سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Background
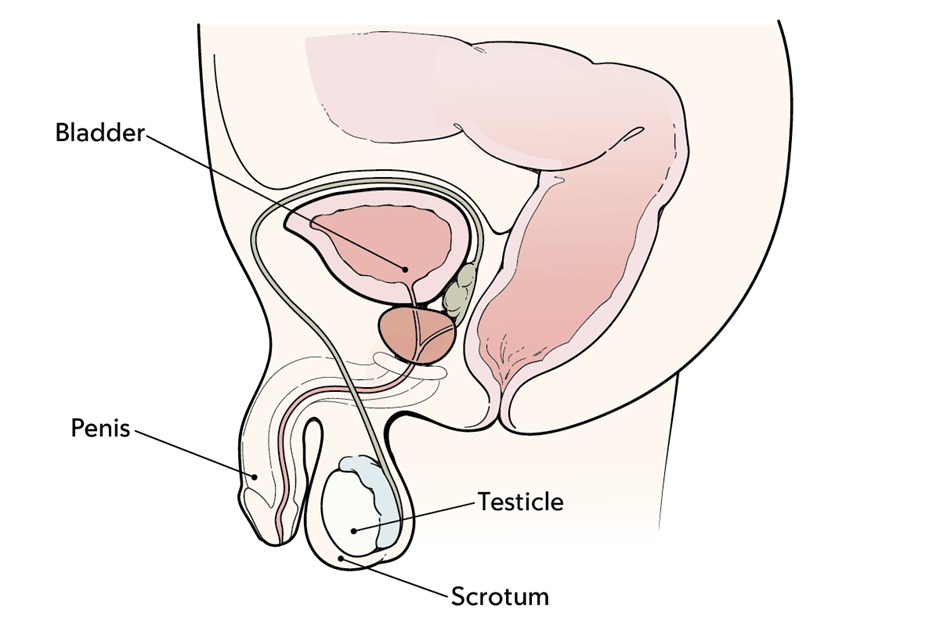
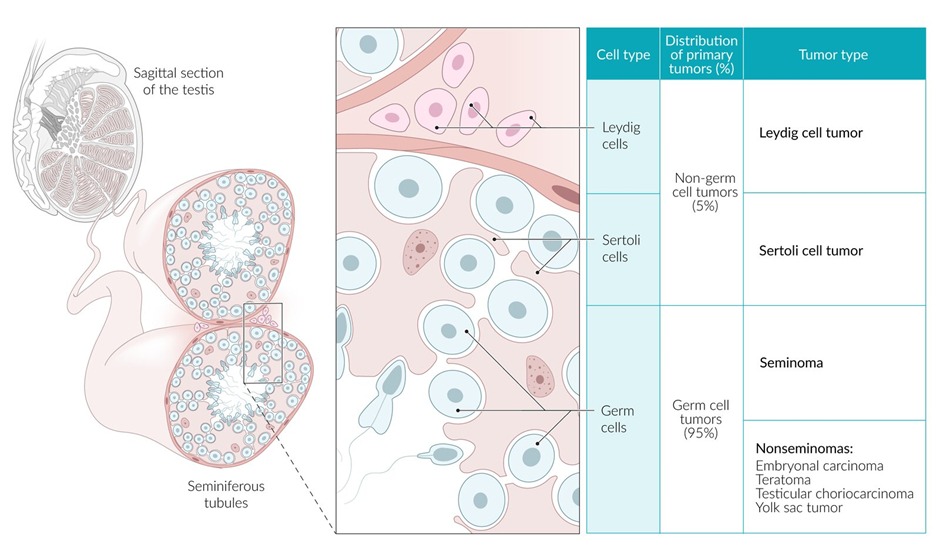
- Testicular malignancy can be divided into germ cell tumors (seminoma and nonseminoma) that are usually malignant and sex cord-stromal tumors that are usually benign
- Testicular cancer is usually more common in men 15 - 35 years of age
- Risk factors include: cryptorchidism, family history and infertility
- Germ cell tumors account for 95% of all testicular cancers (arise from germ cells that produce sperms)
- Testicular cancers do not transilluminate
- Testicular cancers are usually not biopsies (risk of seeding scrotum)
| Testicular Tumors | |
| Germ cell tumors | |
| Seminoma |
|
| Embryonal |
|
| Choriocarcinoma |
|
| Yolk sac tumor |
|
| Teratoma |
|
| Sex cord-stromal tumors | |
| Leydig cell tumor |
|
| Sertoli cell tumor |
|
| Non-Hodgkin Lymphomas | |
| Testicular lymphoma |
|
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Clinical features
- Symptoms
- Painless nodule or swelling in one testicle (usually)
- Physical exam
- Firm, hard, or fixed mass (must be considered testicular cancer until proven otherwise)
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Diagnosis
Imaging
- Ultrasonography (bilaterally)
Ultrasound findings in Seminomas and Nonseminomatous germ cell tumors Seminoma - Seminomas show hypoechoic lesions WITHOUT cystic findings
Nonseminomatous germ cell tumors - Nonseminomatous germ cell tumors can show (inhomogeneous lesions, calcifications, cystic areas and indistinct margins)
- Radiography (to assess for mediastinal, hilar or lung metastasis)
- CT scan (to detect retroperitoneal lymph nodes metastasis in patients diagnosed with testicular cancer)
Serum labs
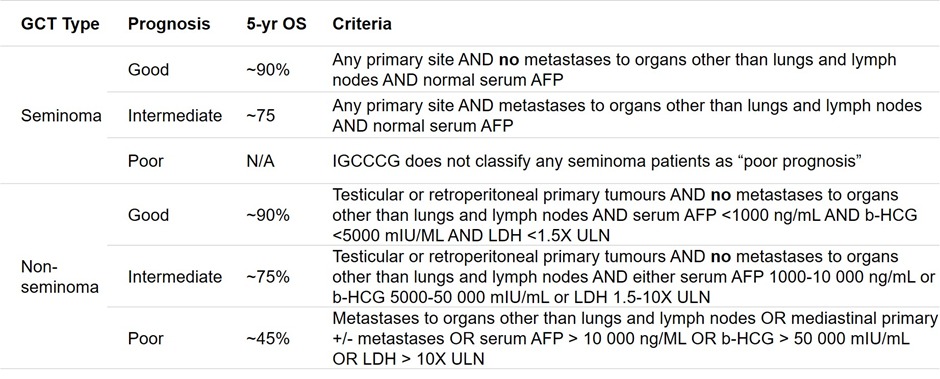
- Serum markers including; AFP, hCG, lactate dehydrogenase (LDH)
Seminoma Yolk sac Choriocarcinoma Teratoma Embryonal PLAP ↑ — — — — AFP — ↑↑ — —/↑ —/↑ (when mixed) B-hCG —/↑ —/↑ ↑↑ — ↑
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Differential diagnosis
- Orchitis
- Epididymitis
- Varicoceles
- Hydroceles
- Indirect inguinal hernias
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Complications
- Infertility
- Metastasis
- Endocrine abnormalities
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
Supplementary tables
- Table 1: epidemiology, manifestations, diagnosis and treatment of testicular cancer
Testicular cancer Epidemiology - Age 15 - 35 years
- Risk factors: family history, cryptorchidism
Manifestations - Unilateral, painless testicular nodule or swelling
- Dull lower abdominal ache
- Metastatic symptoms (eg, dyspnea, neck mass, low back pain)
Diagnosis - Examination: firm, ovoid mass or unilateral swelling
- Scrotal ultrasound
- Tumor markers (alpha fetoprotein, beta-HCG)
Treatment - Radical orchiectomy
- Chemotherapy
- Cure rate (95%)
- Table 2: malignant testicular neoplasms types and main details
Malignant testicular neoplasms Germ cell (95 %)
Seminoma - Retain features of spermatogenesis
- beta-HCG, AFP usually negative
Nonseminoma - >1 partially differentiated cells: yolk sac, embryonal carcinoma, teratoma, and/or choriocarcinoma
- beta-HCG, AFP usually positive
Stromal (5%)
Leydig - Often produces excessive estrogen (gynecomastia) or testosterone (acne)
- Can cause precocious puberty
Sertoli - Rare
- Occasionally associated with excessive estrogen secretions (gynecomastia)
سجل دخولك لإضافة ملاحظات خاصة لكل قسم
· اشترك الآن
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.
فيديوهات الشرح
بطاقات تفاعلية
أسئلة ممارسة
اشترك الآن