المفتاح لتشخيص Kallmann syndrome هو: فقدان حاسة الشم + تأخر البلوغ + انخفاض FSH و LH. إذا رأيت هذه المجموعة في السؤال، التشخيص هو Kallmann |
تذكر |
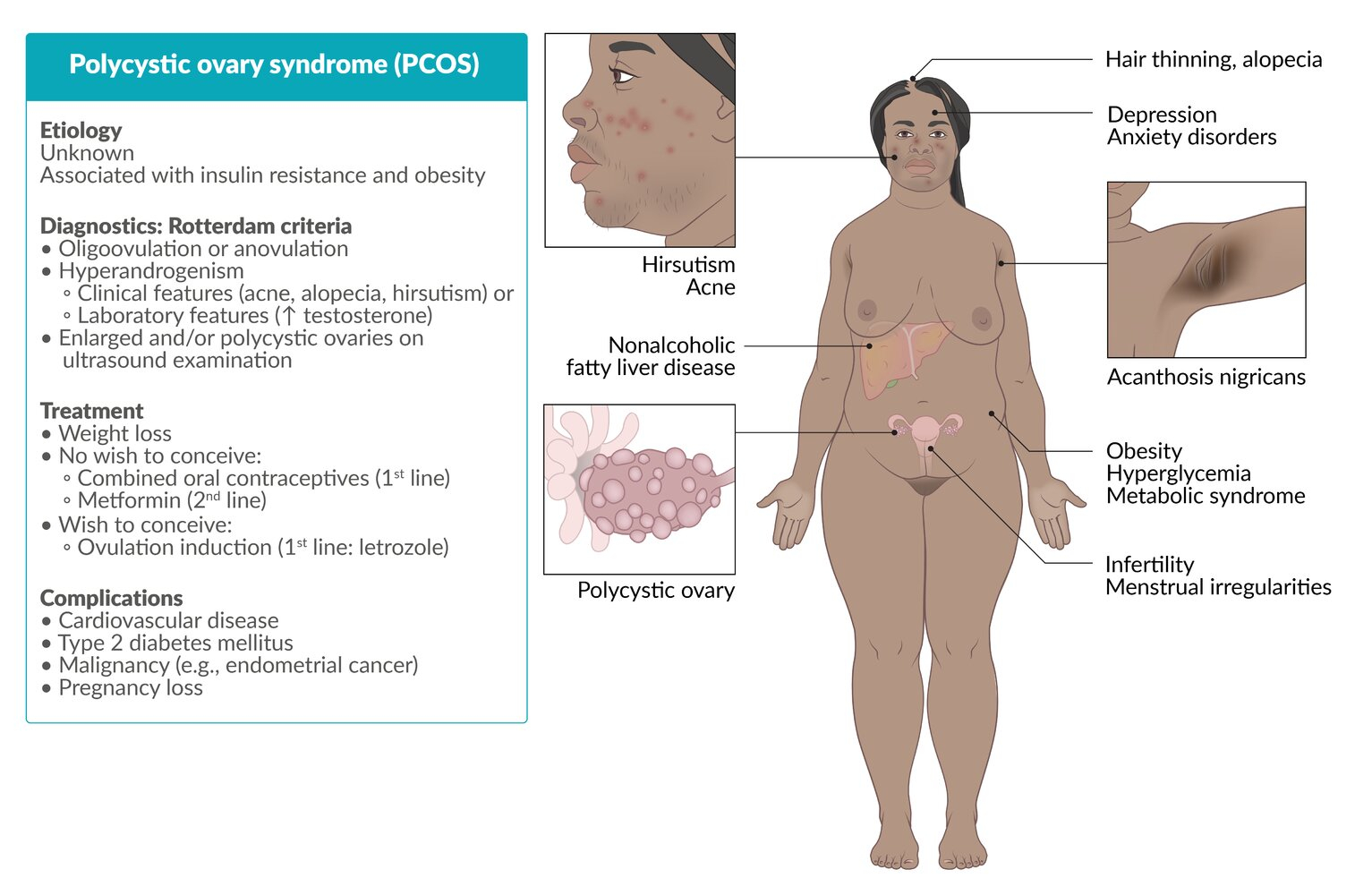
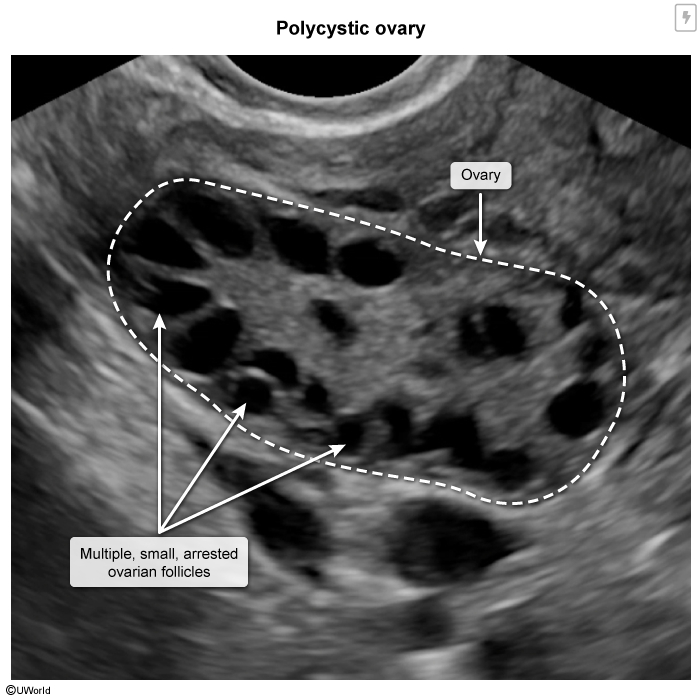
4. Polycystic Ovary Syndrome (PCOS)
Type: Secondary Amenorrhea or Oligomenorrhea
Etiology: Multifactorial (insulin resistance, androgen excess)
Pathophysiology:
- Insulin resistance → hyperinsulinemia → stimulates ovarian androgen production
- Excess androgens → disrupted follicular development → chronic anovulation
- Multiple follicles arrested at antral stage → "polycystic" appearance on ultrasound
Clinical Features:
- Irregular menses
- Hirsutism, acne
- Polycystic ovaries on ultrasound
- Obesity, insulin resistance
Diagnosis: Rotterdam Criteria (any 2 of 3):
- Oligo-/anovulation
- Clinical or biochemical hyperandrogenism
- Polycystic ovaries on ultrasound
Management:
- Lifestyle modification
- Oral contraceptives
- Metformin
- Ovulation induction for fertility
| Important – فكرة سؤال | |
|
A 22-year-old obese woman presents with irregular periods (every 2-3 months), acne, and excessive facial hair. Ultrasound shows enlarged ovaries with multiple small follicles. Diagnosis: PCOS. First-line treatment for menstrual irregularity: oral contraceptives. For infertility: clomiphene citrate or letrozole. PCOS هو أكثر سبب لانقطاع الطمث الثانوي في سن الإنجاب. العلامات المميزة: سمنة، دورة غير منتظمة، شعرانية، حب الشباب. التشخيص يحتاج 2 من 3 معايير Rotterdam |
تذكر |
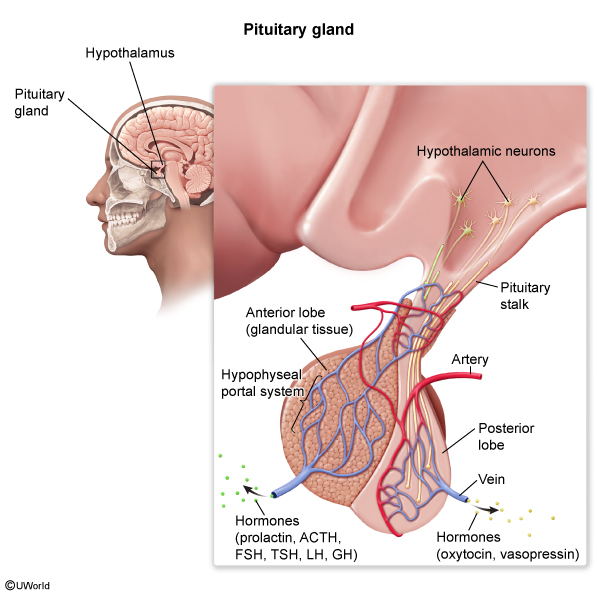
5. Sheehan Syndrome
Sheehan Syndrome
- Type: Secondary amenorrhea
- Etiology: Ischemic necrosis of the pituitary gland following severe postpartum hemorrhage
- Pathophysiology:
- During pregnancy, pituitary gland enlarges (especially lactotrophs) but blood supply does not increase proportionally
- Severe postpartum hemorrhage → hypovolemic shock → hypoperfusion of pituitary
- Results in pituitary infarction and necrosis
- Leads to panhypopituitarism (deficiency of all anterior pituitary hormones)
Clinical Features
- Immediate postpartum presentation:
- Failure to lactate postpartum (earliest and most specific sign) فشل الإرضاع بعد الولادة - أهم علامة
- History of severe postpartum hemorrhage
- Later presentations (due to hormone deficiencies):
- Gonadotropin deficiency:
- Amenorrhea (failure to resume menses postpartum)
- Loss of libido
- Breast atrophy
- ACTH deficiency (secondary adrenal insufficiency):
- Fatigue, weakness
- Hypotension
- Inability to handle stress
- TSH deficiency (secondary hypothyroidism):
- Fatigue, cold intolerance
- Weight gain
- Constipation
- Growth hormone deficiency:
- Decreased energy
- Changes in body composition
- Gonadotropin deficiency:
Diagnosis
- Clinical suspicion: History of postpartum hemorrhage + failure to lactate + amenorrhea
- Hormonal testing:
- Low or inappropriately normal pituitary hormones: FSH, LH, ACTH, TSH, prolactin
- Low target organ hormones: estradiol, cortisol, T4
- MRI pituitary:
- Empty sella or pituitary hypoplasia
- Small pituitary gland
- Stimulation tests may be needed:
- ACTH stimulation test
- Insulin tolerance test (gold standard but rarely done due to risks)
Management
- Lifelong hormone replacement therapy:
- Glucocorticoids: Hydrocortisone (must be started first) → most important
- Thyroid hormone: Levothyroxine (started after glucocorticoids to avoid adrenal crisis)
- Sex hormones: Estrogen + progesterone in premenopausal women
- Growth hormone: If symptomatic and patient desires treatment
- Stress dose steroids: During illness, surgery, or stress
- Patient education: Medical alert bracelet, emergency steroid administration
| Important – فكرة سؤال | |
|
A 28-year-old woman had severe bleeding during delivery 6 months ago. She has not resumed menstruation and was unable to breastfeed. She complains of fatigue, weakness, and cold intolerance. Diagnosis: Sheehan Syndrome. Key features: postpartum hemorrhage + inability to lactate + amenorrhea + symptoms of hormone deficiencies. العلامات المهمة: نزيف شديد بعد الولادة، فشل الإرضاع (أهم علامة)، عدم رجوع الدورة الشهرية، أعراض نقص الهرمونات. العلاج: تعويض هرموني مدى الحياة، نبدأ بالكورتيزون أولاً |
تذكر |
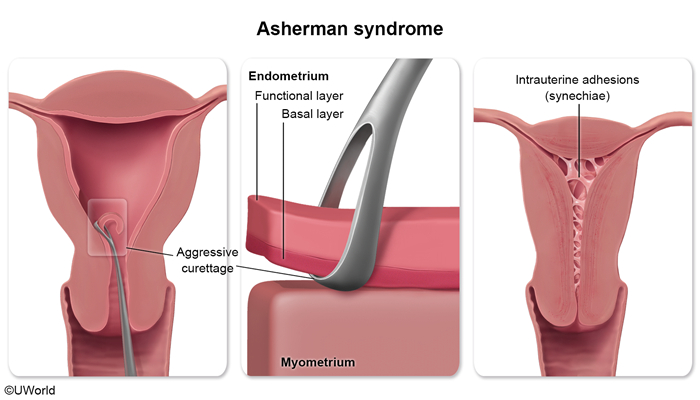
6. Asherman Syndrome (Intrauterine Adhesions)
Asherman Syndrome (Intrauterine Adhesions)
- Type: Secondary amenorrhea
- Etiology: Endometrial scarring and intrauterine adhesions
- Common causes:
- Dilation and curettage (D&C), especially following postpartum hemorrhage or abortion (most common)
- Endometrial infection (endometritis, tuberculosis)
- Uterine surgery (myomectomy, cesarean section)
- Uterine artery embolization
- Pathophysiology:
- Trauma to basal layer of endometrium → scarring and adhesion formation
- Adhesions obliterate uterine cavity partially or completely
- Loss of functional endometrium → amenorrhea despite normal ovarian function
Clinical Features
- Menstrual abnormalities:
- Secondary amenorrhea (most common presentation)
- Hypomenorrhea (scanty menstruation)
- Reproductive issues:
- Infertility
- Recurrent pregnancy loss
- Abnormal placentation in pregnancy
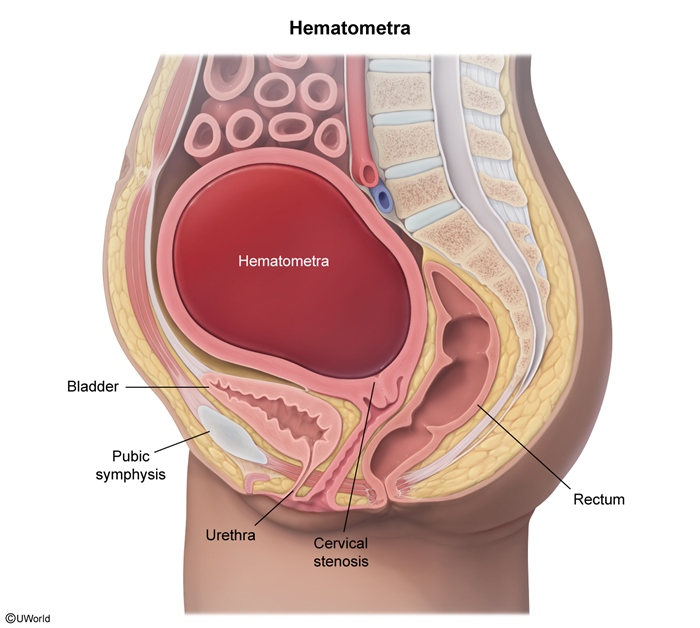
- Cyclic pelvic pain:
- Occurs if adhesions trap menstrual blood (hematometra) (figure)
- Pain occurs cyclically with hormonal changes despite no visible bleeding
- History: Recent uterine instrumentation (D&C) or infection
Diagnosis
- History: Prior uterine instrumentation + new-onset amenorrhea
- Progesterone withdrawal test:
- Negative (no bleeding after progesterone) despite normal estrogen levels
- Indicates anatomical problem, not hormonal
- Hysteroscopy: Gold standard for diagnosis
- Direct visualization of intrauterine adhesions
- Can be therapeutic (adhesiolysis during same procedure)
- Hysterosalpingography (HSG):
- Shows filling defects in uterine cavity
- Irregular uterine contour
- Saline infusion sonography: May show adhesions
- Hormonal profile: Normal FSH, LH, estradiol (ovarian function intact)
Management
- Hysteroscopic adhesiolysis:
- Surgical removal of adhesions under direct visualization
- Treatment of choice
- Post-operative management:
- High-dose estrogen therapy to stimulate endometrial regeneration
- Intrauterine device (IUD) or Foley catheter to prevent re-adhesion
- Follow-up hysteroscopy to assess cavity
- Prevention:
- Gentle D&C technique
- Ultrasound guidance during uterine procedures
| Important – فكرة سؤال | |
|
A 26-year-old woman underwent D&C for postpartum hemorrhage 3 months ago. She now presents with absence of menstruation. Hormonal workup shows normal FSH, LH, and estradiol. Progesterone challenge test is negative. Diagnosis: Asherman Syndrome. Confirmatory test: hysteroscopy. Treatment: hysteroscopic adhesiolysis. المفتاح: تاريخ D&C + انقطاع الطمث الثانوي + هرمونات طبيعية + progesterone challenge test سلبي. هذا يدل على مشكلة تشريحية في الرحم وليست هرمونية |
تذكر |
7. Mayer-Rokitansky-Küster-Hauser (MRKH) Syndrome
Mayer-Rokitansky-Küster-Hauser (MRKH) Syndrome
- Type: Primary amenorrhea
- Etiology: Congenital absence or underdevelopment of Müllerian structures
- Karyotype: 46,XX (genetically and phenotypically female)
- Pathophysiology:
- Failure of Müllerian duct development during embryogenesis
- Results in absence of uterus, cervix, and upper 2/3 of vagina
- Ovaries are normal (develop from different embryologic origin)
Clinical Features
- At presentation:
- Primary amenorrhea in adolescent with normal secondary sexual characteristics
- Usually diagnosed at age 15-18 when patient seeks care for absent menses
- Normal features:
- Normal breast development
- Normal pubic and axillary hair
- Normal external genitalia
- Normal ovarian function (normal hormones)
- Anatomical findings:
- Absent or shortened vagina (blind vaginal pouch)
- Absent uterus and cervix
- Normal ovaries (may be palpable on exam)
- Associated anomalies (in some cases):
- Renal anomalies (30-40%): unilateral renal agenesis, ectopic kidney
- Skeletal abnormalities (10-15%): vertebral, rib anomalies
Diagnosis
- Physical examination:
- Normal secondary sexual characteristics
- Short or absent vaginal canal on speculum or digital exam
- Hormonal profile:
- Normal FSH, LH, estradiol (normal ovarian function)
- Karyotype: 46,XX
- Pelvic imaging (MRI preferred):
- Absence of uterus and upper vagina
- Presence of normal ovaries
- Renal ultrasound: To evaluate for associated renal anomalies
Management
- Vaginal dilation therapy (Frank method):
- Non-surgical first-line approach
- Progressive vaginal dilators used regularly
- Success rate: 80-90% with consistent use
- Surgical vaginal reconstruction:
- If dilation fails or patient prefers surgery
- Fertility options:
- Patient's own oocytes can be retrieved
- IVF with gestational surrogacy
- Adoption
- Psychological support: Essential for coping with diagnosis
- No hormonal therapy needed: Ovarian function is normal
| Important – فكرة سؤال | |
|
A 16-year-old girl presents with primary amenorrhea. She has well-developed breasts and normal pubic hair. Pelvic MRI shows absence of uterus but normal ovaries. Karyotype is 46,XX. Diagnosis: MRKH Syndrome. Key difference from AIS: normal karyotype (46,XX) and normal body hair. الفرق الأساسي عن AIS: الكروموسومات 46,XX طبيعية، شعر الجسم طبيعي، المبايض موجودة وطبيعية. العلامة المشتركة: غياب الرحم. العلاج الأول: توسيع المهبل بالطرق التدريجية |
تذكر |
8. 5-Alpha-Reductase Deficiency
5-Alpha-Reductase Deficiency
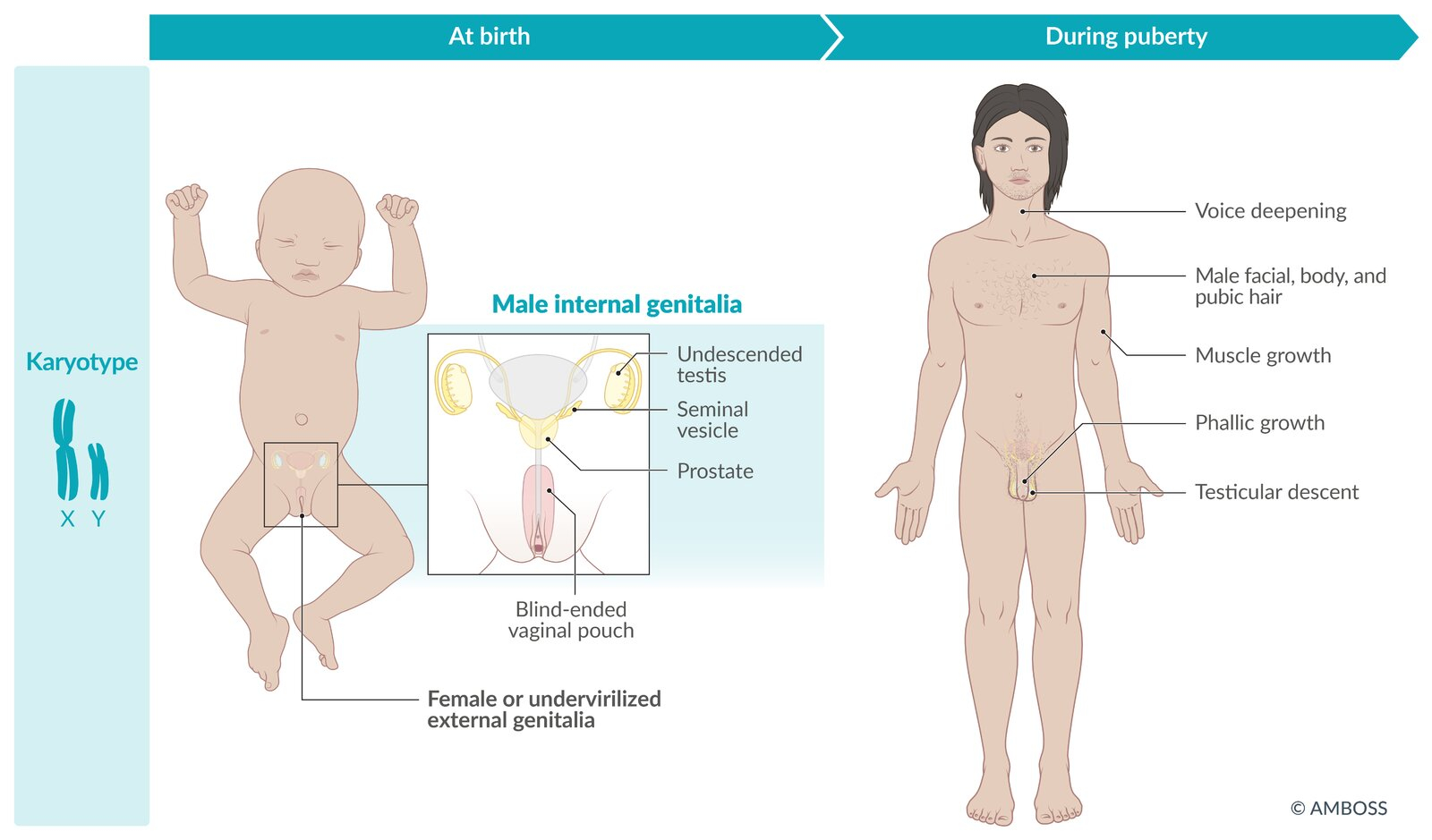
- Type: Primary amenorrhea in 46,XY individuals
- Genetics: Autosomal recessive mutation in SRD5A2 gene
- Karyotype: 46,XY (genetically male)
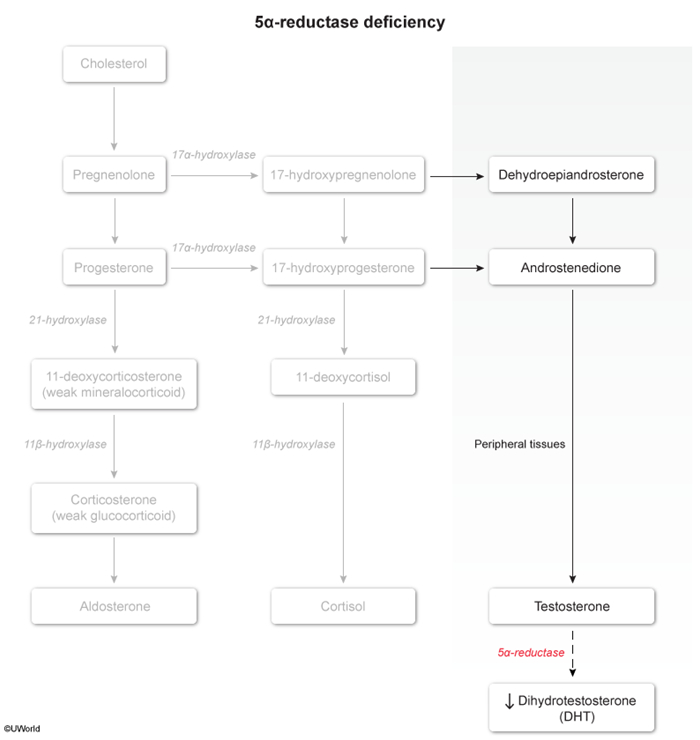
- Pathophysiology:
- Deficiency of 5-alpha-reductase enzyme
- This enzyme converts testosterone to dihydrotestosterone (DHT)
- DHT is essential for masculinization of external genitalia in utero
- Testosterone levels are normal or elevated
- Internal male structures develop normally (testosterone-dependent)
- External genitalia remain undervirilized (DHT-dependent)
Clinical Features
- At birth:
- Ambiguous genitalia or female-appearing external genitalia
- Micropenis
- Bifid scrotum
- Blind vaginal pouch
- Often raised as female
- Internal structures:
- Normal male internal reproductive organs (epididymis, vas deferens, seminal vesicles)
- Testes present (may be undescended)
- No uterus or fallopian tubes (due to AMH from testes)
- At puberty (dramatic changes):
- Significant virilization occurs
- Testicular descent
- Phallic growth
- Increased muscle mass
- Deepening of voice
- Male body habitus
- Facial and body hair (but less than typical males)
- No breast development
- Unique feature: Some individuals change gender identity from female to male at puberty
Diagnosis
- Karyotype: 46,XY
- Hormonal profile:
- Normal or elevated testosterone
- Low DHT
- Elevated testosterone:DHT ratio (diagnostic)
- Elevated LH
- Genetic testing: Mutation in SRD5A2 gene
- Physical examination: Ambiguous genitalia with palpable gonads
Management
- Gender assignment: Complex decision, ideally made with multidisciplinary team
- Consider degree of virilization at birth
- Cultural context
- Patient/family preferences
- If female gender identity chosen:
- Gonadectomy (remove testes) to prevent virilization at puberty
- Estrogen replacement therapy
- Vaginal reconstruction if needed
- If male gender identity chosen:
- Testosterone supplementation
- Surgical correction of hypospadias and cryptorchidism
- Psychological support
- Fertility: Usually infertile due to impaired spermatogenesis
| Important – فكرة سؤال | |
|
A child raised as female presents at age 12 with unexpected virilization: voice deepening, muscle growth, and phallic enlargement. Karyotype shows 46,XY. Labs show normal testosterone but low DHT with elevated testosterone:DHT ratio. Diagnosis: 5-Alpha-Reductase Deficiency. العلامة المميزة: طفل يُربى كأنثى ثم يحدث تذكير واضح عند البلوغ. الفحص المهم: نسبة testosterone:DHT مرتفعة. هذا المرض نادر لكن مهم للامتحانات |
تذكر |
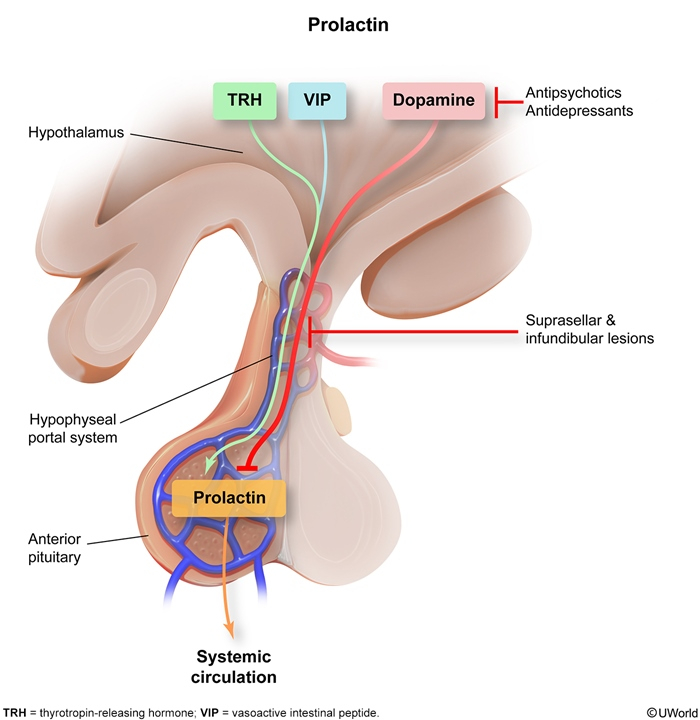
9. Hyperprolactinemia
Hyperprolactinemia
- Type: Secondary amenorrhea (one of the most common endocrine causes)
- Etiology: Elevated prolactin levels from various causes
- Common causes:
- Prolactinoma (prolactin-secreting pituitary adenoma) - most common pathological cause
- Medications:
- Antipsychotics (risperidone, haloperidol)
- Antiemetics (metoclopramide, domperidone)
- Antidepressants (SSRIs, tricyclics)
- Primary hypothyroidism: ↑ TRH → ↑ prolactin
- Chronic renal failure: Decreased clearance
- Physiological: Pregnancy, lactation, stress, nipple stimulation
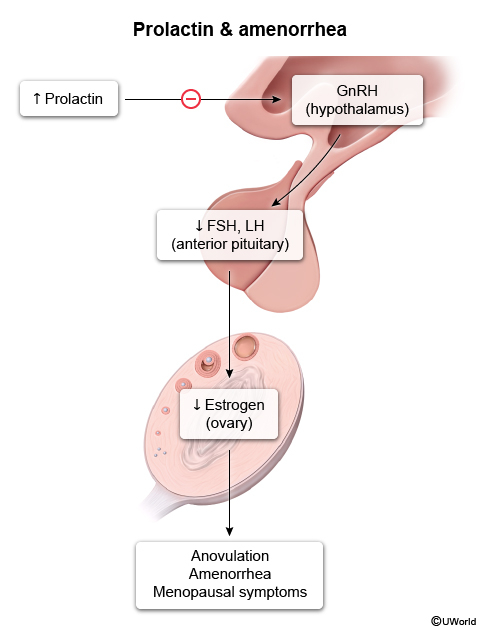
- Pathophysiology:
- Elevated prolactin inhibits GnRH pulsatility
- Leads to decreased FSH and LH secretion
- Results in anovulation and amenorrhea
Clinical Features
- Reproductive symptoms:
- Secondary amenorrhea or oligomenorrhea
- Infertility due to anovulation
- Decreased libido
- Galactorrhea: إدرار الحليب
- Spontaneous or expressible milk discharge from nipples
- Occurs in ~80% of women with hyperprolactinemia
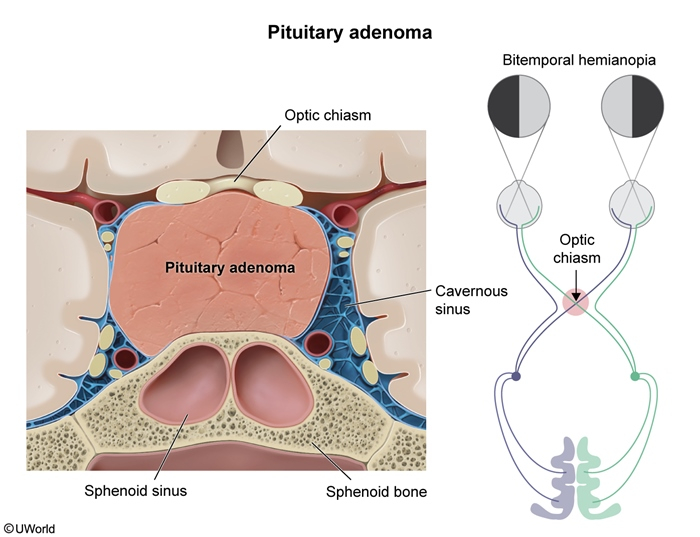
- Symptoms of mass effect (if large prolactinoma):
- Headaches
- Visual field defects (bitemporal hemianopsia)
- Cranial nerve palsies
- In males:
- Erectile dysfunction
- Decreased libido
- Gynecomastia (rare)
Diagnosis
- Serum prolactin level:
- Obtain fasting, morning sample (prolactin has diurnal variation)
- Repeat if elevated to confirm
- Normal: < 25 ng/mL
- Level > 200 ng/mL strongly suggests prolactinoma
- Rule out secondary causes:
- Pregnancy test (β-hCG)
- TSH and free T4 (rule out hypothyroidism) → must be checked
- Medication review
- Renal function tests
- MRI pituitary:
- Indicated if prolactin persistently elevated and secondary causes excluded
- Identifies prolactinoma (microadenoma < 10 mm, macroadenoma ≥ 10 mm)
Management
- Treat underlying cause:
- Discontinue offending medications if possible
- Treat hypothyroidism with levothyroxine
- Dopamine agonists (first-line for prolactinoma):
- Cabergoline
- Bromocriptine
- Effects: normalize prolactin, restore ovulation, shrink tumor
- Surgery (transsphenoidal):
- For large tumors resistant to medication
- Tumors with mass effect not responding to dopamine agonists
- Monitoring:
- Prolactin levels
- Visual fields if macroadenoma
- Repeat MRI to assess tumor size
| Important – فكرة سؤال | |
|
A 28-year-old woman presents with 6 months of amenorrhea and milky discharge from both breasts. She is not pregnant. Prolactin level is 180 ng/mL. MRI shows a 7mm pituitary adenoma. Diagnosis: Prolactinoma (microadenoma). First-line treatment: cabergoline (dopamine agonist). دائماً افحص TSH و T4 لاستثناء hypothyroidism قبل تشخيص prolactinoma. العلاج الأول: dopamine agonists (cabergoline أفضل من bromocriptine). الجراحة فقط إذا لم تستجب للأدوية |
تذكر |
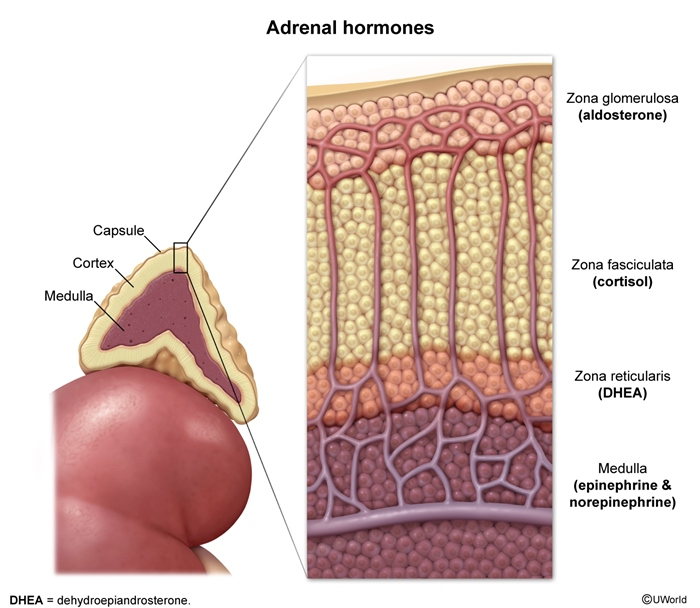
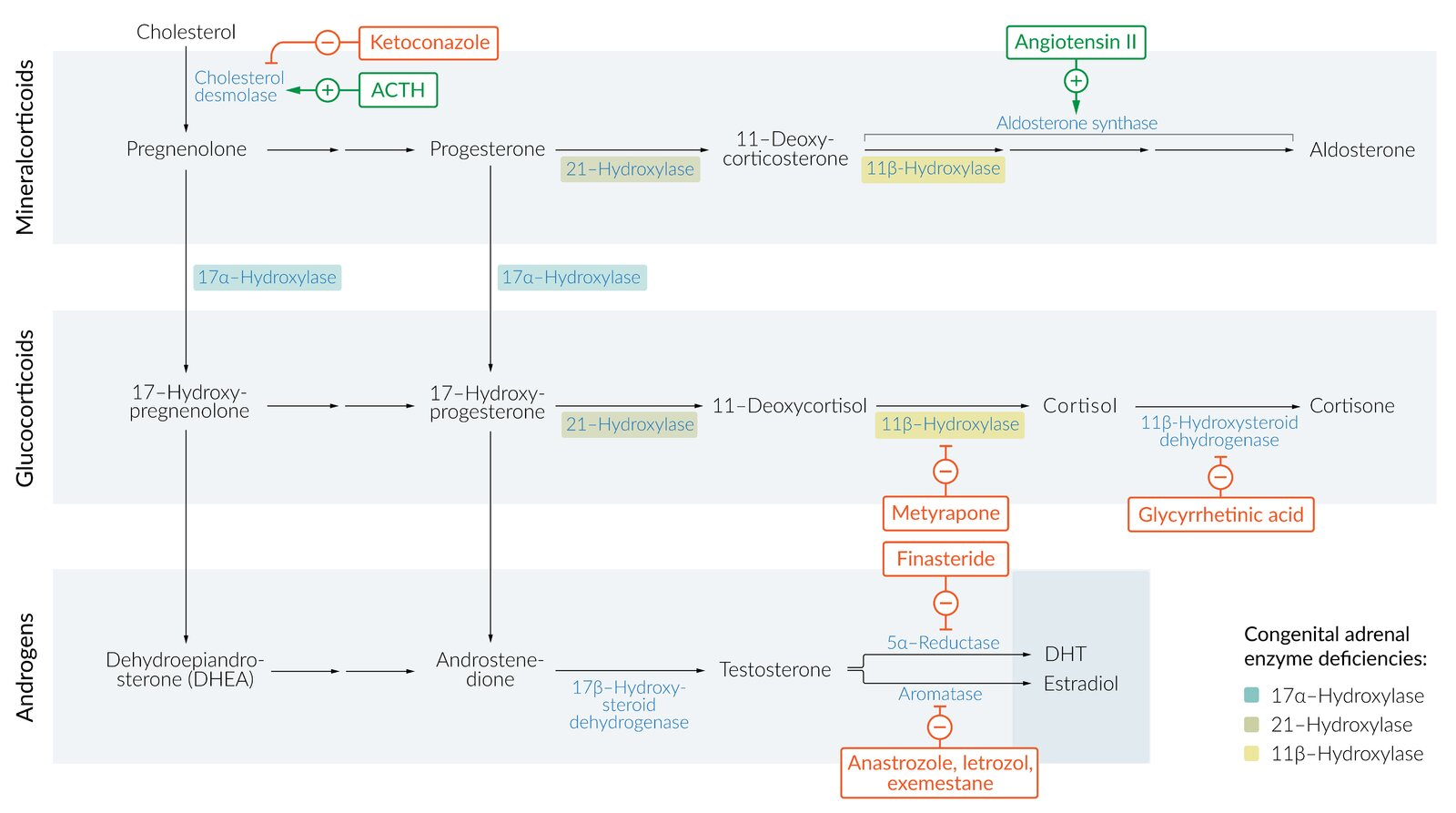
10. Congenital Adrenal Hyperplasia (CAH)
Congenital Adrenal Hyperplasia (CAH)
- Type: Variable; can cause ambiguous genitalia (disorder of sex development) or secondary amenorrhea
- Genetics: Autosomal recessive enzyme defects in adrenal steroidogenesis
- Most common form: 21-hydroxylase deficiency (>90% of cases)
- Pathophysiology:
- Enzyme deficiency → impaired cortisol and aldosterone synthesis
- Precursors shunted to androgen pathway → excess androgens
- Decreased cortisol → increased ACTH → adrenal hyperplasia
Forms of CAH
- Classic CAH (severe):
- Salt-wasting form: Deficiency of both cortisol and aldosterone
- Life-threatening in neonatal period
- Hyponatremia, hyperkalemia, metabolic acidosis
- Hypotension, dehydration
- Simple virilizing form: Cortisol deficiency only, aldosterone preserved
- Virilization without salt wasting
- Salt-wasting form: Deficiency of both cortisol and aldosterone
- Non-classic CAH (mild):
- Presents later in life (adolescence or adulthood)
- Milder androgen excess
- May present with amenorrhea, hirsutism, infertility
Clinical Features
- At birth (classic form):
- Ambiguous genitalia (virilization of external genitalia)
- Clitoromegaly
- Labial fusion
- Internal female organs normal (uterus, ovaries)
- In childhood:
- Premature pubarche (early pubic hair)
- Accelerated growth initially, then short final height due to early epiphyseal closure
- In adolescence/adulthood (non-classic):
- Hirsutism
- Acne
- Oligomenorrhea or amenorrhea
- Infertility
- Similar to PCOS presentation
- Salt-wasting crisis (if present):
- Occurs at 1-4 weeks of age
- Vomiting, diarrhea, dehydration
- Failure to thrive
- Hypotension, shock
Diagnosis
- Neonatal screening: Now performed in many countries (measures 17-hydroxyprogesterone)
- Laboratory findings:
- Elevated 17-hydroxyprogesterone (diagnostic for 21-hydroxylase deficiency)
- Elevated androgens (DHEA-S, androstenedione, testosterone)
- In salt-wasting: hyponatremia, hyperkalemia, elevated renin
- ACTH stimulation test: Gold standard; exaggerated rise in 17-OHP
- Genetic testing: Can identify specific CYP21A2 mutations
- Imaging:
- Pelvic ultrasound: normal uterus and ovaries in females
- Adrenal ultrasound or CT: may show adrenal enlargement
Management
- Lifelong glucocorticoid replacement:
- Hydrocortisone (preferred in children)
- Suppresses ACTH and reduces androgen overproduction
- Stress-dose steroids during illness or surgery
- Mineralocorticoid replacement (if salt-wasting):
- Fludrocortisone
- Sodium supplementation in infancy
- Surgical correction:
- Feminizing genitoplasty for virilized females
- Usually performed in infancy or early childhood
- For fertility:
- Optimize glucocorticoid dose to suppress androgens
- May need ovulation induction
- Monitoring:
- Growth and bone age
- Electrolytes
- 17-OHP and androgens
| Important – فكرة سؤال | |
|
A newborn with ambiguous genitalia presents at 2 weeks of age with vomiting, dehydration, and lethargy. Labs show hyponatremia and hyperkalemia. 17-hydroxyprogesterone is markedly elevated. Diagnosis: Classic CAH with salt-wasting. This is a medical emergency requiring immediate glucocorticoid and mineralocorticoid replacement. CAH يمكن أن يظهر بأشكال مختلفة: عند الولادة (أعضاء تناسلية غير واضحة)، في الطفولة (بلوغ مبكر)، أو في المراهقة (شعرانية وانقطاع طمث). الفحص التشخيصي: 17-hydroxyprogesterone مرتفع جداً |
تذكر |
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.