Summary
Acute cholecystitis is an inflammatory condition of the gallbladder, most commonly caused by gallstone obstruction of the cystic duct (90-95% of cases). It presents with persistent right upper quadrant (RUQ) pain lasting >4-6 hours, fever, and positive Murphy's sign. Diagnosis is primarily clinical, supported by ultrasound findings of gallbladder wall thickening >4mm, pericholecystic fluid, and gallstones. Early laparoscopic cholecystectomy within 72 hours is the standard treatment. Complications include gangrene, perforation, and empyema. Acalculous cholecystitis, occurring in critically ill patients, represents 5-10% of cases and carries higher mortality.
Definition
- Acute cholecystitis: Acute inflammation of the gallbladder wall
- Results from cystic duct obstruction in ~90-95% of cases (calculous cholecystitis)
- 5-10% occur without gallstones (acalculous cholecystitis) - typically in critically ill patients
- Most frequent complication of gallstone disease
- Distinguished from biliary colic by:
- Duration of pain (>4-6 hours vs <4 hours)
- Presence of inflammatory signs (fever, leukocytosis)
- Gallbladder wall changes on imaging
Types of Acute Cholecystitis
- Calculous – most common
- Acalculous – 5–10%, in critically ill patients
- Emphysematous
- Gangrenous
- Empyema
- Chronic cholecystitis – chronic inflammatory infiltration on histopathology
| Types of Acute Cholecystitis | ||
|---|---|---|
| Type | Characteristics | Clinical Features |
| Calculous (90–95%) |
|
|
| Acalculous (5–10%) |
|
|
| Emphysematous |
|
|
| Gangrenous |
|
|
Risk Factors
- For Calculous Cholecystitis - follows the "4 F's" rule:
- Female
- Forty (age >40)
- Fertile (pregnancy, OCP use)
- Fat (obesity, rapid weight loss)
- Additional risk factors:
- Hemolytic disorders (sickle cell disease) → pigment stones
- Total parenteral nutrition (TPN) → bile stasis
- Diabetes mellitus
- Hyperlipidemia
- Fibrate medications (↓ bile acid synthesis)
- Crohn's disease (terminal ileum involvement)
- For Acalculous Cholecystitis:
- Critical illness (shock, sepsis, burns)
- Major surgery (especially cardiac, abdominal)
- Prolonged fasting/TPN
- Mechanical ventilation
- Immunosuppression
| Important – فكرة سؤال | |
| Acalculous cholecystitis typically occurs in ICU patients around postoperative day 3-5. Think of it in any critically ill patient with unexplained fever and RUQ tenderness. | تذكر |
Pathophysiology
- Initial cause: cystic duct obstruction → gallbladder distention, wall edema.
- Irritant: lysolecithin (from bile lecithin via phospholipase A), released by mucosal trauma.
- Wall findings: thickened, erythematous, subserosal hemorrhage; pericholecystic fluid.
- 5–10% progress to ischemia, necrosis; perforation usually contained by omentum.
- Bacterial infection in ~50% (E. coli most common); only 15–30% have infected bile.
- Initiating event: Cystic duct obstruction by gallstone
- Bile stasis → gallbladder distension
- Increased intraluminal pressure
- Venous and lymphatic compromise
- Inflammatory cascade:
- Mucosal trauma releases phospholipase A
- Lecithin → lysolecithin (mucosal irritant)
- Prostaglandin-mediated inflammation
- Neutrophilic infiltration of gallbladder wall
- Secondary bacterial infection (in 50% of cases; only 15–30% have infected bile):
- E. coli (most common)
- Klebsiella, Enterococcus
- Bacteroides (anaerobe)
- Natural progression:
- Edema → Ischemia → Gangrene → Perforation
- 5-10% progress to gangrene/perforation if untreated
Clinical Presentation
- Classic triad:
- RUQ pain
- Fever
- Leukocytosis
- Pain characteristics:
- Persistent RUQ or epigastric pain >4-6 hours (unlike biliary colic <4 hours)
- May radiate to right shoulder/scapula (phrenic nerve irritation)
- Worsens with fatty meals
- Associated with nausea/vomiting
- Physical examination:
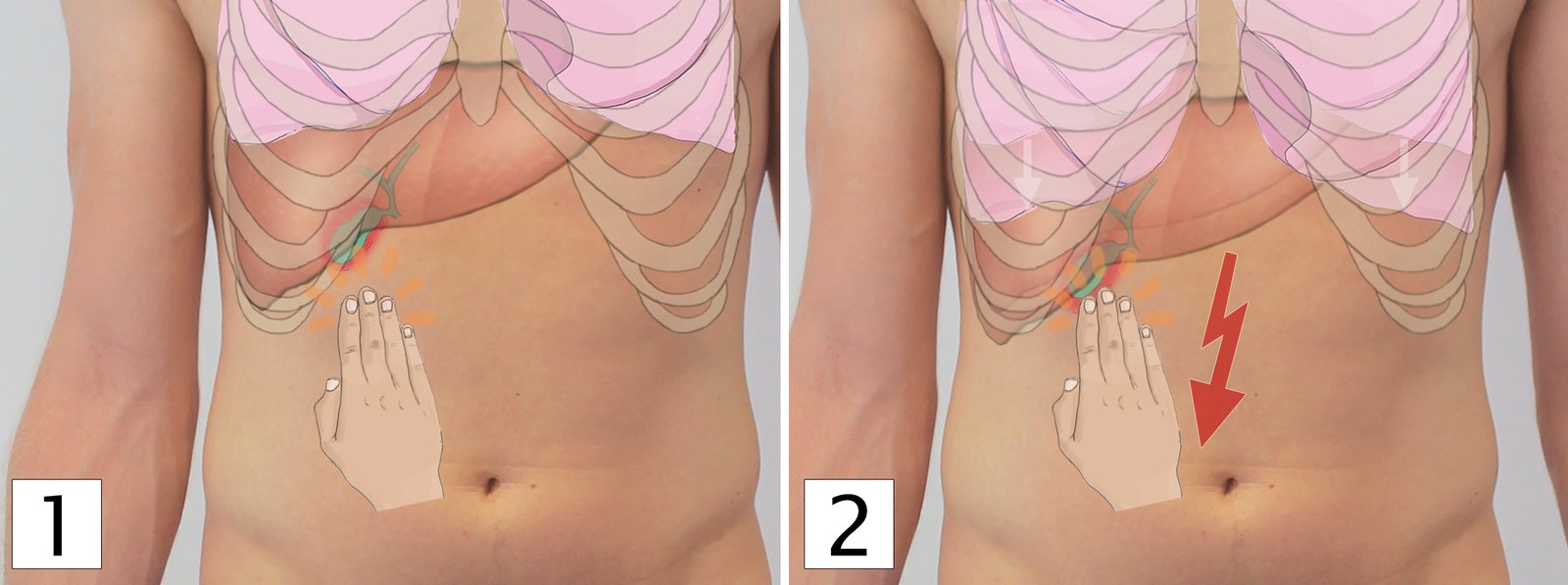
- Murphy's sign: Inspiratory arrest during RUQ palpation (65% sensitivity, 87% specificity)
- Boas' sign: Hyperesthesia below right scapula
- RUQ tenderness with guarding
- Palpable gallbladder mass (20% of cases)
- Low-grade fever (38-38.5°C)
| Clinical Pearl | |
| Elderly and diabetic patients may present atypically with minimal pain or fever. Have a high index of suspicion in these populations. | ملاحظة |
Diagnosis
- Laboratory findings:
- Leukocytosis (12,000-15,000/μL); >20,000 suggests complications
- Mild transaminase elevation (<3x normal)
- Bilirubin usually <4 mg/dL (if >4, consider choledocholithiasis or Mirizzi syndrome)
- Alkaline phosphatase mildly elevated
- Amylase/lipase normal (if elevated, consider gallstone pancreatitis)
- Imaging studies:
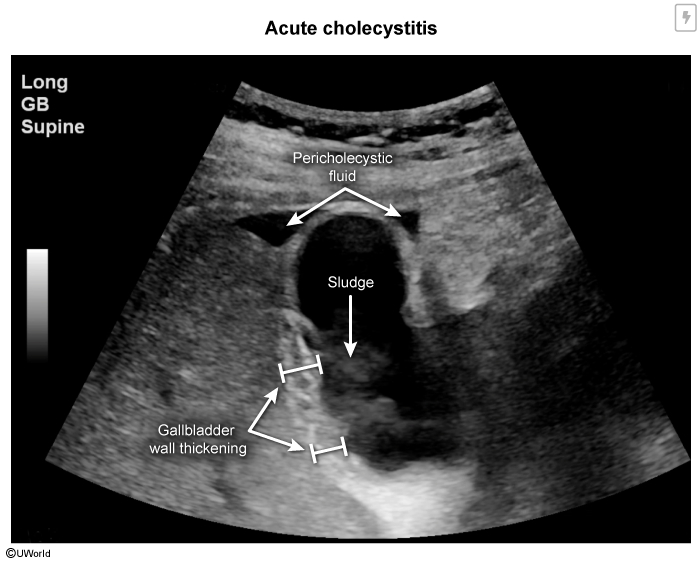
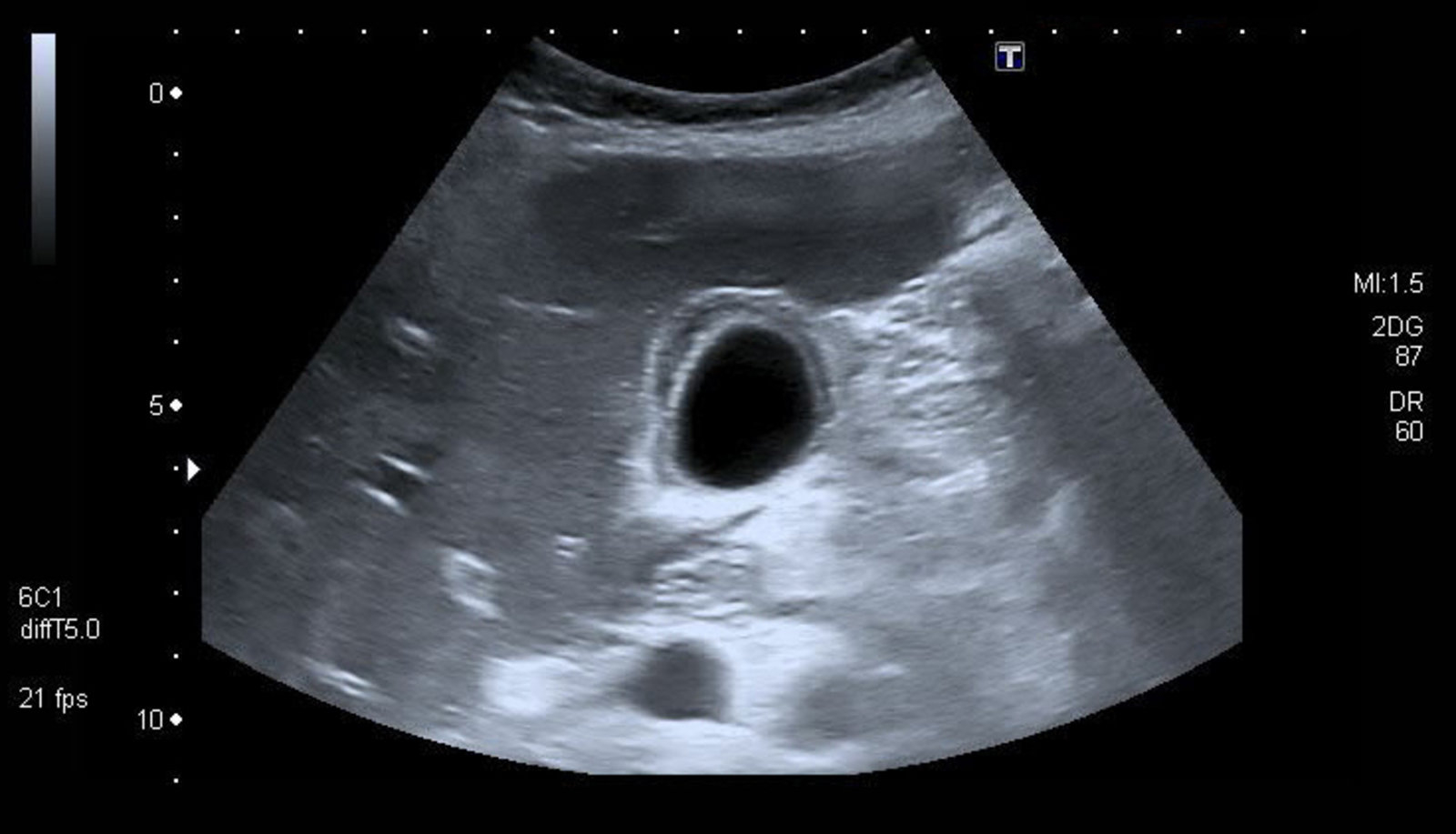
- Ultrasound (first-line):
- Gallbladder wall thickening >4 mm (most specific)
- Pericholecystic fluid
- Gallstones or sludge
- Sonographic Murphy's sign
- Gallbladder distension
- Sensitivity: 81%, Specificity: 83%
- HIDA scan (Hepatobiliary scintigraphy) (gold standard):
- Gold standard when ultrasound equivocal
- Non-visualization of gallbladder after 4 hours = positive
- Sensitivity: 97%, Specificity: 94%
- False positives: prolonged fasting, TPN, chronic cholecystitis
- CT scan:
- Better for complications (perforation, abscess)
- Shows gas in gallbladder wall (emphysematous cholecystitis)
- Alternative diagnoses
- Ultrasound (first-line):
Differential Diagnosis
| Differential Diagnosis of RUQ Pain | |||
|---|---|---|---|
| Condition | Key Features | Labs | Distinguishing Points |
| Biliary colic | Pain <4 hours, no fever | Normal WBC, LFTs | Self-limited, no inflammatory signs |
| Acute cholangitis | Charcot's triad: fever, jaundice, RUQ pain | ↑↑ Bilirubin, ↑ ALP | Jaundice prominent, septic appearance |
| Acute pancreatitis | Epigastric pain radiating to back | ↑↑ Lipase/amylase | Pain worse supine, better leaning forward |
| Peptic ulcer disease | Epigastric pain, relation to meals | Normal or ↑ amylase | No Murphy's sign, endoscopy diagnostic |
| Acute hepatitis | RUQ pain, jaundice | ↑↑↑ Transaminases (>1000) | Marked transaminase elevation |
| Right lower lobe pneumonia | Pleuritic chest pain, cough | ↑ WBC | Abnormal lung exam, CXR findings |
Management
- Initial supportive care:
- NPO (bowel rest) منع الأكل والشرب
- IV fluids for hydration
- Pain control (NSAIDs or opioids)
- Antiemetics for nausea
- NG decompression if severe vomiting
- Antibiotic therapy:
- Indicated for moderate/severe cases or high-risk patients
- Coverage for gram-negative and anaerobes:
- Options:
- Piperacillin-tazobactam
- Ceftriaxone + metronidazole
- Ciprofloxacin + metronidazole
- Definitive treatment:
- Early laparoscopic cholecystectomy within 72 hours
- Standard of care for acute cholecystitis
- Lower morbidity than delayed surgery
- Shorter hospital stay
- Conversion to open: 5-10%
- Percutaneous cholecystostomy (drainage):
- For high-risk surgical patients
- Bridge to elective cholecystectomy
- Keep drain 3-6 weeks minimum
- Interval cholecystectomy after 6-8 weeks
- Early laparoscopic cholecystectomy within 72 hours
| Important – فكرة سؤال | |
|
Early cholecystectomy (within 72 hours) is superior to delayed surgery. It results in shorter hospital stays and lower complication rates. |
تذكر |
Special Considerations
- Pregnancy:
- Second most common non-obstetric surgical emergency
- Laparoscopic cholecystectomy safe in all trimesters
- Best timing: second trimester
Key Takeaways
| Acute Cholecystitis - Summary | |
|---|---|
| Clinical Diagnosis |
|
| Diagnostic Tests |
|
| Management |
|
| Complications |
|
| Remember: Early surgery is better than delayed surgery. Always consider acalculous cholecystitis in critically ill patients with fever and RUQ tenderness. | |
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.