Summary
Primary biliary cholangitis (PBC), formerly known as primary biliary cirrhosis, is a chronic autoimmune liver disease characterized by progressive destruction of small intrahepatic bile ducts. The disease predominantly affects middle-aged women (40-60 years) with a female to male ratio of 9:1. The hallmark of PBC is the presence of anti-mitochondrial antibodies (AMA), which are positive in approximately 95% of cases. Patients typically present with an insidious onset of fatigue and pruritus, though many are diagnosed incidentally through abnormal liver function tests showing a cholestatic pattern. The diagnosis requires 2 of 3 criteria: elevated alkaline phosphatase, positive AMA, and characteristic histological findings. First-line treatment is ursodeoxycholic acid (UDCA), which slows disease progression when started early. Without treatment, the disease progresses through stages from portal inflammation to cirrhosis over 15-20 years.
Overview
- Definition: Chronic autoimmune destruction of small intrahepatic bile ducts leading to cholestasis
- Demographics:
- 90% of patients are women
- Typical age at diagnosis: 40-60 years
- More common in Northern Europeans
- Prevalence: 40-400 cases per million
- Natural history: Slow progression over 15-20 years from asymptomatic disease to cirrhosis if untreated
- Prognosis: Excellent with early treatment; patients responding to UDCA have near-normal life expectancy
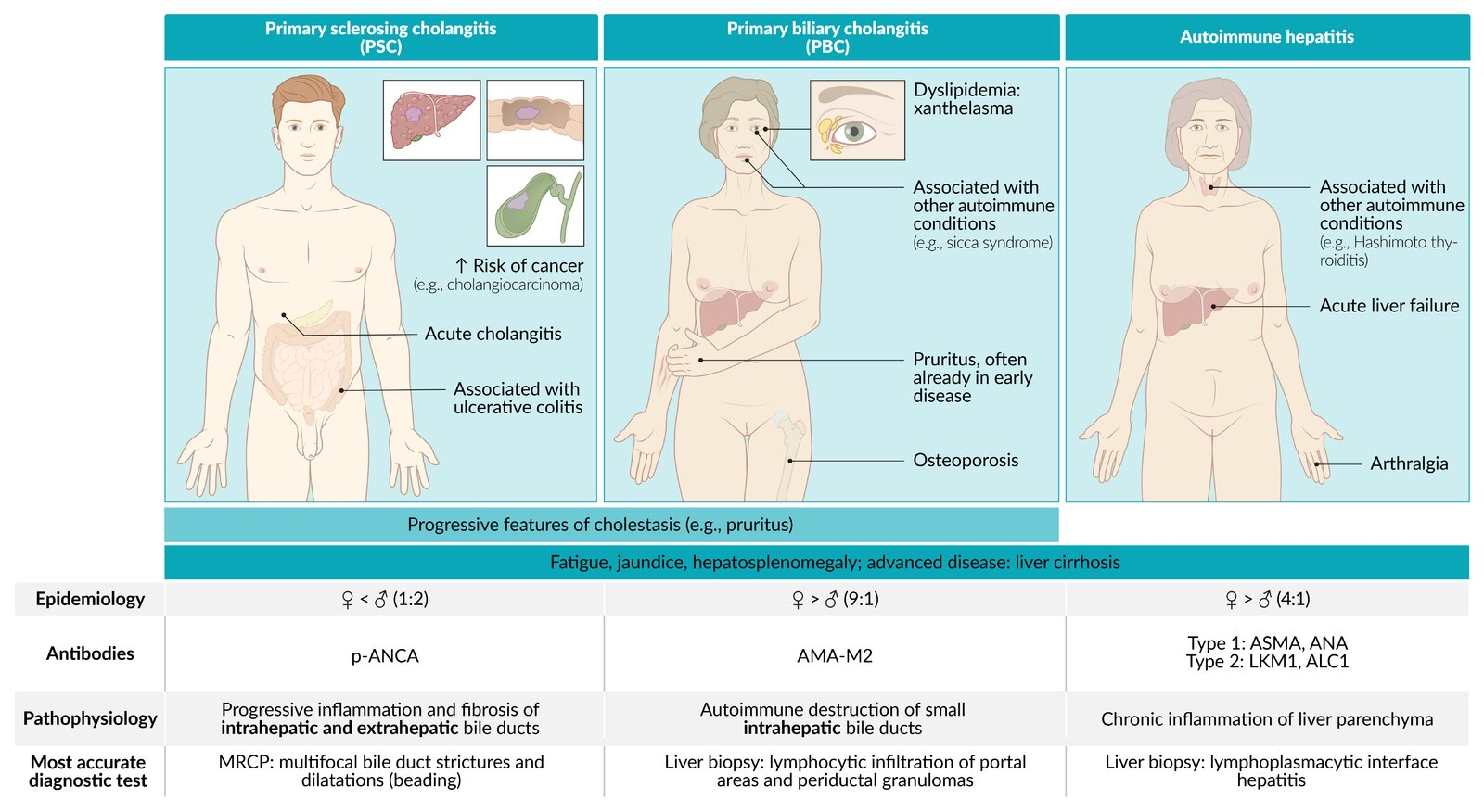
Epidemiology
- Age: Peak incidence 40-60 years (mean age ~55 years)
- Sex: Female >> Male (9:1 ratio)
- Geography: More common in Northern Europe and North America
- Prevalence: 19-402 cases per million population
- Risk factors:
- Family history of PBC (increased risk in first-degree relatives)
- Presence of other autoimmune diseases
- Environmental factors (smoking, nail polish use, hair dye - controversial)
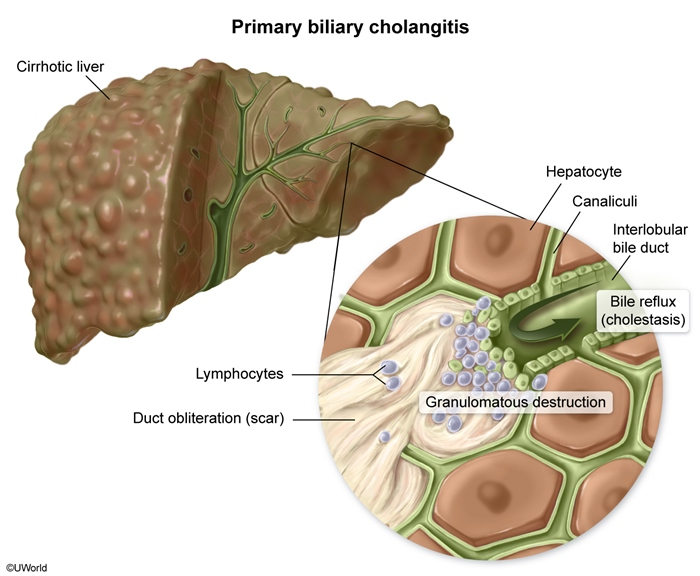
Pathophysiology
- Autoimmune mechanism:
- T-cell mediated destruction of cholangiocytes (bile duct epithelial cells)
- Target antigen: M2 subtype of mitochondrial pyruvate dehydrogenase complex (PDC-E2)
- Environmental trigger in genetically susceptible individuals
- Histological progression:
- Stage 1: Portal inflammation with florid duct lesions (granulomas around bile ducts)
- Stage 2: Periportal inflammation and fibrosis
- Stage 3: Bridging fibrosis
- Stage 4: Cirrhosis
- Consequences of bile duct destruction:
- Cholestasis → accumulation of bile acids
- Reduced bile flow → malabsorption of fat-soluble vitamins (A, D, E, K)
- Progressive fibrosis → cirrhosis and portal hypertension
Clinical Features
- Early symptoms (may be absent in 50-60% at diagnosis):
- Fatigue (65%): Most common symptom, often profound and disproportionate to disease severity
- Pruritus (55%):
- Worse at night
- Often affects palms and soles first
- Due to bile acid accumulation
- May precede diagnosis by years
- Physical examination findings:
- Hepatomegaly: Smooth, non-tender liver enlargement
- Xanthelasma and xanthomas: Due to severe hypercholesterolemia
- Skin hyperpigmentation: Related to melanin deposition
- Excoriations: From scratching due to pruritus
- Late features (advanced disease):
- Jaundice (indicates poor prognosis)
- Portal hypertension: splenomegaly, varices, ascites
- Bone pain from osteoporosis
| Important – فكرة سؤال | |
|
Classic presentation: Middle-aged woman with fatigue + pruritus + elevated alkaline phosphatase = Think PBC! تذكر: الحكة قد تسبق التشخيص بسنوات وتكون أسوأ في الليل |
تذكر |
Associated Conditions
PBC frequently occurs with other autoimmune disorders (up to 84% of patients):
- Sjögren's syndrome (50-60%): Dry eyes and dry mouth
- Autoimmune thyroid disease (20%): Usually hypothyroidism
- Raynaud's phenomenon (15%)
- Scleroderma/CREST syndrome (10%)
- Rheumatoid arthritis (10%)
- Celiac disease (6%)
Laboratory Findings
- Liver biochemistry (cholestatic pattern):
- ↑↑ Alkaline phosphatase (ALP): 2-10× normal
- ↑ Gamma-GT (GGT): Confirms hepatic origin of ALP
- Normal or mildly ↑ aminotransferases (ALT, AST)
- Bilirubin: Normal early, elevated in advanced disease
- Immunological markers:
- Anti-mitochondrial antibodies (AMA):
- Positive in 95% of cases
- Highly specific (98%)
- M2 subtype most specific
- Elevated IgM levels
- ANA positive in 30% (may indicate overlap syndrome)
- Anti-mitochondrial antibodies (AMA):
- Lipid profile:
- Marked hypercholesterolemia (total cholesterol may exceed 500 mg/dL)
- Predominantly HDL elevation (not atherogenic)
Diagnosis
Diagnostic Criteria - Need 2 of 3:
- Elevated ALP (≥1.5x upper limit of normal) for >6 months
- Positive AMA
- Liver biopsy showing characteristic histology (rarely needed)
Diagnostic Approach:
- Step 1: Confirm cholestatic pattern on liver tests
- Step 2: Rule out extrahepatic obstruction
- Ultrasound abdomen - normal bile ducts in PBC
- MRCP if PSC suspected
- Step 3: Check AMA
- If positive → diagnosis confirmed
- If negative → check PBC-specific ANA
- Step 4: Liver biopsy (only if AMA negative and high suspicion)
| Important – فكرة سؤال | |
| AMA is the MOST SENSITIVE and SPECIFIC test for PBC. If a patient has cholestatic LFTs + positive AMA = PBC diagnosis confirmed! | تذكر |
| Note | |
| Liver biopsy is NOT required for diagnosis if AMA positive + cholestatic liver tests. Biopsy is mainly for staging or when diagnosis is uncertain (AMA-negative PBC in 5% of cases). | ملاحظة |
Differential Diagnosis
| Autoimmune Liver Disease | |||
|---|---|---|---|
| Autoimmune Hepatitis |
Primary Biliary Cholangitis (PBC) |
Primary Sclerosing Cholangitis (PSC) |
|
| Epidemiology |
|
|
|
| Associations |
|
|
|
| Liver Injury Pattern |
|
|
|
| Antibodies |
|
|
|
| Histology |
|
|
|
|
* Antinuclear and p-ANCA are nonspecific. IBD = inflammatory bowel disease; UC = ulcerative colitis; p-ANCA = perinuclear anti-neutrophil cytoplasmic antibodies |
|||
Management
First-line therapy:
- Ursodeoxycholic acid (UDCA) 13-15 mg/kg/day:
- Mechanism: Replaces toxic hydrophobic bile acids with hydrophilic UDCA
- Benefits: Improves liver biochemistry, delays progression, may improve survival
- Response assessment at 12 months (Paris criteria)
- Continue indefinitely, even in asymptomatic patients
Second-line therapy (for UDCA non-responders ~40%):
- Obeticholic acid (5-10 mg/day): FXR agonist, add to or replace UDCA
- Fibrates (bezafibrate, fenofibrate): Off-label use
Symptomatic treatment:
- For pruritus:
- First-line: Cholestyramine 4-16 g/day
- Second-line: Rifampicin 150-300 mg/day
- Third-line: Naltrexone, sertraline
- For fatigue: Modafinil (limited evidence)
- For osteoporosis: Calcium + Vitamin D, bisphosphonates
Liver transplantation:
- Indications: Decompensated cirrhosis, intractable pruritus, recurrent variceal bleeding
- Excellent outcomes: 5-year survival >80%
- Disease recurs in 20-30% post-transplant
| Important – فكرة سؤال | |
| Remember: UDCA should be started immediately upon diagnosis, even in asymptomatic patients, as it's most effective in early disease!
يجب البدء بعلاج UDCA فور التشخيص حتى لو كان المريض بدون أعراض |
تذكر |
Monitoring
- Liver function tests: Every 3-6 months
- Assessment of UDCA response: At 12 months (Paris criteria)
- Screening for complications:
- Bone density (DEXA): Baseline and every 2-3 years
- Fat-soluble vitamins: Annual measurement
- Thyroid function: Annual TSH
- Hepatocellular carcinoma: Ultrasound every 6 months if cirrhotic
- Varices: Endoscopy if cirrhotic
Complications
- Metabolic complications:
- Osteoporosis/osteomalacia (30%): Due to vitamin D deficiency and cholestasis
- Fat-soluble vitamin deficiencies (A, D, E, K)
- Steatorrhea and malabsorption
- Portal hypertension complications:
- Esophageal varices
- Ascites
- Hepatic encephalopathy
- Hepatocellular carcinoma: Increased risk (3-5%) in cirrhotic patients
- Hyperlipidemia: Usually not atherogenic due to HDL predominance
Quick Review Table
| Primary Biliary Cholangitis (PBC) | |
|---|---|
| Pathophysiology |
|
| Clinical Features |
|
| Diagnosis |
|
| Treatment |
|
| Complications |
|
| AMA = anti-mitochondrial antibodies; PDC = pyruvate dehydrogenase complex; UDCA = ursodeoxycholic acid | |
High-Yield Exam Points
| Must-Know Points for Exams |
|
1. Classic presentation: Middle-aged woman with fatigue + pruritus + ↑ALP 2. AMA is the key diagnostic test - 95% sensitivity and specificity 3. PBC vs PSC distinction: 4. UDCA is first-line treatment - slows progression but doesn't help symptoms 5. Cholestyramine for pruritus - give 4 hours apart from UDCA 6. Complications to remember: Osteoporosis (not osteomalacia primarily) 7. Hypercholesterolemia does NOT increase CV risk (HDL mainly elevated) 8. Jaundice = late finding = poor prognosis |
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.