Summary
Bowel obstruction is the partial or complete blockage of intestinal lumen impeding passage of contents. Primary causes include adhesions (60-80%) for small bowel obstruction (SBO) and colorectal cancer (50-60%) for large bowel obstruction (LBO).
Clinical features vary by location: SBO presents with colicky periumbilical pain and early bilious vomiting, while LBO shows early pronounced distention with later vomiting. Signs include abdominal distention, tenderness, and altered bowel sounds.
Diagnosis relies on imaging (CT abdomen/pelvis is gold standard) showing dilated proximal bowel, collapsed distal bowel, and multiple air-fluid levels. Laboratory tests assess severity and complications.
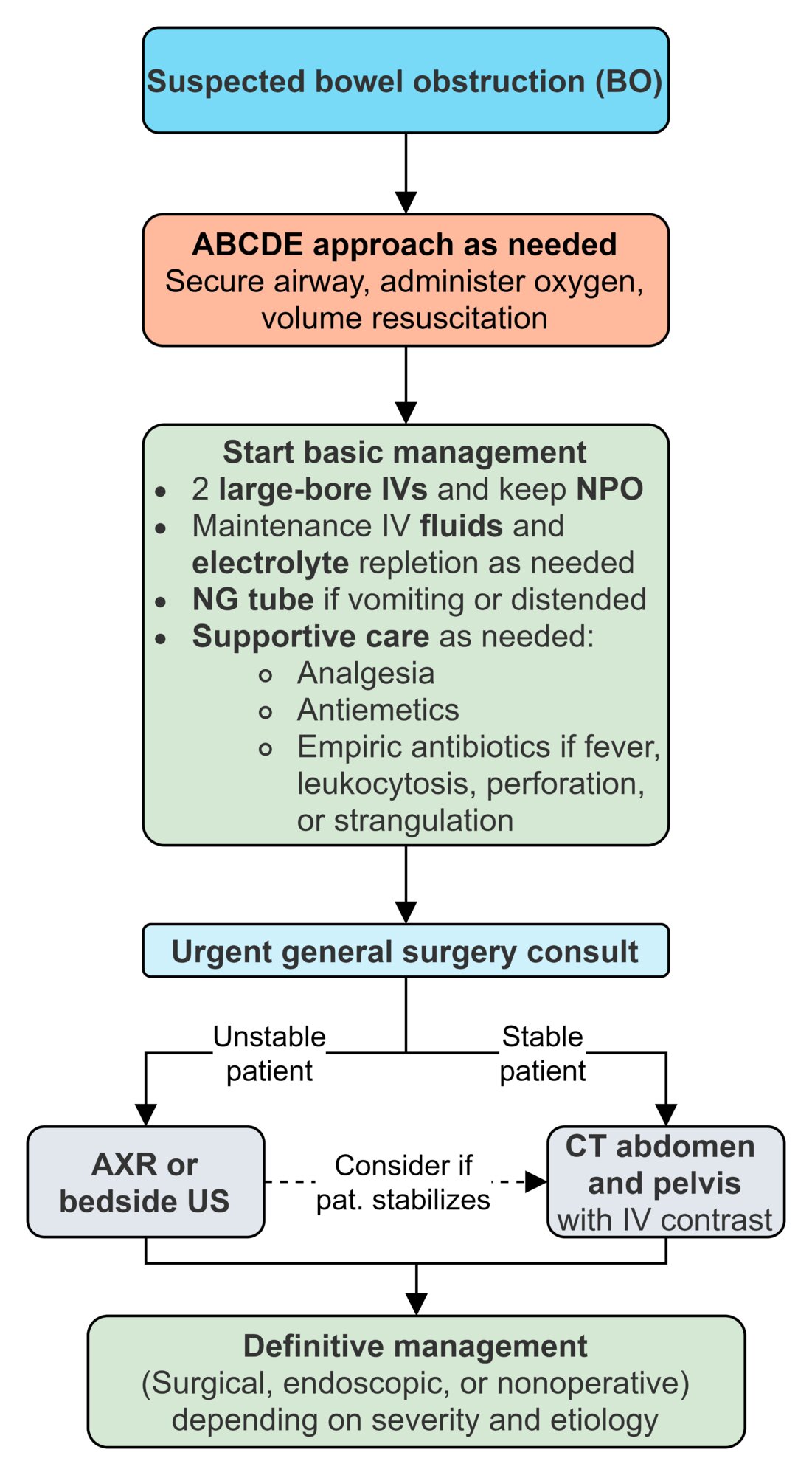
Management includes supportive care (IV fluids, nasogastric decompression) with nonoperative approach for simple obstructions. Surgical intervention is indicated for complicated cases (showing strangulation, ischemia), closed-loop obstructions, or when conservative management fails after 72 hours. Complications include bowel ischemia, perforation, and peritonitis.
Definition
Bowel obstruction refers to the partial or complete blockage of the intestinal lumen that impairs the normal passage of intestinal contents. It is categorized based on:
- Location: Small bowel obstruction (SBO) vs. large bowel obstruction (LBO)
- Physiologic mechanism: Mechanical vs. functional (paralytic ileus)
- Degree: Partial vs. complete
- Etiology: Intrinsic, intramural, extrinsic, or intraluminal causes
Epidemiology
- SBO primary cause: Adhesions (60-80% of cases)
- LBO primary cause: Colorectal cancer (50-60% of cases) in adults
- Age distribution: Varies by etiology (see specific causes)
Etiology
Classification by location and mechanism
| Classification by location and mechanism | |
|---|---|
| Classification | Description |
| Dynamic (mechanical) |
|
| Adynamic (paralytic/neurogenic ileum) |
|
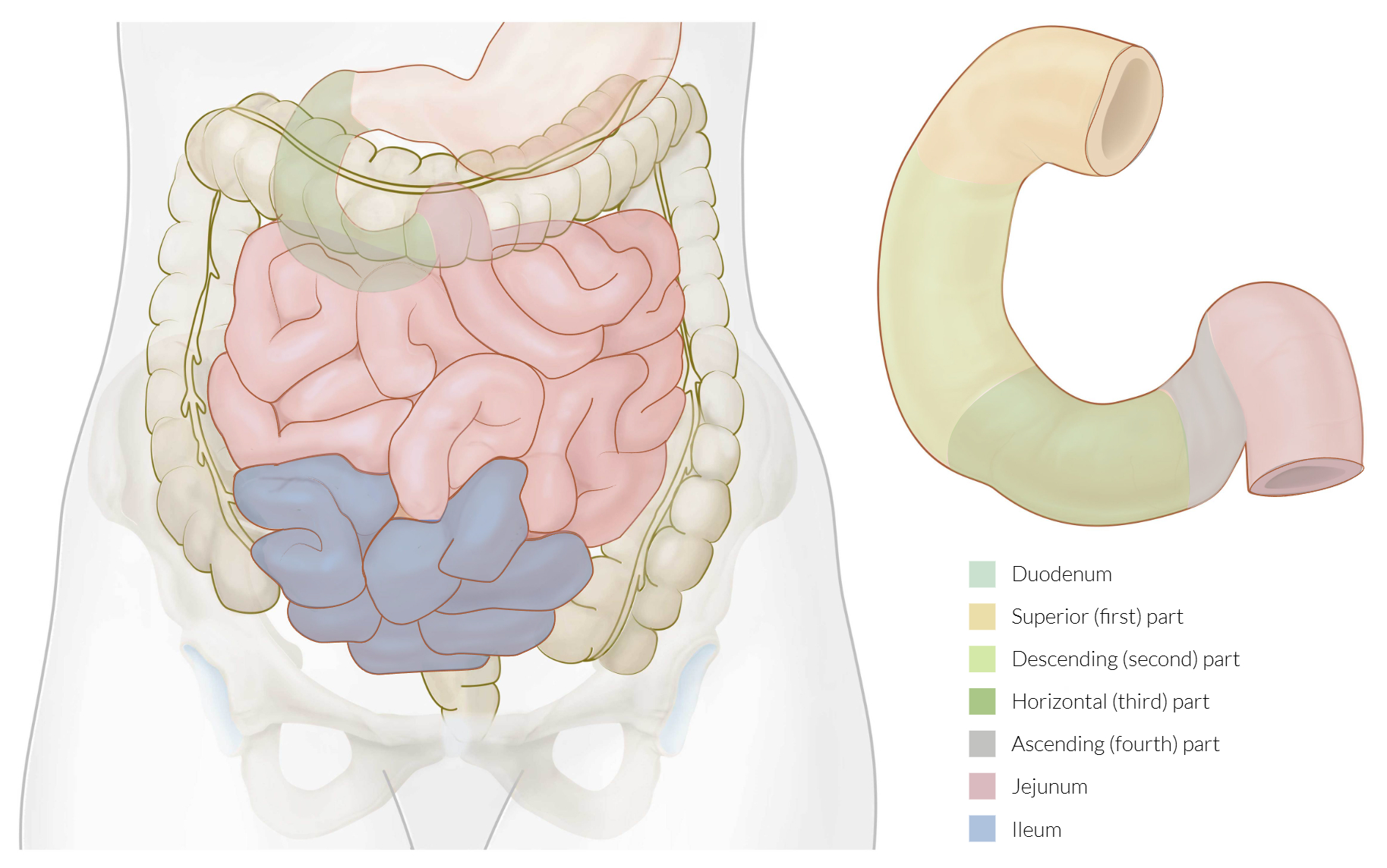
Classification by location of obstruction
| Classification by location of obstruction | |
|---|---|
| Location | Common Causes |
| Inside the lumen | Fecal impaction, gallstone ileus, foreign bodies, intussusceptions, parasites (Ascaris lumbricoides) |
| In the wall | Tumors, strictures (Crohn's disease), congenital atresia, diverticulitis |
| Outside the wall | Adhesions, strangulated hernias, volvulus, bands, masses |
Most common causes by age group
| Common Causes of Intestinal Obstruction by Age Group | |
|---|---|
| Age Group | Common Causes |
| Neonatal | Congenital anomalies, meconium ileus, Hirschsprung's disease |
| Infants | Intussusception, Hirschsprung's disease, obstruction due to meckel’s diverticulum, strangulated hernia |
| Young adults | Strangulated hernia, Crohn's disease, bands, adhesions |
| Adults & Elderly | Cancer, sigmoid volvulus, diverticulitis, strangulated hernias |
Small bowel obstruction (SBO)
- Post-surgical adhesions: 60-80% of cases
- Risk increases with number of previous abdominal surgeries
- May occur weeks to decades after surgery
- Hernias: 10-15% of cases (inguinal, femoral, umbilical, incisional)
- Neoplasms: 5-10% of cases (primary or metastatic)
- Crohn's disease: Strictures or inflammatory masses
- Intussusception: More common in children (90%) than adults
- Gallstone ileus: More common in elderly women
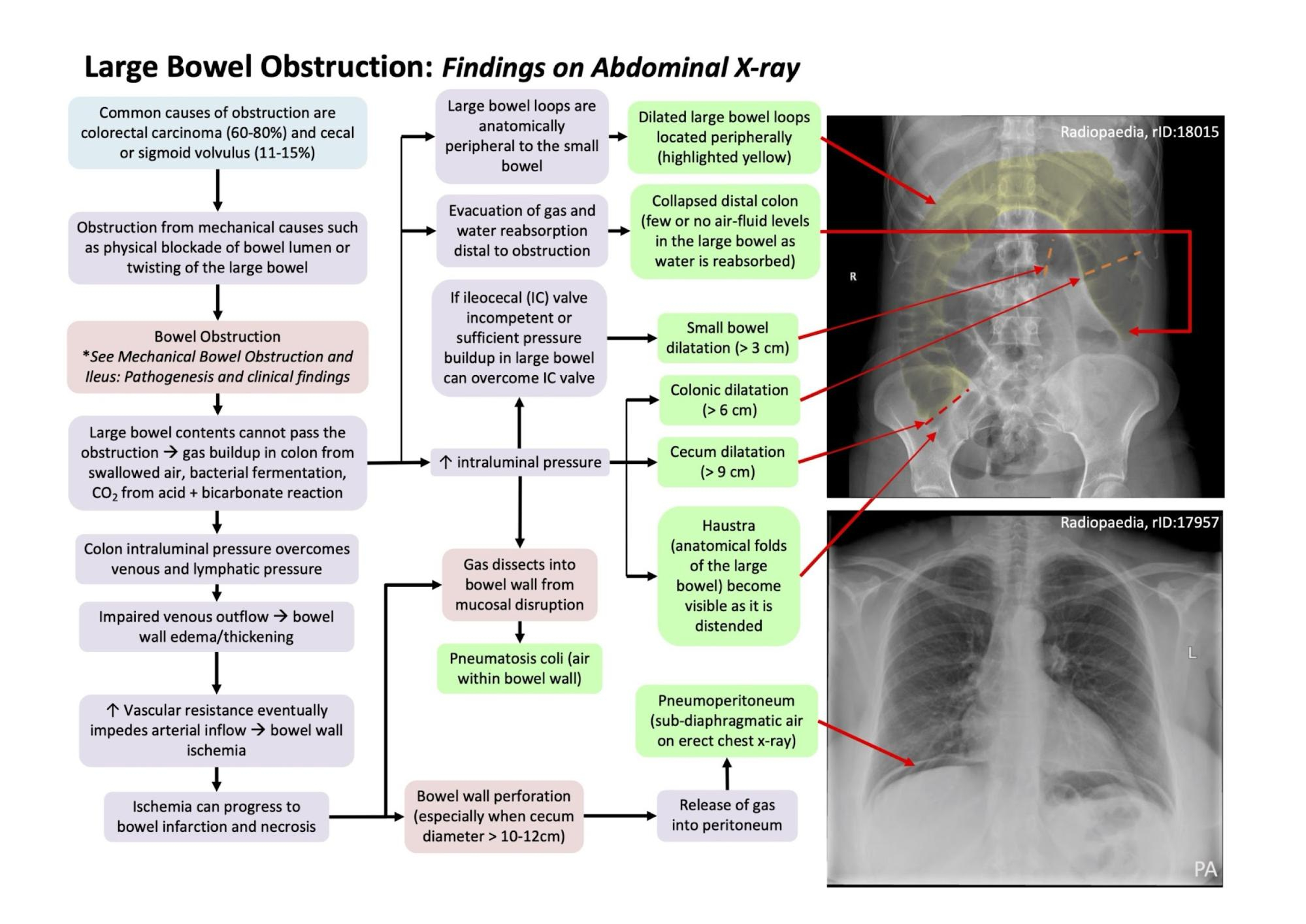
Large bowel obstruction (LBO)
- Colorectal cancer: 50-60% of cases
- Most commonly in sigmoid colon and rectum
- Diverticular disease: 10-20% of cases
- Volvulus: 10-15% of cases
- Sigmoid volvulus: More common in elderly, chronic constipation
- Cecal volvulus: More common in younger patients
- Strictures: Post-inflammatory, radiation-induced, ischemic
Clinical presentation
General clinical presentation of intestinal obstruction
- Abdominal pain
- Distension
- Vomiting
- Absolute constipation
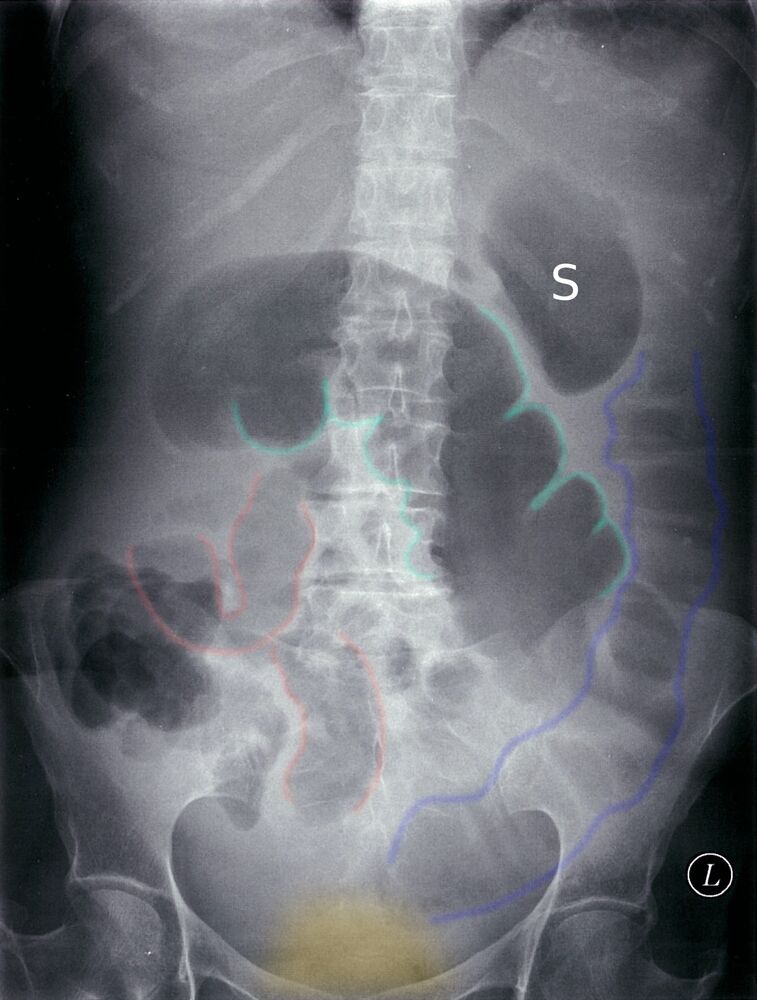
Clinical presentation according to the site
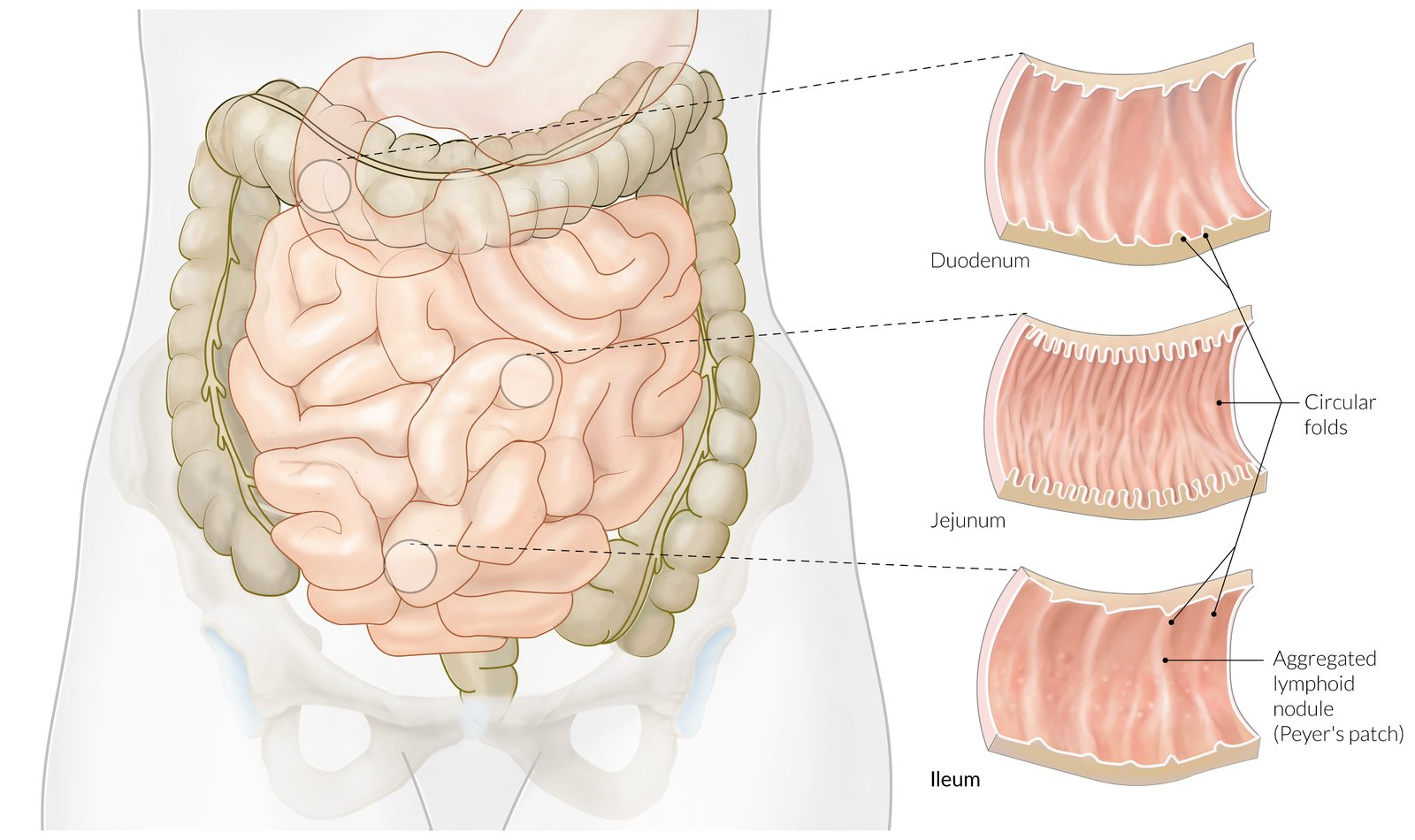
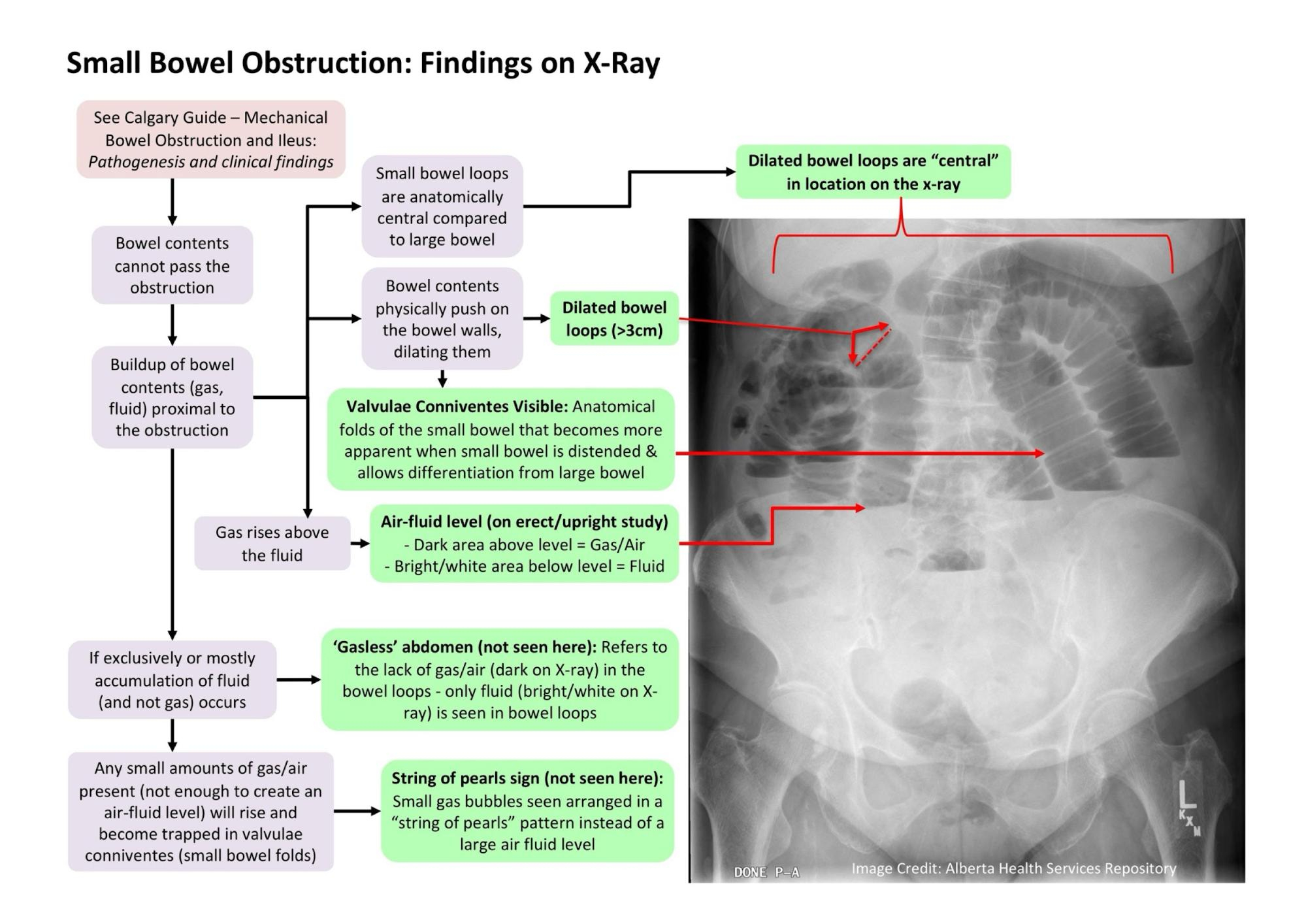
High small bowel obstruction
- Periumbilical pain
- Early profuse vomiting with rapid dehydration
- Minimal distension
- No air fluid levels on abdominal X-ray
Low small bowel obstruction
- Periumbilical pain
- Delayed vomiting
- Central distension multiple central air fluid level
Large bowel obstruction
- Distension is early and pronounced
- Pain is mild
- Vomiting and hydration are late
- Distended proximal colon and cecum on abdominal X-ray
Physical examination
- Signs of dehydration
- Visible peristalsis might be present
- Scars might suggest adhesions and hernias might suggest strangulation
- Abdominal distension and tenderness might be present
Small bowel obstruction (SBO)
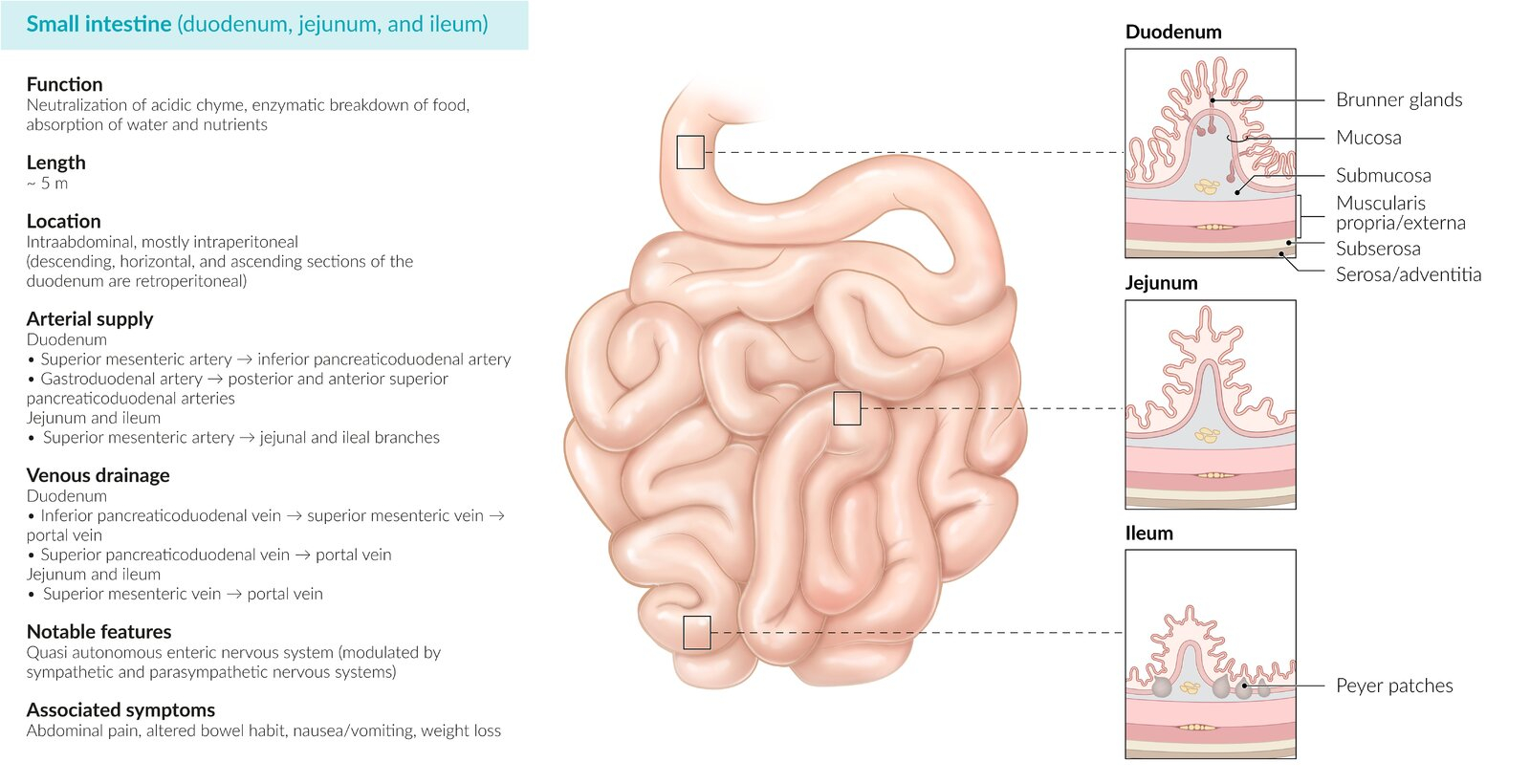
Background
- Small bowel obstruction (SBO) indicates partial or complete blockage of the small intestines
- Risk factors include prior abdominal surgery (most common cause, masses/malignancy (common in elderly), hernias, inflammatory bowel disease, and intussusception (in children)
Clinical presentation
- Symptoms
- Nausea and vomiting
- Abdominal pain
- Physical signs
- Abdominal distention
- Generalized tenderness
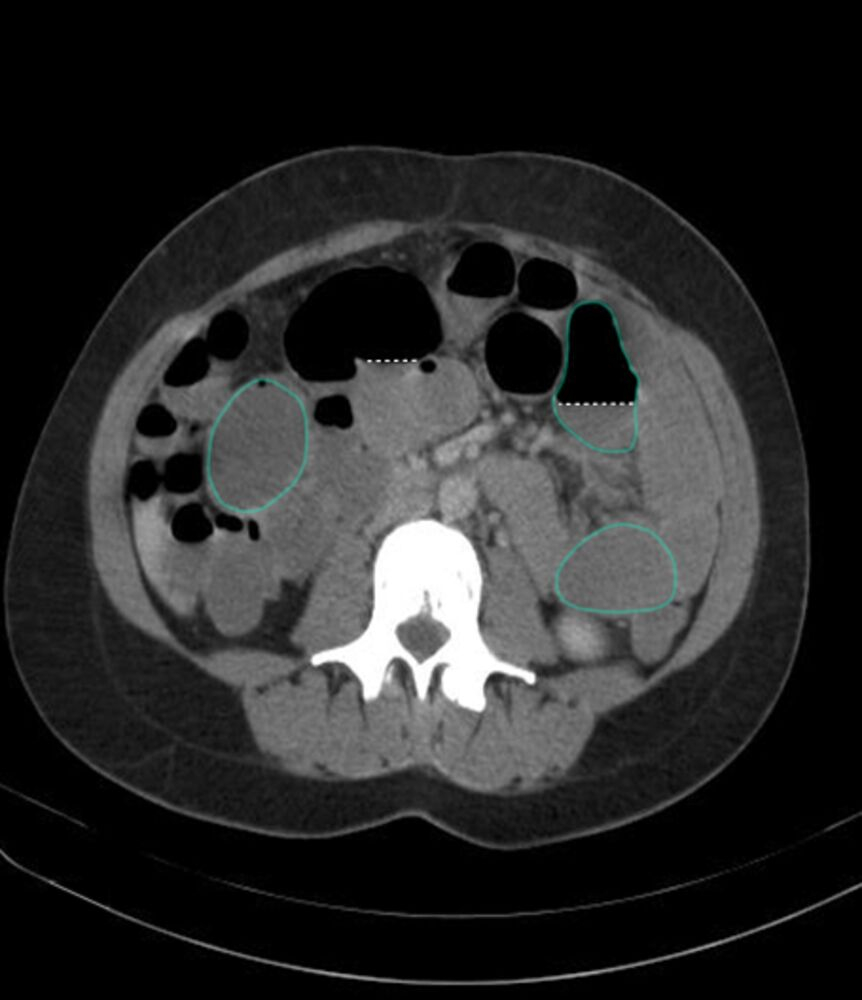
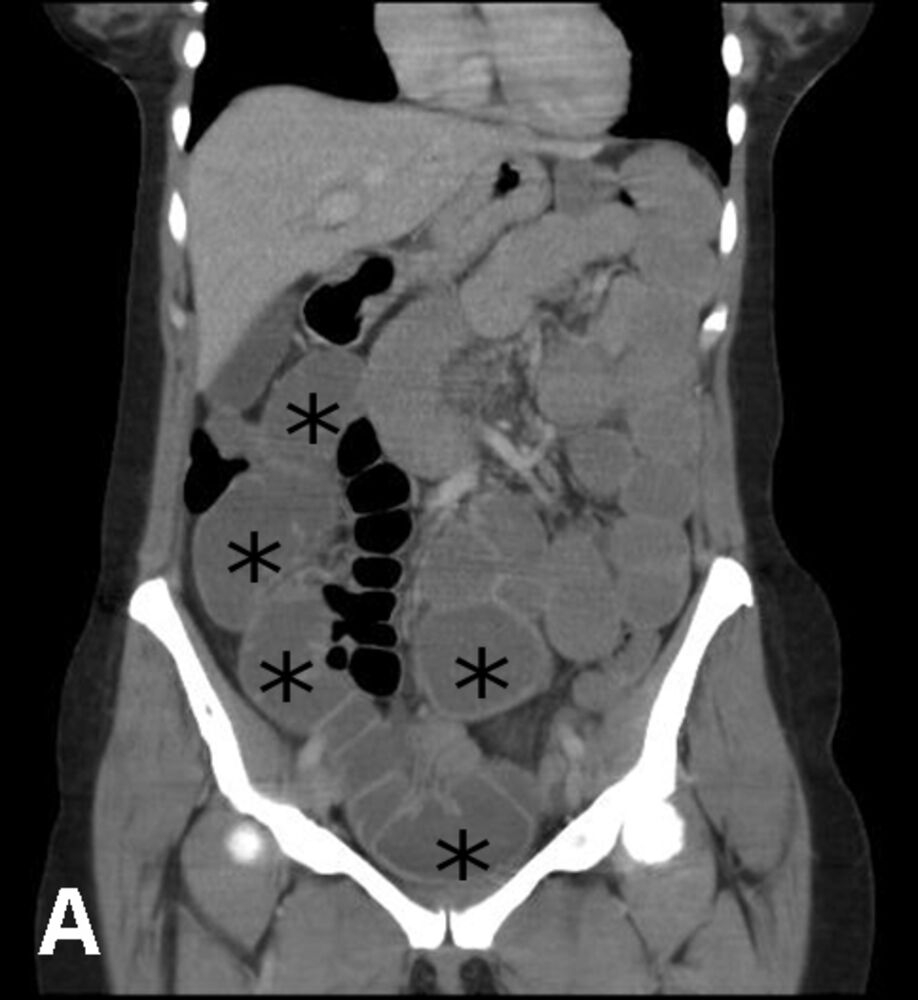
Diagnosis
- Labs
- Lactic acid (to monitor for bowel necrosis)
- Imaging
- Abdominal X-ray (best initial test) that would show dilated loops of small bowel
- CT scan of the abdomen and pelvis would show dilated loops of small bowel and any masses present


Differential diagnosis
- Acute appendicitis (imaging would reveal an enlarged appendix with signs of inflammation instead of dilated loops of bowel)
Treatment
- Conservative management
- IV fluids
- Medical management
- Treat the underlying condition
- Nasogastric decompression and bowel rest (indicated for partial SBO with no signs of bowel strangulation)
- Surgical management
- Should be performed to relieve the obstruction and correct the cause of SBO (eg, removal of adhesions and bands)
- Surgical management is indicated for peritonitis and signs of bowel strangulation (systemic signs, metabolic acidosis and continuous pain)
Complications
- bowel necrosis
- peritonitis
- bowel perforation
Prognosis
- Partial SBO is often self resolving
- Complete SCO may be self resolving but often may require surgical intervention
Mind maps
| Small Bowel Obstruction - Summary | |
| Clinical Presentation |
|
| Diagnosis |
|
| Complications |
|
| Management |
|
Large bowel obstruction (LBO)
Background
- Large bowel obstruction (LBO) is a surgical emergency and requires intervention (obstruction may be partial or complete)
- LBO is commonly seen in elderly patients
- Chronic constipation is a major risk factor
Clinical presentation
- Symptoms
- Cramps abdominal pain
- Nausea and vomiting
- Bloating
- Physical signs
- Abdominal distention
- Generalized tenderness
Diagnosis
- Labs
- Lactic acid (to monitor for bowel necrosis)
- Imaging
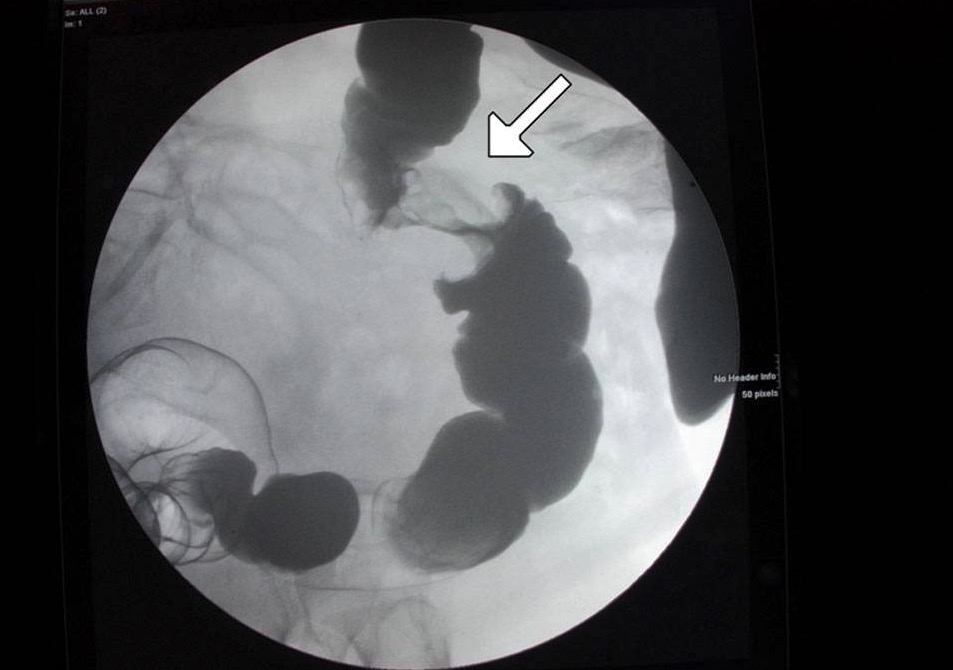
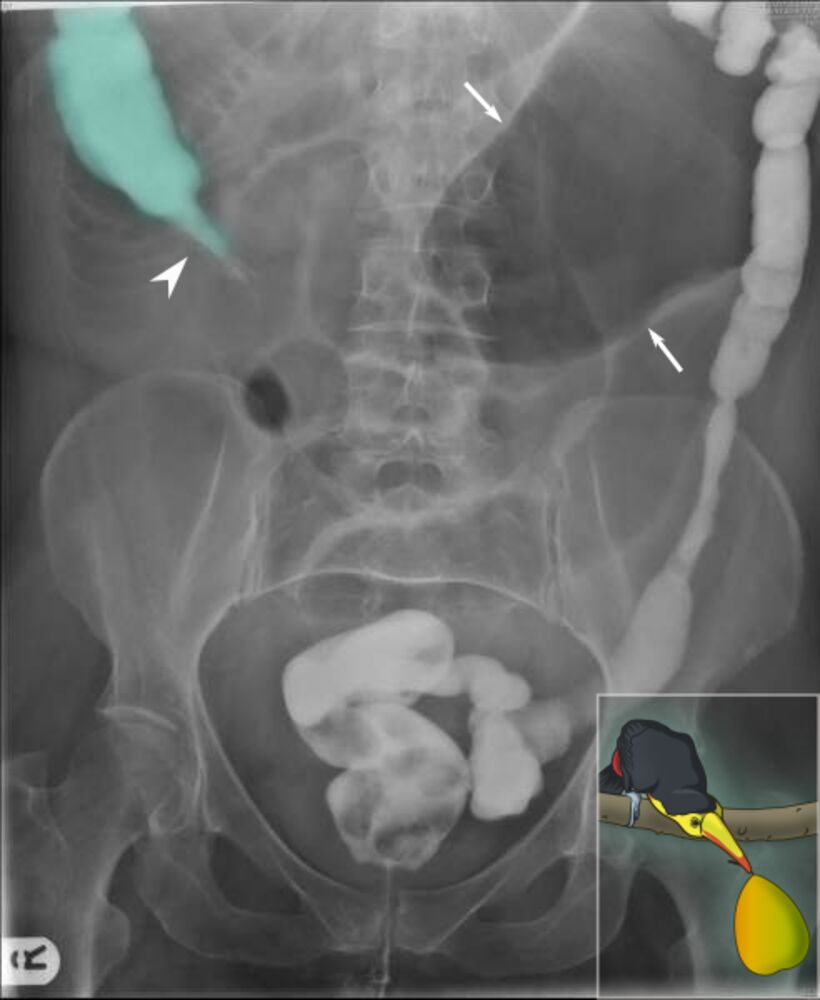
- Abdominal X-ray (best initial test) that would show dilated bowel (screen for free air under the diaphragm)
- CT scan of the abdomen and pelvis with contrast (imaging of choice for diagnosis of LBO) to distinguish between a partial or complete obstruction
- Contrast radiography with enema (bird’s beak appearance in volvulus, Apple core sign in colonic malignancy)




Differential diagnosis
- Small bowel obstruction (dilated loops of small bowel seen on imaging rather than dilated loops of large bowel)
- Ogilvie syndrome (no mechanical lesion on CT imaging)
Treatment
- Conservative management
- Modified diet (high fiber diet, stool softeners)
- Medical management
- IV fluids
- Nasogastric decompression and bowel rest (indicated for cases with abdominal distention or vomiting)
- Surgical management
- Exploratory laparotomy (indicated for complete LBO, bowel ischemia, or volvulus)
Complications
- Ischemic colitis
- Bowel perforation
Prognosis
- If treated early, mortality for LBO is low
- If there is bowel ischemia or perforation, mortality is higher Mind maps
Mind maps
Acute Colonic Pseudo-Obstruction (Ogilvie Syndrome)
| Acute Colonic Pseudo-Obstruction (Ogilvie Syndrome) | |
| Etiologies |
|
| Clinical Findings |
|
| Imaging |
|
| Management |
|
Sigmoid volvulus
| Sigmoid Volvulus | |
| Risk Factors |
|
| Clinical Presentation |
|
| Imaging |
|
| Management |
|
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.