سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Background
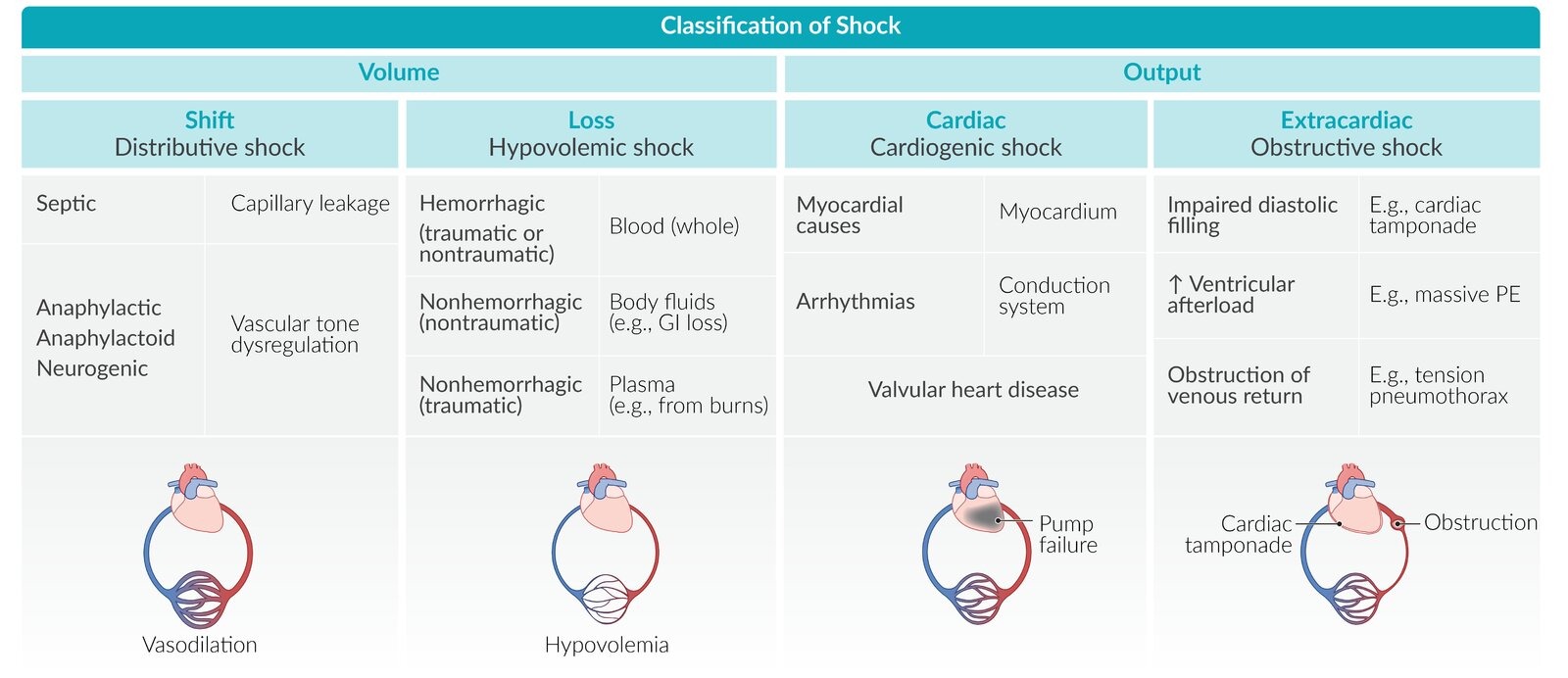
- Shock is a life threatening circulatory disorder that leads to tissue hypoxia and ischemia
- The several causes of shock are classified into hypovolemic, cardiogenic, obstructive, and distributive shock
- Distributive shock is further classified into septic, anaphylactic and neurogenic shock
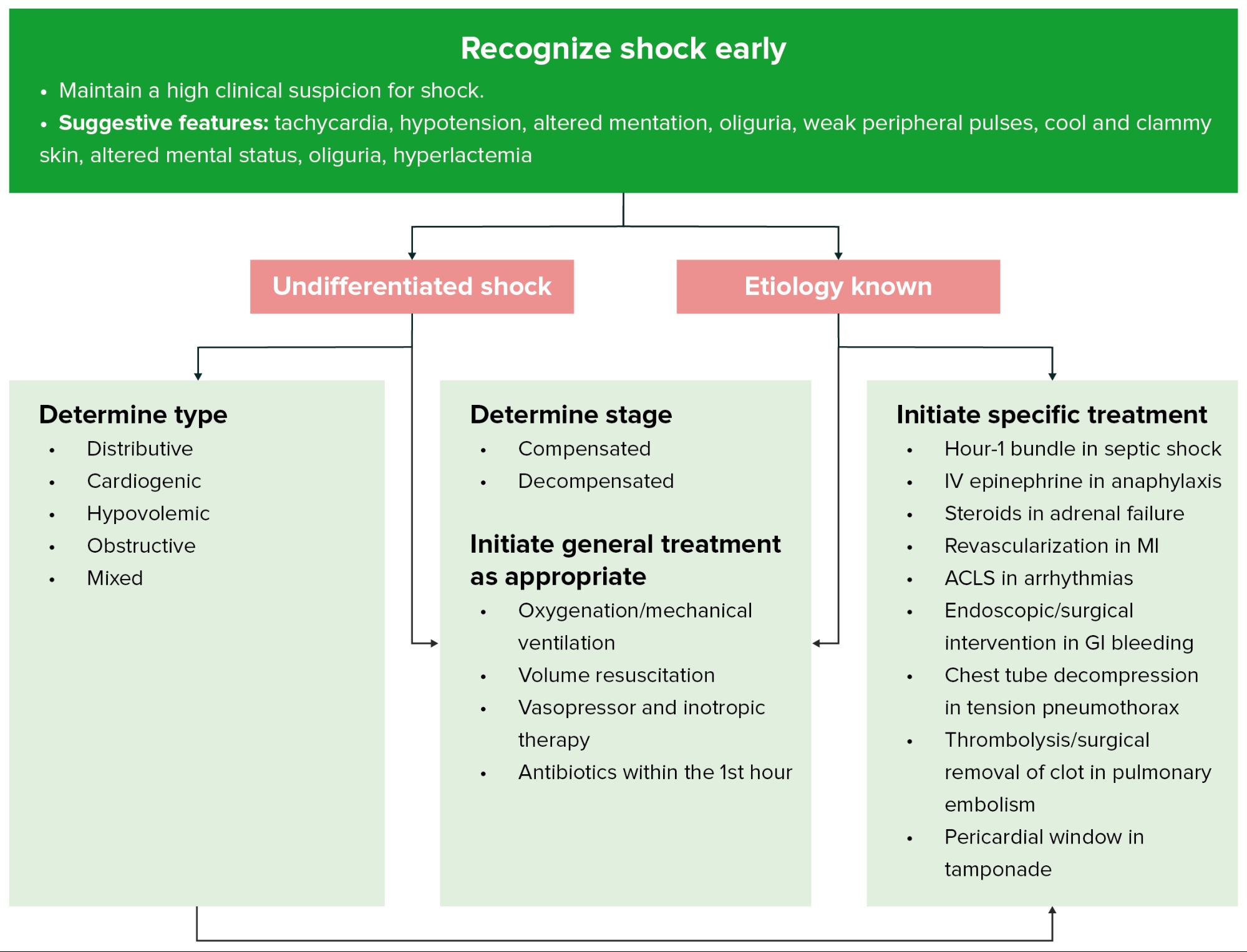
- Diagnosis is mostly clinical but measurements of functional parameters (eg, cardiac output, systemic vascular resistance) can help distinguish between the different types of shock
- Management of shock involves circulatory support and treatment of the underlying cause
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Hemodynamic measurements of undifferentiated shock
| Hemodynamic Measurements in Shock | |||
|---|---|---|---|
| Parameter | Hypovolemic Shock | Cardiogenic Shock | Septic Shock |
| Right atrial pressure (preload) | ↓ | ↑ | Normal to slight ↓ |
| Pulmonary capillary wedge pressure (preload) | ↓ | ↑ | Normal to slight ↓ |
| Cardiac index (pump function) | ↓ | ↓ | ↑ |
| Systemic vascular resistance (afterload) | ↑ | ↑ | ↓ |
| Mixed venous oxygen saturation | ↓ | ↓ | ↑ |
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Hypovolemic shock
Background
- Loss of intravascular fluid volume would lead to decreased preload and stroke volume (this would lead to decreased cardiac output and compensatory increase in systemic vascular resistance)
Hemorrhage
- Postpartum hemorrhage
- Upper GI bleeding (eg, variceal bleeding, PUD)
- Blunt/penetrating trauma
- Ruptured aneurysm or hematoma
- Arteriovenous fistula
Nonhemorrhagic shock
- GI loss (Eg, diarrhea, vomiting)
- Increased sensitive fluid loss (eg, burns)
- Third space fluid loss (eg, bowel obstruction, pancreatitis)
- Renal fluid loss (eg, adrenal insufficiency, drug induced diuretics)
| Classification of Hemorrhagic Shock | ||||
|---|---|---|---|---|
| Class | 1 | 2 | 3 | 4 |
| Blood loss (%) | < 15% | 15-30% | 30-40% | >40% |
| Volume loss | 750 mL | 750-1500 mL | 1500-2000 mL | >2000 mL |
| Heart rate (bpm) | 70-99 | 100-120 | 120-140 | >140 |
| Systolic blood pressure | Normal | Normal | ↓ | ↓ |
| Pulse pressure | Normal or ↑ | ↓ | ↓ | ↓ |
| Respiratory rate (rpm) | Normal | 20-30 | 30-40 | >40 |
| Urine output | > 30 mL/hour | 20-30 mL/hour | 1-15 mL/hour | Absent |
| Mental status | Normal | Mildly anxious | Anxious, confused | Confused, lethargic |
Clinical presentation
- Physical examination include hypotension, tachycardia, reduced skin turgor, nondistended jugular veins, dry mucous membranes and cold clammy skin
Diagnosis
- Most cases are clinically diagnosed
Treatment
- The priority is aggressive fluid resuscitation (further treatment depends on the etiologic category of hypovolemia (hemorrhagic vs. nonhemorrhagic)
- If hemorrhagic shock is suspected, perform blood grouping and cross matching and have packed RBCs at hand for transfusion (uncrossmatched RBC type O negative units can be transfused if the hemorrhage is severe)
- Treat the underlying etiology
- Supportive care (electrolyte abnormalities should be corrected)
- Once hemodynamically stable, replacement of fluid loss should be continued and oral rehydration therapy should be attempted
Complications
- Acute renal failure
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Cardiogenic shock
Background
- Cardiogenic shock is a shock secondary to dysfunction of the heart (pump failure)
- The heart is unable to generate adequate cardiac output to maintain tissue perfusion
- Coronary artery disease is a major risk factor
| Cardiogenic Syncope | |
|---|---|
| Etiology | Clues to Diagnosis |
| Aortic stenosis or HCM |
|
| Ventricular tachycardia |
|
| Sick sinus syndrome |
|
| Advanced AV block |
|
| Torsades de pointes |
|
Clinical presentation
- Symptoms include myocardial infarction (chest pain and dyspnea) or arrhythmias (palpitations and syncope)
- Physical examination findings include hypotension, tachycardia, pulmonary edema (diffuse lung crackles, distended jugular veins), cool extremities, and decreased urine output
Diagnosis
- Most cases are clinically diagnosed
Treatment
- Supportive (fluid resuscitation and oxygen)
- Medical intervention (intravenous inotropic drugs like dopamine, dobutamine, norepinephrine)
Complications
- Pulmonary edema
- Acute renal failure
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Obstructive shock
Background
- A type of shock secondary to extra-cardiac causes of pump failure
- There are several etiologies to obstructive shock; subclassified into pulmonary vascular and mechanical etiologies
- Pulmonary vascular etiologies are associated with right ventricular failure. These include pulmonary embolism and severe pulmonary hypertension
- Mechanical etiologies include tension pneumothorax, pericardial tamponade, constrictive pericarditis, and restrictive cardiomyopathy
Clinical presentation
- Physical examination findings include hypotension, tachycardia, jugular venous distention, and cold clammy skin
Diagnosis
- Echocardiography (to detect underlying causes, such as pericardial tamponade)
- Most cases are clinically diagnosed
Treatment
- Manage underlying cause
Complications
- Death
- Acute renal failure
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Distributive shock
Distributive shock
- A shock secondary to severe peripheral vasodilation
- Risk factors include infection, exposure to allergens, or trauma
Septic shock (most common type)
- Background
- Septic shock is a type of distributive shock
- This condition is a potentially fatal medical condition that occurs when sepsis leads to hypotension (this condition is the most severe complication of sepsis)
- There is a decreased systemic vascular resistance due to peripheral vasodilation and increased cardiac output
- Clinical presentation
- Bounding pulse seen in early septic shock due to hyperdynamic circulation
- Late septic shock presents with decreased cardiac output
- Diagnosis
- Most cases are clinically diagnosed
- Treatment
- Fluid resuscitation
- Identifying the underlying infection and treating it properly
- Vasopressors
- Complications
- Death
- Acute renal failure
Non-septic shock (Anaphylactic and Neurogenic shock)
- Anaphylactic shock
- Background
- Anaphylactic shock is a potentially life threatening systemic allergic reason (can results in airway obstruction and cardiovascular collapse)
- Anaphylactic shock is very rapid (minutes to hours)
- Assess and secure the airway as needed
- Remove allergen when possible (e.g., stop medication or IV contrast)
- Administer epinephrine IM 1:1,000 as soon as possible and repeat as needed
- Provide immediate hemodynamic support with fluid resuscitation
- Differential diagnosis includes vasovagal syncope and other diseases associated with flushing (alcohol-induced, rosacea, or carcinoid tumor)
-
Causes of anaphylaxis Immunologic mechanism IgE-mediated - Medications
- Food
- Insect stings/bites
- Latex
Nonimmunologic mechanisms Direct activation of mast cells and basophils - Exercise
- Cold air
- Iodinated contrast medium
- Medications (eg, opioids, NSAIDs)
Idiopathic - Mast cell activation syndrome
- Clinical presentation
-
Anaphylaxis Category Details Triggers - Food (e.g., nuts, shellfish)
- Medications (e.g., beta-lactam antibiotics)
- Insect stings
Clinical Manifestation - Cardiovascular (vasodilation, hypotension, edema, and tachycardia)
- Respiratory (stridor, hoarseness, and wheezing)
- Cutaneous (urticaria, pruritus, flushing)
- Gastrointestinal (nausea, vomiting, and abdominal pain)
Treatment - Intramuscular epinephrine
- Airway management and volume resuscitation
- Adjunctive therapy (e.g., antihistamines, glucocorticoids)
-
Clinical Features of Anaphylaxis Category Details Cutaneous/Mucosal - Ocular: periorbital swelling, injected conjunctiva, tearing
- Oral mucosa: swelling, tingling, or itching of tongue and lips
- Skin: urticaria, flushing, pruritus
Respiratory - Nose: congestion, rhinorrhea
- Upper airway: edema (hoarseness and stridor)
- Lower airway: bronchospasm (wheezing)
Cardiovascular - Vasodilation (hypotension and syncope)
- Cardiac dysfunction, cardiac arrest
Gastrointestinal - Nausea, vomiting, abdominal pain, diarrhea
Neurological - Headache, confusion, anxiety, feeling of impending doom
-
- Treatment
-
Management of Anaphylaxis Category Details Immediate Management - Epinephrine (most common)
- IM is preferred, may be repeated (e.g., 3 doses)
- IV crystalloids and Trendelenburg positioning for hypotension
- Albuterol for bronchospasm
- Early intubation for upper airway obstruction
Adjunct Management - Antihistamines
- Glucocorticoids
- Glucagon for patients on beta blockers (reversal)
- Hospital admission for severe initial presentation (e.g., shock) or ongoing symptoms despite treatment
-
- Background
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Neurogenic shock
- Background
- A type of distributive shock that is secondary to a traumatic brain injury
- Clinical presentation
- Physical examination include hypotension, warm/dry skin, may have fever
- Diagnosis
- Most cases are clinically diagnosed
- Treatment
- Fluid resuscitation
- Vasopressors
- Complications
- Death
- Acute renal failure
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Shock Management
| Treatments for Shock | ||
|---|---|---|
| Type | Subtype | Treatment |
| Hypovolemic | Nonhemorrhagic |
|
| Hemorrhagic |
|
|
| Cardiogenic | — |
|
| Obstructive | — |
|
| Distributive | Septic |
|
| Anaphylactic |
|
|
| Neurogenic |
|
|
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.
فيديوهات الشرح
بطاقات تفاعلية
أسئلة ممارسة
اشترك الآن