سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Background
- Diseases of the salivary glands include sialadenosis, sialodenitis, sialolithiasis and neoplasms
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Background Version 2
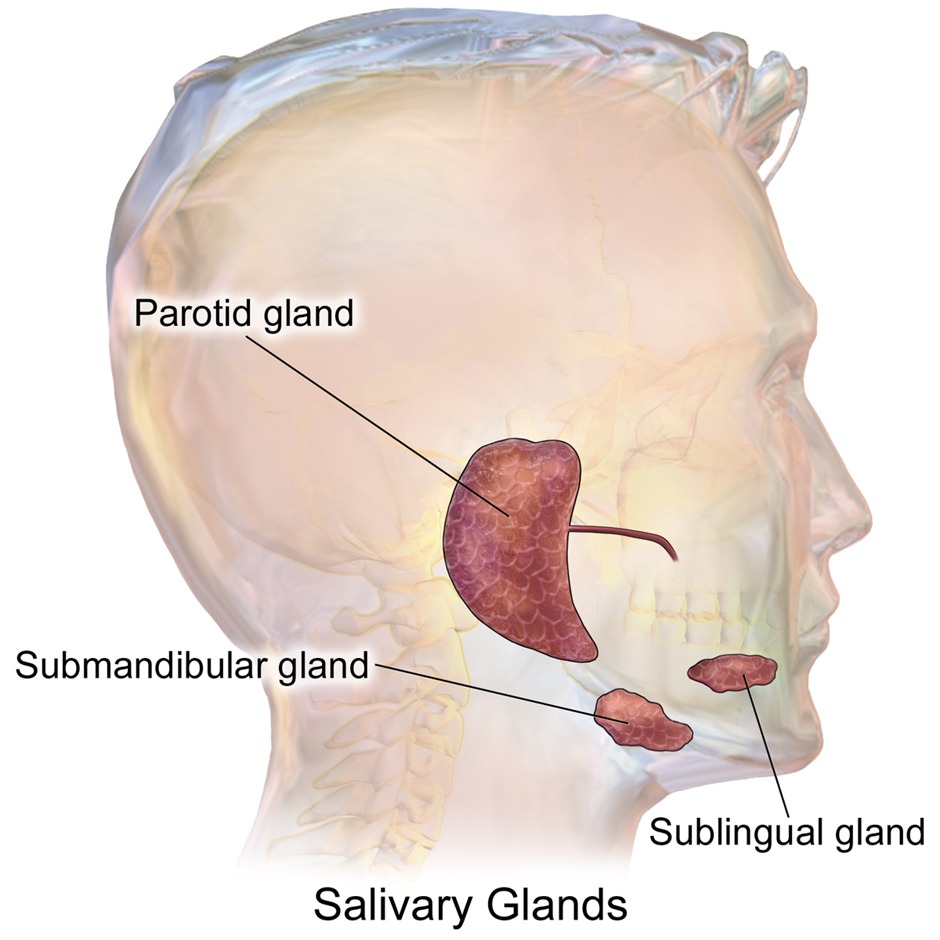
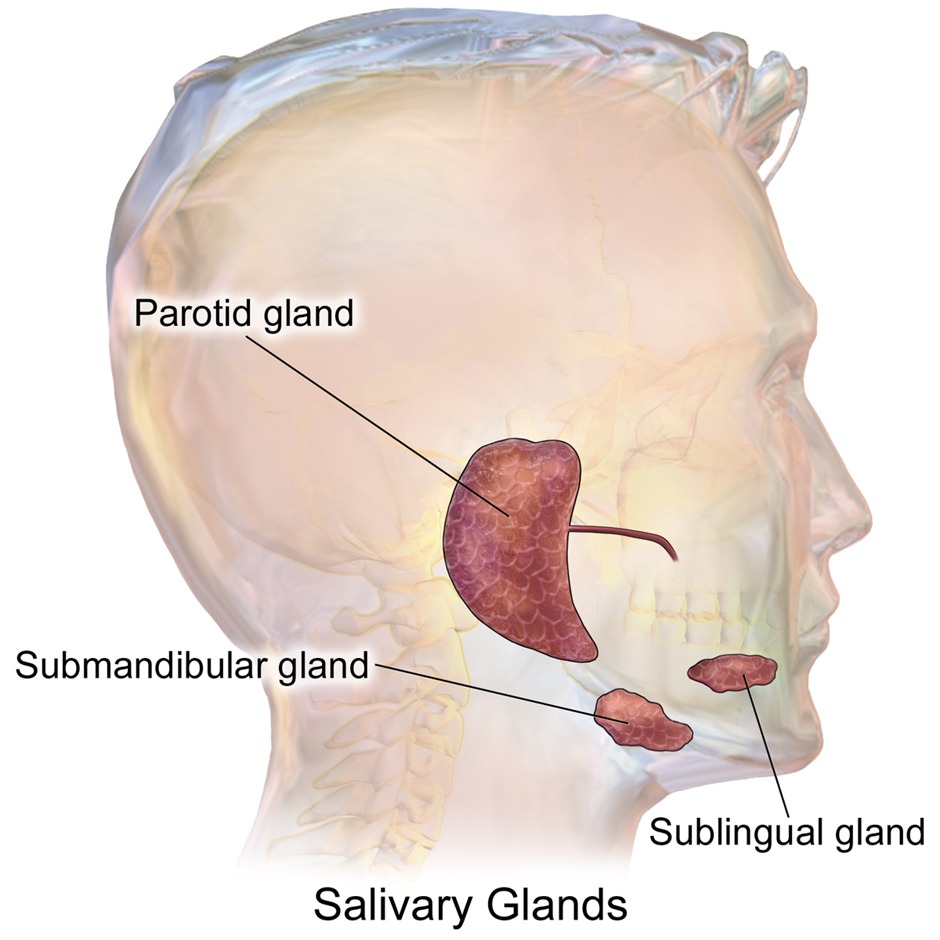
- Definition: Diseases affecting the major salivary glands (parotid, submandibular, sublingual) and minor salivary glands
- Epidemiology:
- Sialolithiasis: ★Most common (1% of population)
- Acute sialadenitis: 0.01-0.02% hospital admissions
- Salivary tumors: 3-4% of all head/neck tumors
- Key anatomical relationships:
- Parotid: Facial nerve runs through it
- Submandibular: Wharton's duct opens near frenulum
- Sublingual: Multiple small ducts (Rivinus ducts)
| Comparison of Major Salivary Gland Disorders | |||||
|---|---|---|---|---|---|
| Feature | Sialadenosis | Sialolithiasis ★ | Acute Sialadenitis | Chronic Sialadenitis | Tumors |
| Most common location | Parotid (bilateral) | Submandibular (80%) | Parotid | Parotid | Parotid (80%) |
| Age group | Adults 40-60 | Adults 30-60 | Elderly, postop | Any age | Adults >40 |
| Pain | Painless | Painful with meals | Painful, constant | Intermittent pain | Usually painless |
| Key finding | Bilateral swelling | "Salivary colic" | Purulent discharge | Recurrent swelling | Facial palsy = malignant |
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Sialadenosis
| Sialadenosis | |
| Definition |
|
| Clinical presentation |
|
| Risk factors |
|
| Differential diagnosis |
|
| Treatment |
|
Version 2
| Sialadenosis (Sialosis) | |
| Definition |
|
| Epidemiology |
|
| Clinical presentation |
|
| Risk factors/Causes |
|
| Diagnosis |
|
| Treatment |
|
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Sialolithiasis
| Sialolithiasis | |
| Definition |
|
| Risk factors |
|
| Clinical presentation |
|
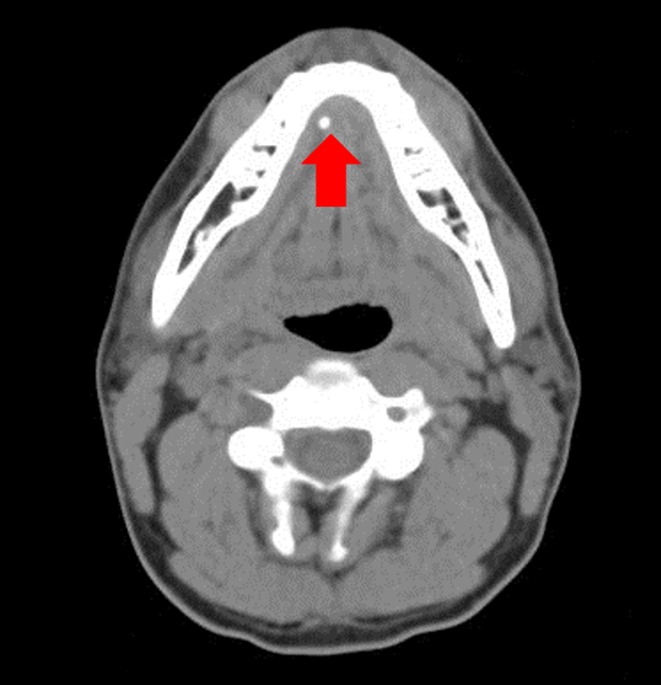
| Diagnosis |
|
| Treatment |
|
Version 2
| Sialolithiasis (Salivary Stones) | |
| Definition |
|
| Pathophysiology |
|
| Clinical presentation |
|
| Diagnosis |
|
| Treatment |
|
| Complications |
|
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Sialadenitis
| Sialadenitis | |
| Definition |
|
| Microbiology |
|
| Risk factors |
|
| Clinical presentation |
|
| Diagnosis |
|
| Treatment |
|
Version 2
| Acute Sialadenitis | |
| Definition |
|
| Types |
|
| Risk factors |
|
| Clinical presentation |
|
| Diagnosis |
|
| Treatment |
|
| Complications |
|
💡 CLINICAL PEARLS
- Pus from Stensen's duct = Acute bacterial parotitis (pathognomonic)
- Bilateral parotid swelling + orchitis = Mumps until proven otherwise
- "Chipmunk cheeks" = Classic description for bilateral parotid swelling
- Stone palpable in floor of mouth = Submandibular sialolithiasis
Chronic Sialadenitis
| Definition |
|
| Causes |
|
| Clinical features |
|
| Diagnosis |
|
| Treatment |
|
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
CLINICAL PEARLS - Version 2
- Pus from Stensen's duct = Acute bacterial parotitis (pathognomonic)
- Bilateral parotid swelling + orchitis = Mumps until proven otherwise
- "Chipmunk cheeks" = Classic description for bilateral parotid swelling
- Stone palpable in floor of mouth = Submandibular sialolithiasis
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
HIGH-YIELD FACTS - Version 2
⭐ HIGH-YIELD FACTS
- Most common salivary gland disorder overall: Sialolithiasis (80% in submandibular gland)
- Most common cause of bilateral parotid swelling: Mumps (viral sialadenitis)
- Most common salivary gland tumor: Pleomorphic adenoma (benign)
- Pathognomonic sign: Facial nerve palsy = malignant parotid tumor until proven otherwise
- Classic triad of chronic sialadenitis: Pain + swelling + occurs with meals
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.
فيديوهات الشرح
بطاقات تفاعلية
أسئلة ممارسة
اشترك الآن