Summary
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Introduction
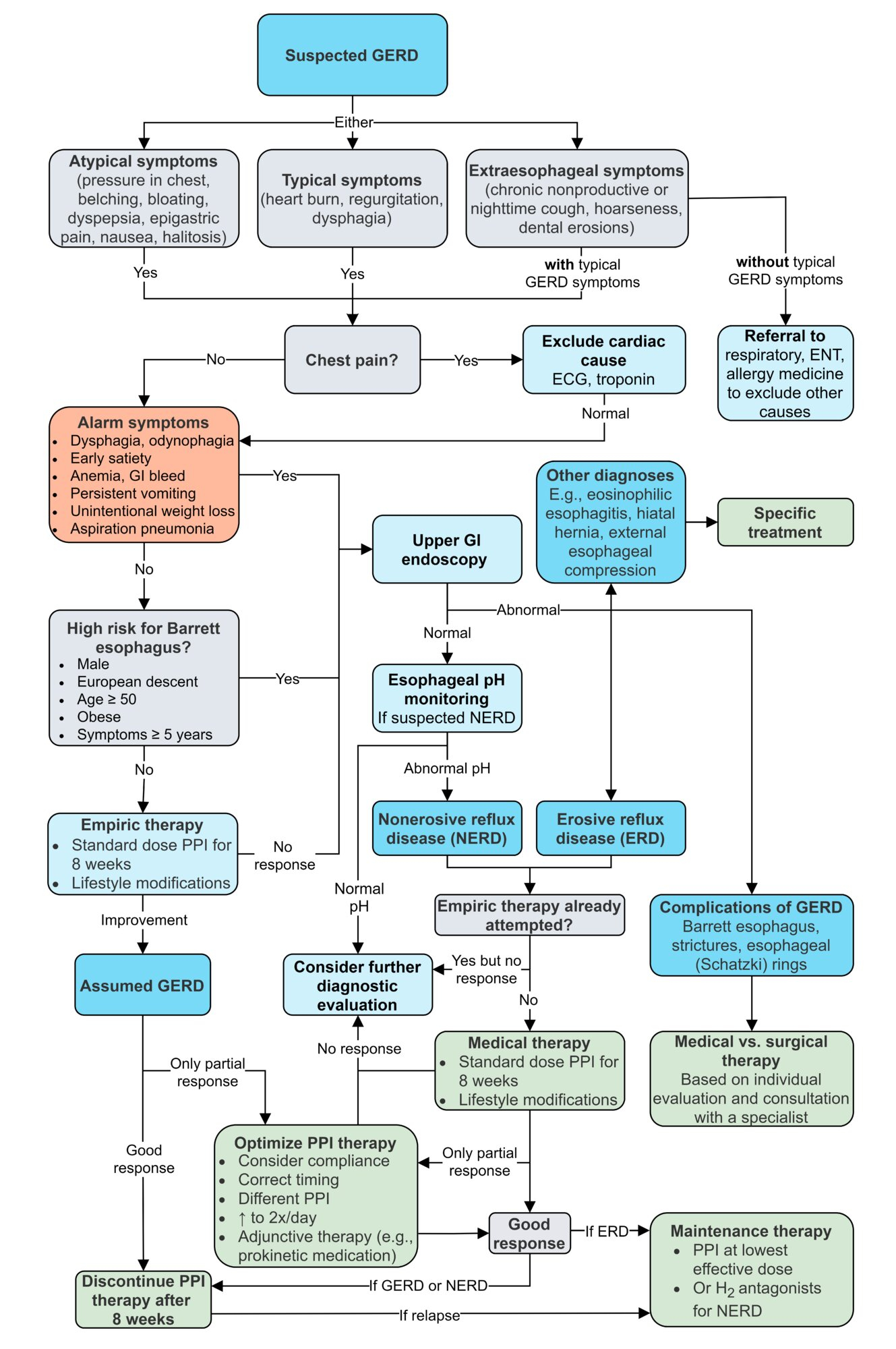
- Gastroesophageal reflux (GER) is the normal physiologic state in which stomach contents move retrograde into the esophagus.
- Gastroesophageal reflux disease (GERD) is characterized by transient inappropriate decrease in lower esophageal sphincter tone which allows excessive gastric refluxate to enter the esophagus and even the oropharynx.
- GERD presents as heartburn, regurgitation, and dysphagia.
- This condition is also associated with respiratory symptoms such as chronic cough, hoarseness and it may exacerbate asthma.
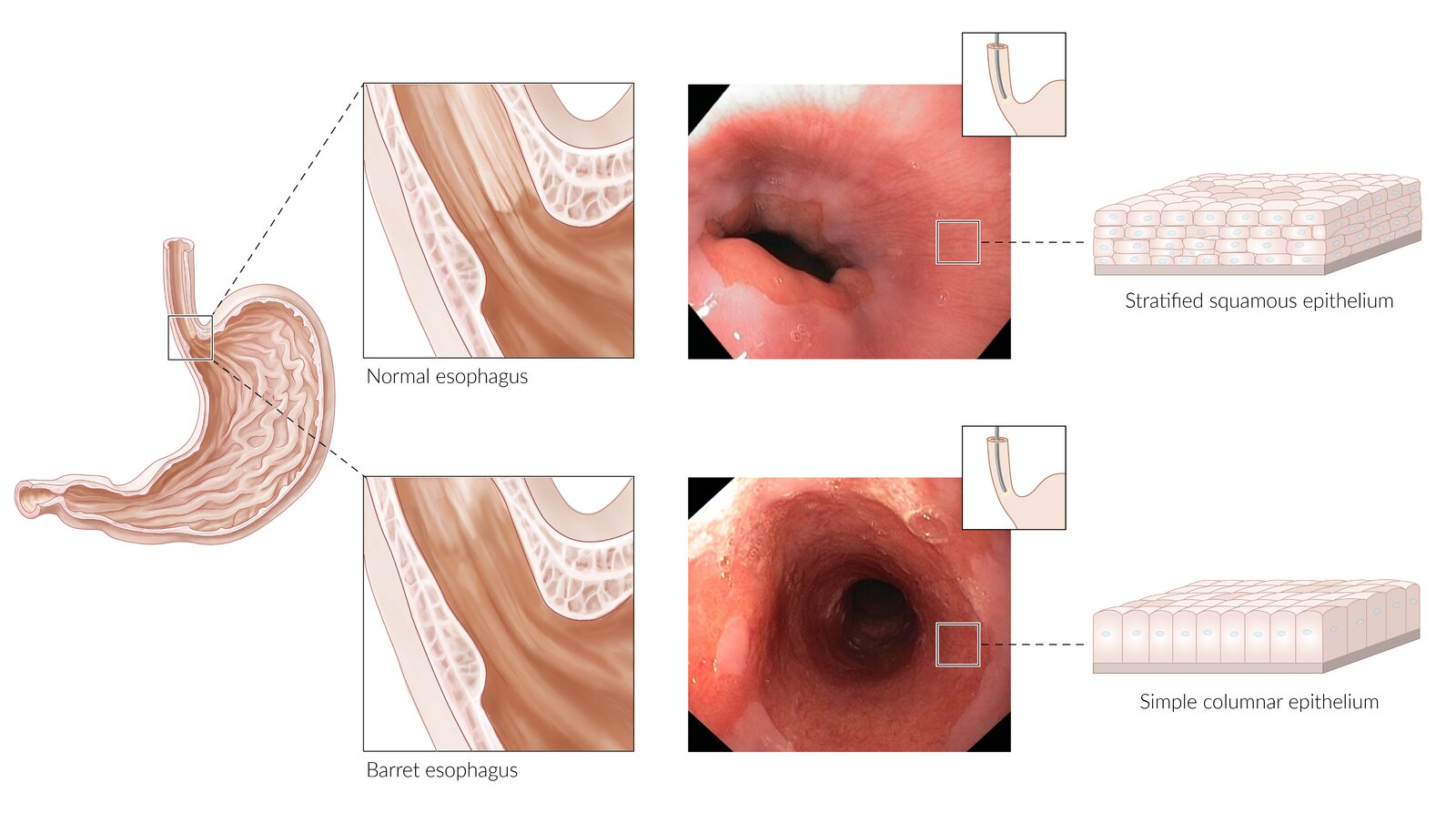
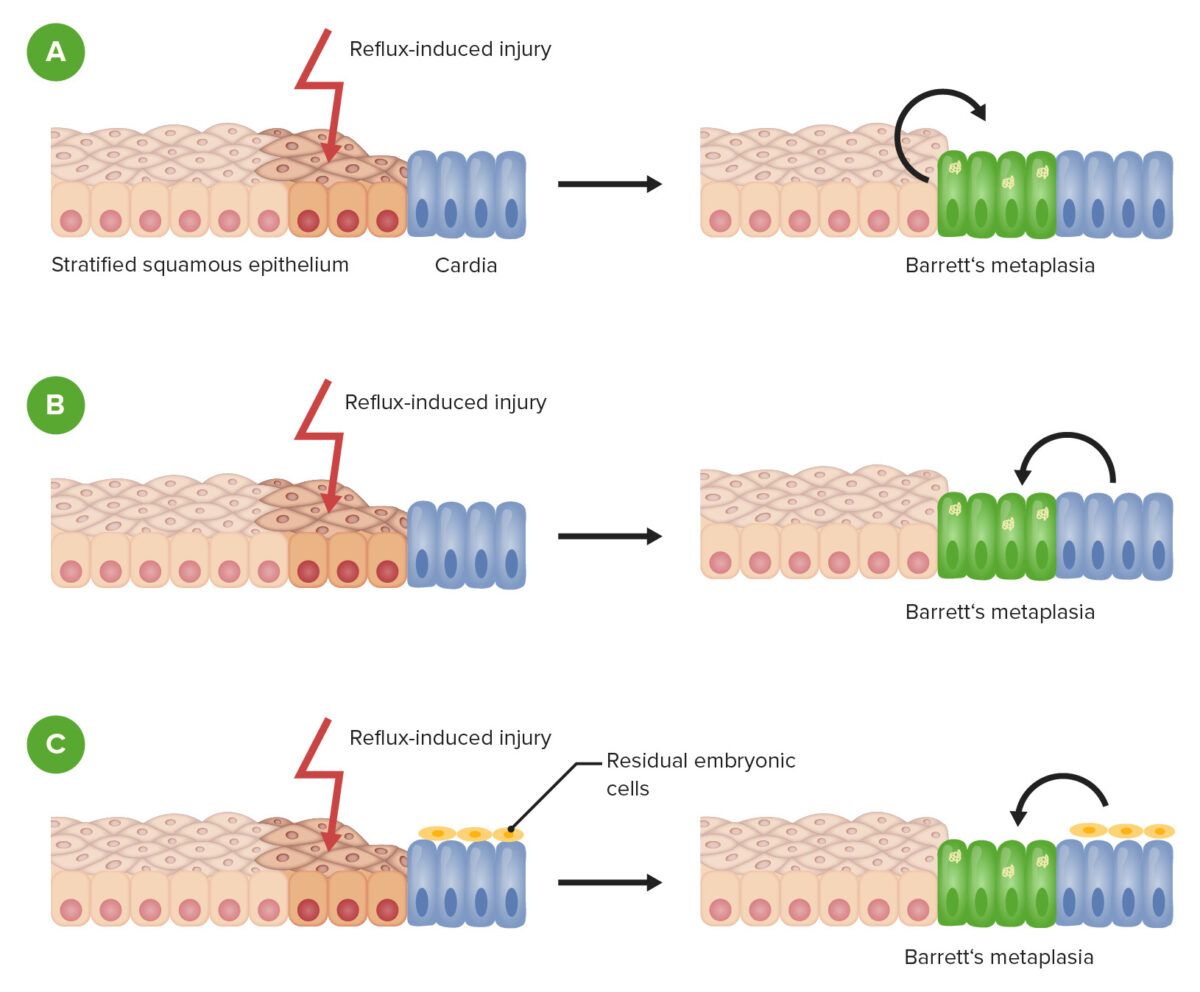
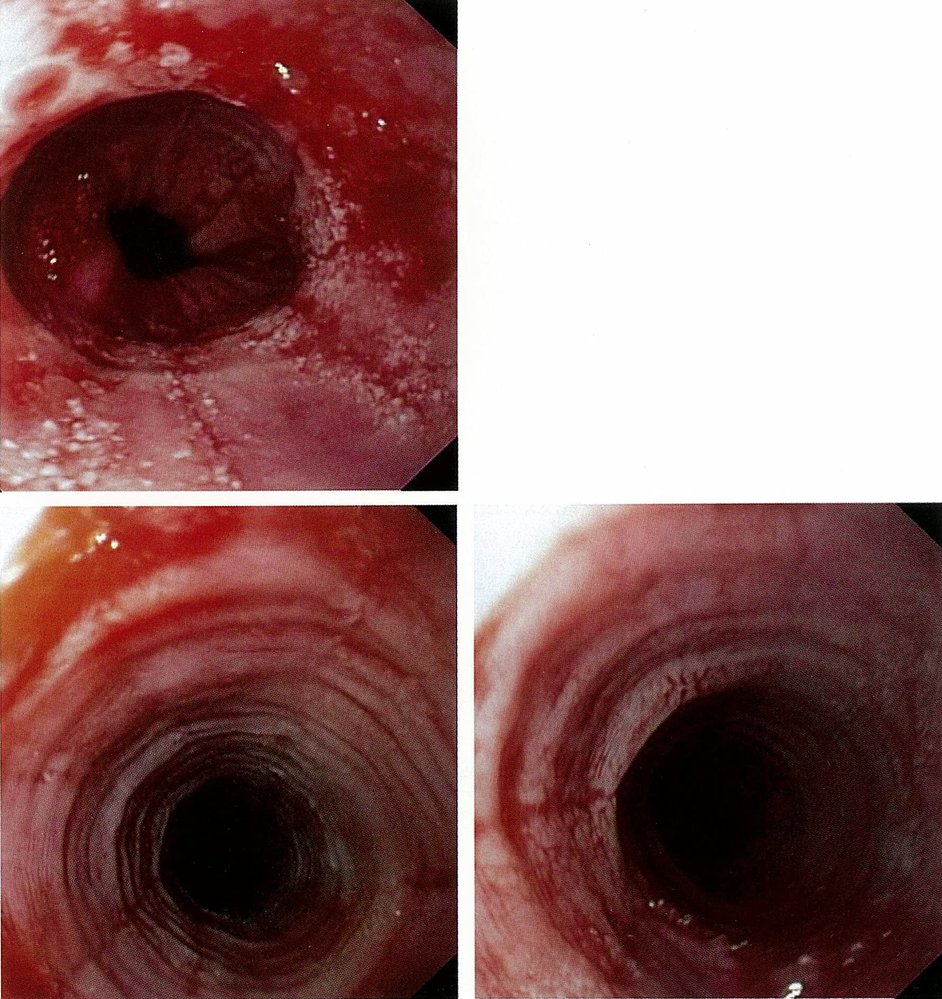
- Complications include erosive esophagitis, strictures, and Barrett esophagus.
| Gastroesophageal Reflux Disease (GERD) | |
|---|---|
| Pathophysiology |
|
| Manifestations |
|
| Complications |
|
| Initial Treatment |
|
| Barrett Esophagus | |
|---|---|
| Definition |
|
| Location |
|
| Etiology |
|
| Associations |
|
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Epidemiology
- GERD is one of the most common gastrointestinal disorders (approximately 20% of adults).
- This condition presents higher in girls compared with boys.
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Etiology
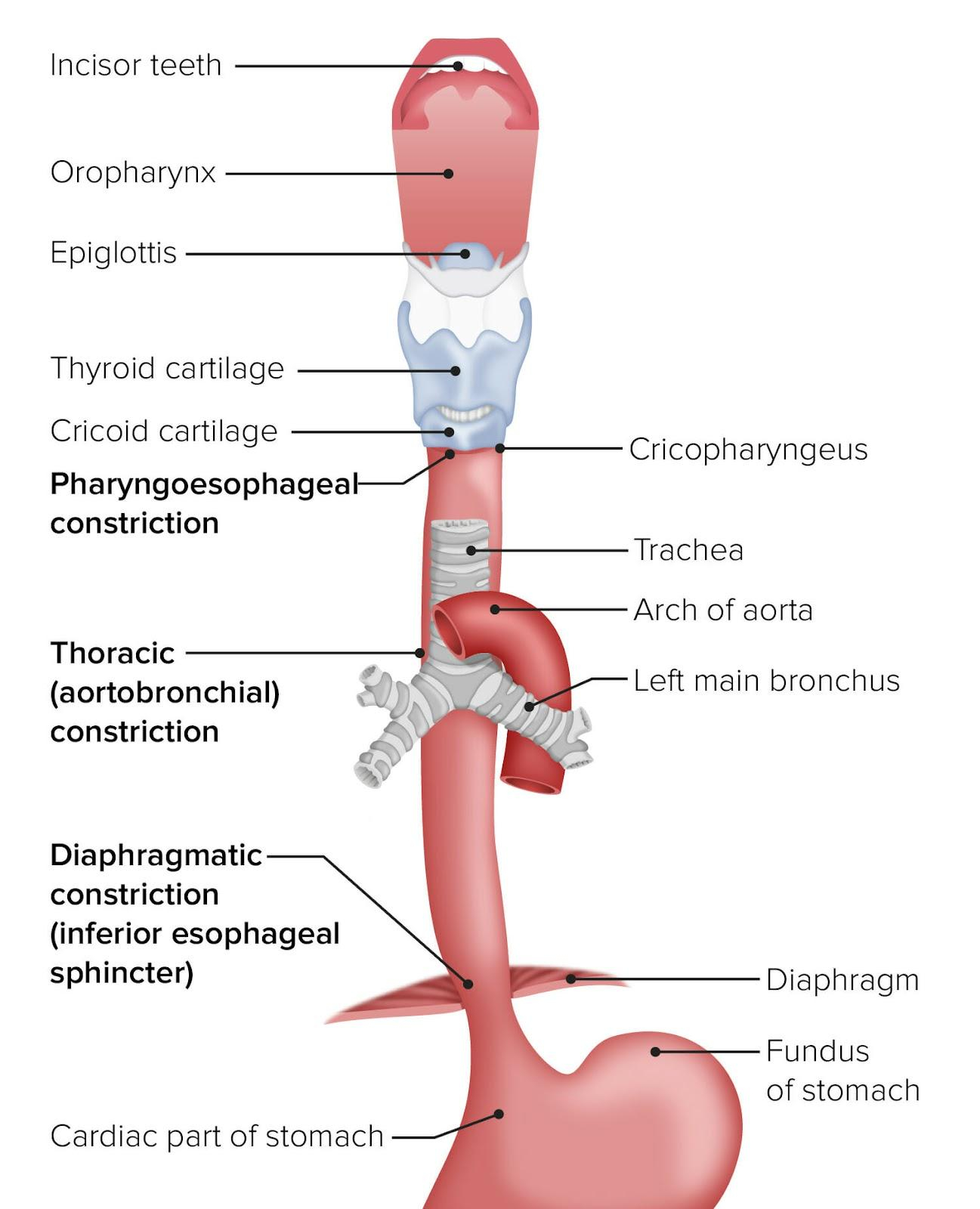
- Impaired lower esophageal sphincter (LES) function and transient lower esophageal sphincter relaxations (TLESRs)
- Acidic refluxate from the stomach enters the esophagus and oropharynx.
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Presentation of physiologic reflux (GER)
- Infants are often termed “happy spitters” (they are without reflux-associated symptoms).
- Emesis is benign.
- Education and reassurance of parents are important (to avoid aimless formula changes, early weaning, medications or remedies).
- Emesis from physiology reflux resolves by 6-12 months of age.
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Presentation of pathological reflux (GERD)
- Presentation of pathological reflux is different based on the age of the child affected.
| Difference in Presentation of Gastroesophageal Reflux Disease Based on Age | |
| Infants | Older Children |
|
|
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Diagnosis
- pH probe measurement (the gold standard for diagnosis)
- Barium upper gastrointestinal study
- Gastric emptying study
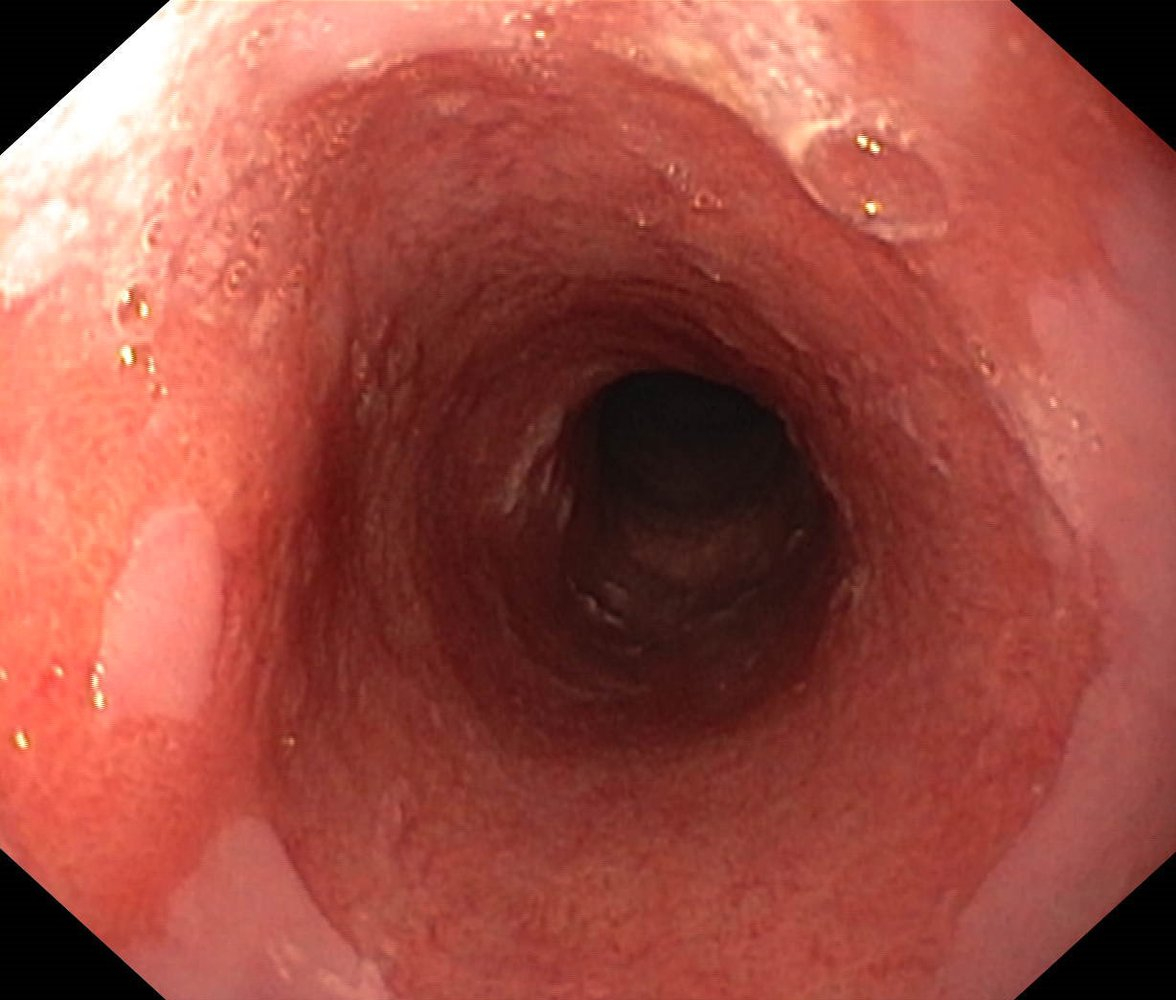
- Endoscopy with biopsy (detects inflammation)
- Bronchoscopy with alveolar lavage (when aspiration is suspected)
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Differential diagnosis
- Milk protein allergy
- Pyloric stenosis
| Differential Diagnosis of Regurgitation and Vomiting in Infants | ||
|---|---|---|
| Diagnosis | Clinical Features | Management |
| Gastroesophageal Reflux |
|
|
|
|
|
| Milk Protein Allergy |
|
|
| Pyloric Stenosis |
|
|
| Infantile Hypertrophic Pyloric Stenosis | |
|---|---|
| Risk Factors |
|
| Clinical Presentation |
|
| Associations |
|
| Laboratory Findings |
|
| Diagnostic Studies |
|
| Treatment |
|
| Protein Intolerance Leading to Malabsorption | |
|---|---|
| Epidemiology |
|
| Clinical Features |
|
| Diagnosis |
|
| Management |
|
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Treatment
- Conservative management
- Positioning in an upright or sitting position (raise the head of the bed after feeding or when asleep)
- Dietary recommendations (frequent small meals and thickening of feeds)
- Acid inhibition with antacids, histamine 2 receptor blockers, and proton pump inhibitors
- Surgical management
- Nissen fundoplication (wrapping the fundus of the stomach around the distal esophagus)
- Pyloroplasty (to improve gastric emptying)
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Complications
- Upper and lower airway disease may be induced or worsened by GERD (acidic refluxate induces bronchopulmonary constriction and can also lead to frank aspiration or microaspiration)
- Chronic laryngitis, hoarseness, wheezing and the development of vocal cord nodules.
- Failure to thrive
- Esophageal strictures
- Barrett esophagus
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.
فيديوهات الشرح
بطاقات تفاعلية
أسئلة ممارسة
اشترك الآن