Definition
Preterm labor is defined as the onset of regular uterine contractions that lead to cervical effacement, dilation, or both before 37 weeks of gestation.
Classification of prematurity categorized by birth weight or gestational age
|
Birth weight |
|
|
Low birth weight (LBW) |
<2500 g |
|
Very low birth weight (VLBW) |
<1500 g |
|
Extremely low birth weight (ELBW) |
<1000 g |
|
Gestational age |
|
|
Term |
≥37 weeks |
|
Late preterm |
34 weeks to <37 weeks |
|
Moderate preterm |
32 weeks to <34 weeks |
|
Very preterm |
<32 weeks |
|
Extremely preterm |
<28 weeks |
The pathogenesis
- Stress-induced premature activation of the maternal or fetal hypothalamic-pituitary-adrenal axis, which may initiate labor through increased production of corticotropin-releasing hormone.
- Exaggerated inflammatory response, infection, or alterations in the genital tract microbiome, which can provoke premature labor through the production of pro-inflammatory cytokines.
- Decidual hemorrhage, which can disrupt the maternal-fetal interface and lead to the release of pro-labor substances.
- Pathological uterine distention, resulting from conditions like polyhydramnios or multiple gestations, can stretch the uterus and activate labor pathways.
Clinical Findings
- Menstrual-like Cramping: Similar to the discomfort experienced during menstrual periods.
- Mild, Irregular Contractions: Unlike the consistent and regular contractions seen in true labor, these are less regular and may not result in cervical changes.
- Low Back Ache: A common discomfort associated with labor, presenting as a continuous dull pain in the lower back.
- Pressure Sensation in the Vagina or Pelvis: Feeling of pressure or fullness, indicating the baby is moving lower into the pelvis.
- Vaginal Discharge of Mucus: The discharge may be clear, pink, or slightly bloody, signifying the expulsion of the mucus plug (bloody show).
- Spotting, Light Bleeding: Slight vaginal bleeding can occur as the cervix begins to change in preparation for labor.
Distinguishing True from False Labor
| Criteria | True Labor | False Labor (Braxton Hicks Contractions) |
| Contraction Nature | Regular contractions resulting in cervical change | Mild and irregular contractions |
| Cervical Changes | Dilation, effacement, softening, and anterior positioning | No significant cervical change |
| Frequency of Contractions | Increasing frequency | May increase transiently, especially at night |
| Intensity and Duration | Increasing intensity and duration | Might not have a significant increase in intensity or duration |
| Commonality | True labor is definitive with cervical changes | Common at all stages of pregnancy, adding complexity to diagnosing true labor |
Risk factors
- Prior OB/GYN history
- Prior PTB (especially multiple PTBs or PTB at an early gestational age)
- Prior cervical surgery (eg, cone biopsy, LEEP)
- Multiple D&Es
- Uterine anomalies
- Maternal demographics
- <17 or >35 years of age
- Non-Hispanic Black race, Indigenous women
- Lower educational level (eg, <12 grades)
- Single marital status
- Lower socioeconomic status
- Short interpregnancy interval (eg, <18 months)
- Other social factors (eg, poor access to medical care, physical abuse, acculturation)
- Nutritional status/physical activity
- BMI <18.5 kg/m2 or prepregnancy weight <50 kg (<120 lb)
- Poor nutritional status
- Long working hours (eg, >80 hours/week)
- Hard physical labor (eg, shift work, standing >8 hours)
- Current maternal/pregnancy characteristics
- Conception by assisted reproductive technology (eg, IVF)
- Multiple gestation
- Fetal disorder (eg, chromosome anomaly, structural abnormality, growth restriction, death, etc)
- Vaginal bleeding (eg, 1st and 2nd trimester, placenta previa, abruption)
- Poly- or oligohydramnios
- Maternal medical conditions (eg, hypertension, diabetes, thyroid disease, asthma, etc)
- Maternal abdominal surgery during pregnancy
- Psychological issues (eg, stress, depression, unplanned pregnancy)
- Substance use:
- Smoking (eg, tobacco)
- Heavy alcohol consumption
- Cocaine
- Heroin
- Infection:
- Bacterial vaginosis
- Trichomoniasis
- Chlamydia
- Gonorrhea
- Syphilis
- Urinary tract (eg, asymptomatic bacteriuria, pyelonephritis)
- Severe viral infection
- Intrauterine infection
- Short cervical length between 14 and 28 weeks
- Positive fFN between 22 and 34 weeks
- Uterine contractions
Components of the Diagnostic Evaluation for Suspected Preterm Labor
History and Initial Examinations
- Review obstetric and medical history, including risk factors for preterm birth. Screen for substance misuse as part of the review.
- Estimate gestational age using the first ultrasound examination. Perform an ultrasound for fetal biometry if necessary.
- Evaluate signs and symptoms of preterm labor, including contraction frequency, duration, and intensity.
- Examine the uterus for firmness, tenderness, fetal size, and position.
- Review the fetal heart rate tracing.
Speculum Examination
- Estimate cervical dilation; ≥3 cm supports the diagnosis of preterm labor.
- Assess uterine bleeding; important for identifying triggers like placental abruption or previa.
- Assess fetal membrane status (intact or ruptured).
- Collect a cervicovaginal fluid specimen for potential fetal fibronectin (fFN) testing.
Digital Cervical Examination
- Assess cervical dilation and effacement after excluding conditions like placenta previa and rupture of membranes. Cervical dilation >3 cm in the presence of contractions at 20+0 to 36+6 weeks supports the diagnosis of preterm labor.
Transvaginal Ultrasound Examination (TVUS)
- Measure cervical length; <30 mm before 34 weeks is predictive of increased risk for preterm birth, while ≥30 mm has a high negative predictive value.
Obstetric Ultrasound Examination
- Provides additional information including fetal, placental, and maternal anatomic abnormalities; fetal presentation; amniotic fluid volume; and estimated fetal weight.
Laboratory Evaluation
- Rectovaginal GBS culture, if not done within the previous five weeks.
- Urine culture to check for asymptomatic bacteriuria or pyelonephritis.
- fFN testing in pregnancies <34 weeks with intact membranes, cervical dilation <3 cm, and cervical length 20 to 30 mm.
- STI testing based on patient risk factors.
Fetal Fibronectin (fFN) for Selected Patients
- fFN testing distinguishes true from false labor, predicting the risk of preterm birth. A positive fFN result indicates an increased risk of preterm birth within seven days.
Diagnosis of Preterm Labor
- Uterine Contractions: At least 6 contractions within a 60-minute period, plus one or more of the following:
- Cervical Dilation: ≥3 cm
- Cervical Length on Transvaginal Ultrasound: <20 mm
- Cervical Length on Transvaginal Ultrasound: 20 to <30 mm and a positive fetal fibronectin test
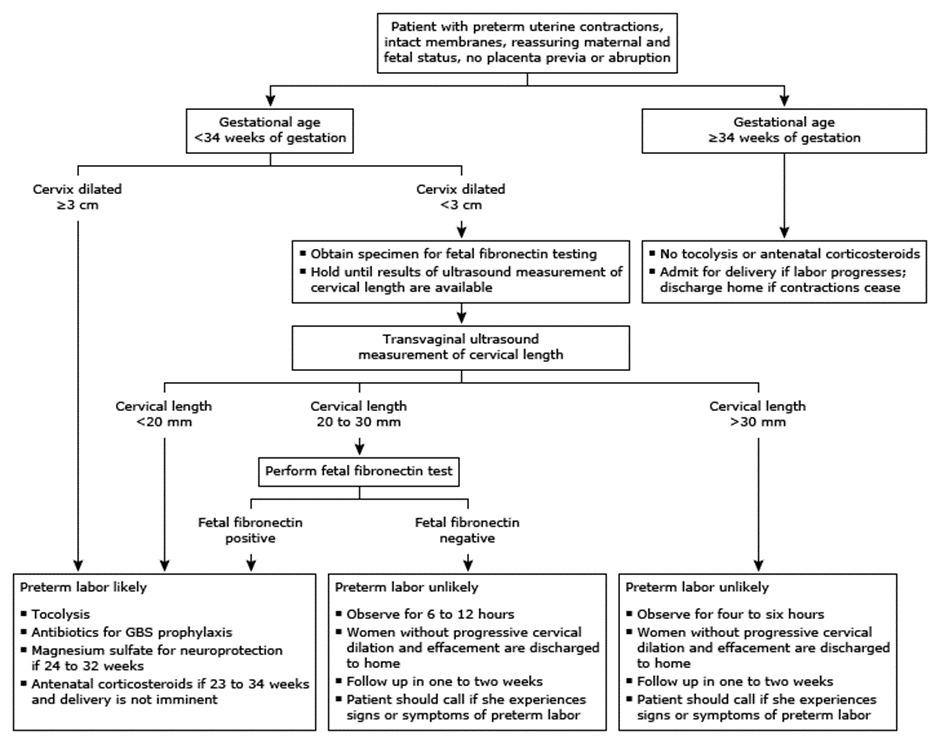
Approach to Triage
For Gestations ≥34 Weeks
Patients suspected of preterm labor at ≥34 weeks are admitted for observation. After 4-6 hours:
- Not in Labor: Discharge if no progressive cervical changes and fetal well-being confirmed. Instructions for follow-up and when to call for preterm labor signs or pregnancy concerns are provided.
- In Labor: Manage according to labor progression.
For Gestations <34 Weeks
Patients with contractions and intact membranes at <34 weeks are evaluated upon admission.
- Cervical Dilation ≥3 cm: Indicates preterm labor. Sonographic cervical length or fetal fibronectin (fFN) tests are not performed as these do not improve diagnostic accuracy. Management focuses on reducing preterm birth morbidity and mortality.
- Cervical Dilation <3 cm: Diagnosis is less clear. Approach involves cervical length measurement and possibly fFN testing for those with cervical length 20 to <30 mm to assess preterm birth risk.
- Cervical Length 20 to <30 mm: fFN testing is considered for symptomatic patients. A positive fFN leads to interventions to reduce preterm birth morbidity. If negative, patients are discharged after 6-12 hours of observation due to the high negative predictive value.
- Cervical Length <20 mm: These patients are at a high risk of preterm birth within seven days. Interventions to reduce morbidity associated with preterm birth are initiated without fFN testing.
- Cervical Length ≥30 mm: Patients are at low risk of preterm birth within seven days. They do not require fFN testing. After an observation period, patients without progressive cervical changes are discharged.
INITIAL TREATMENT OF PRETERM LABOR <34 WEEKS
|
Treatment Component |
Description |
|
Antenatal Corticosteroids |
|
|
Tocolytics |
|
|
GBS Prophylaxis |
|
|
Neuroprotection |
|
Antenatal Corticosteroid Therapy
| Gestational Age | Consideration | Dosing | Timing for Optimal Efficacy |
|
21+0 to 22+6 weeks |
ACS considered for expected delivery within 7 days after thorough counseling. |
- |
- |
|
23+0 to 33+6 weeks |
ACS strongly recommended for high risk of preterm birth within 7 days. |
Betamethasone: 12 mg IM every 24 hours x 2 doses or Dexamethasone: 6 mg IM every 12 hours x 4 doses. |
Benefits start within hours, peaking 1-7 days after first dose. |
|
≥34+0 weeks (Cesarean 34+0 to 36+6 weeks) |
Shared decision-making for possible ACS administration. |
- |
- |
|
Vaginal Birth (Uncertain within 7 days) |
Not recommended |
- |
- |
|
Repeat Courses |
Limited to one dose/course before 34 weeks, only after 14 days since initial course, if high risk of delivery. |
Single 12 mg dose of betamethasone recommended for salvage therapy. |
- |
Tocolytics
Treatment Goals
- Delay Delivery: Extend pregnancy by at least 48 hours, enabling the full benefit of antenatal corticosteroids to enhance fetal lung maturity and reduce neonatal complications.
- Facilitate Safe Maternal Transfer: Provide time for the mother's transfer to a tertiary care facility, if needed, to ensure advanced neonatal care.
- Prolong Pregnancy: Continue the pregnancy safely when possible, especially in cases of self-limited conditions that might induce labor.
Gestational Age Considerations
- Lower Limit: Intervention might be reasonable from 22+0 weeks of gestation, depending on the likelihood of recurring preterm labor and potential benefits of delaying delivery.
- Upper Limit: Beyond 34+0 weeks of gestation, the risks associated with tocolytic therapy usually outweigh the benefits due to lower perinatal morbidity and mortality.
First-Line Therapy
- For patients ≤32+0 weeks of gestation without contraindications, indomethacin is preferred.
- Beyond 32+0 weeks up to ≤34+0 weeks, nifedipine is recommended due to potential adverse fetal effects associated with indomethacin.
Second-Line Therapy
- If initial treatment fails, switching to another tocolytic agent is advised, avoiding simultaneous use of multiple drugs due to increased risk of side effects.
Duration and Retreatment
- Tocolysis is generally discontinued 48 hours after initiating antenatal corticosteroids.
- In cases of recurrent preterm labor, the decision to retreat should mirror the initial episode's criteria.
Most Effective Tocolytic Drugs
- Cyclooxygenase Inhibitors (e.g., Indomethacin)
- Mechanism: Inhibits prostaglandin production, crucial in parturition.
- Efficacy: Demonstrated reduction in the risk of birth within 48 hours of treatment initiation.
- Side Effects: Include gastrointestinal discomfort and potential fetal risks such as ductus arteriosus constriction and oligohydramnios.
- Dose: A loading dose of 50 to 100 mg, followed by 25 mg every 4-6 hours, with careful monitoring for side effects.
- Calcium Channel Blockers (e.g., Nifedipine)
- Mechanism: Blocks calcium influx, leading to myometrial relaxation.
- Efficacy: Comparable to indomethacin with fewer maternal and fetal side effects.
- Side Effects: Primarily vascular, including headaches and potential hypotension.
- Dose: Initial loading dose of 20 to 30 mg, followed by 10 to 20 mg every 3 to 8 hours.
- Beta-Agonists (e.g., Terbutaline)
- Mechanism: Increases intracellular cAMP, causing myometrial relaxation.
- Efficacy: Effective in delaying delivery, though associated with significant maternal side effects.
- Side Effects: Cardiovascular effects such as tachycardia and hypotension, along with potential for hyperglycemia and hypokalemia.
- Dose: 0.25 mg subcutaneously every 20 to 30 minutes up to four doses or until labor is inhibited.
- Nitric Oxide Donors (e.g., Nitroglycerin)
- Mechanism: Induces smooth muscle relaxation through nitric oxide signaling.
- Efficacy: Limited effectiveness in delaying preterm birth compared to other tocolytics.
- Side Effects: Headache and maternal hypotension are common.
- Dose: Varies by administration route, with careful monitoring for blood pressure changes.
Less Effective Tocolytic Drugs
- Oxytocin Receptor Antagonists (e.g., Atosiban)
- Magnesium Sulfate
- Other Nitric Oxide Donors
Group B Streptococcus (GBS) prophylaxis
| Condition | Action | Notes |
| Known positive GBS culture | Administer GBS prophylaxis | If within previous 5 weeks |
| Preterm labor (unknown GBS status) | Obtain GBS cultures at presentation; administer antibiotic prophylaxis if fetus is potentially viable | Screening typically occurs at 36+0 to 37+6 weeks; early treatment if viability and labor is confirmed |
| Observation period (true labor not confirmed) | Discontinue GBS prophylaxis | If initial suspicion of preterm labor is not confirmed after observation |
| Recurrent preterm labor (within 5 weeks, negative culture) | No GBS prophylaxis needed | Applies if culture was negative and preterm labor recurs within 5 weeks |
| Recurrent preterm labor (more than 5 weeks after negative culture) | Treat as unknown colonization status; obtain cultures and consider prophylaxis based on viability and labor status | Cultures not predictive of GBS status for more than 5 weeks; re-assessment necessary |
| Approaching term (36+0 to 37+6 weeks) | Repeat vaginal-rectal culture | To update GBS status and guide management at term |
Neuroprotection
| Criteria | Treatment Recommendation | Notes |
| Risk of Preterm Birth | Suggest administration of magnesium sulfate | For pregnancies at high risk of preterm birth within 24 hours. |
| Gestational Age | Limit therapy to <32 weeks of gestation | Therapy is for pregnancies that have reached a gestational age where neonatal interventions are opted for by the mother but are less than 32 weeks of gestation. |
| Dose | Administer a 4 g IV loading dose over 20 minutes followed by a 1 g/hour infusion | |
| Duration | Discontinue at birth or by 24 hours after initiation of the infusion if birth has not occurred | |
| Emergency Delivery | Do not delay emergency delivery for magnesium sulfate administration | |
| Retreatment | Suggest not retreating if the patient does not give birth after an initial course of magnesium sulfate therapy (Grade 2C) |
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.