Summary
Viral hepatitis is a significant global health burden caused by five main hepatotropic viruses (A-E). Hepatitis A virus (HAV) and hepatitis E virus (HEV) are transmitted via the fecal-oral route and typically cause acute, self-limited infections. Hepatitis B virus (HBV) and hepatitis C virus (HCV) are blood-borne pathogens that can lead to chronic infection, cirrhosis, and hepatocellular carcinoma. Hepatitis D virus (HDV) is a defective virus requiring HBV for replication. Understanding the epidemiology, transmission, clinical features, and management of each type is essential for medical practice. Prevention through vaccination (available for HAV and HBV) and safe practices remains the cornerstone of controlling viral hepatitis.
Introduction
- Viral hepatitis refers to liver inflammation caused by hepatotropic viruses
- Five main types: A, B, C, D, and E
- Classification based on transmission:
- Fecal-oral route: HAV and HEV → typically acute infections
- Parenteral/blood-borne: HBV, HCV, and HDV → can cause chronic infections
- Major cause of morbidity and mortality worldwide
| Important – فكرة سؤال | |
|
Remember the transmission routes: HAV and HEV = fecal-oral. HBV, HCV, HDV = blood-borne |
تذكر |
Hepatitis A
Epidemiology and Transmission
- Causative agent: HAV (Picornaviridae family), nonenveloped single-stranded RNA virus
- Transmission: Fecal-oral route
- Contaminated food and water (especially undercooked shellfish)
- Person-to-person spread in crowded conditions
- Daycare centers, homeless shelters
- High-risk groups:
- International travelers to endemic areas
- Men who have sex with men (MSM)
- Injection drug users
- People in crowded living conditions
- Geographic distribution: Higher incidence in developing countries with poor sanitation
Pathogenesis
- Virus ingested → crosses intestinal epithelium → reaches liver via portal circulation
- Replicates in hepatocytes and Kupffer cells without direct cytopathic effects
- Liver injury is immune-mediated (cytotoxic T cells targeting infected hepatocytes)
- Virus excreted in bile and shed in feces
- Peak infectivity: Before symptom onset ➜ مهم
Clinical Presentation
- Incubation period: 2-6 weeks (average 4 weeks)
- Children <6 years: Often asymptomatic
- Adults: Symptomatic in ~70%
- Prodromal phase: Fever, malaise, anorexia, nausea
- Icteric phase: Jaundice, dark urine, pale stools
- Right upper quadrant pain (hepatomegaly)
- Duration: Self-limited, recovery within 3-6 weeks
Diagnosis
- Laboratory findings:
- ↑ ALT and AST (often >10× upper limit of normal)
- ↑ Bilirubin and alkaline phosphatase
- Serology ➜ Most important for diagnosis
- Anti-HAV IgM: Acute infection
- Anti-HAV IgG: Past infection or immunity
Complications
- Fulminant hepatitis (<1%): More common in elderly, pregnancy, chronic liver disease
- Cholestatic hepatitis: Prolonged jaundice and pruritus
- Relapsing hepatitis: Symptoms return after initial improvement
- NO chronic infection ➜ مهم جداً
Management
- Supportive care: Rest, hydration, avoid hepatotoxins
- No specific antiviral therapy available
- Hospitalization for severe cases (fulminant hepatitis)
Prevention
- Vaccination:
- All children at age 1 year
- Travelers to endemic areas
- High-risk individuals (MSM, chronic liver disease, drug users)
- Post-exposure prophylaxis (within 2 weeks):
- HAV vaccine: Preferred (long-term protection)
- Immunoglobulin: For immunocompromised or age <1 year
- Good hygiene and sanitation
Hepatitis B
Definition
- Acute HBV infection: Self-limited liver inflammation lasting <6 months
- Chronic HBV infection: Persistent infection with HBsAg positive for >6 months
- Caused by hepatitis B virus (HBV), a partially double-stranded DNA virus
- Can lead to cirrhosis and hepatocellular carcinoma (HCC)
Epidemiology
- Global burden:
- 2 billion people have been infected worldwide
- 250-400 million chronic carriers
- Endemic areas: Sub-Saharan Africa, East Asia, Pacific Islands
- Age at infection determines outcome ➜ Very important concept
- Neonates: 90% become chronic
- Children 1-5 years: 30% become chronic
- Adults: Only 5% become chronic
Transmission
- Vertical transmission (mother to child)
- Most common route in endemic areas
- Occurs during birth (not transplacental)
- 90% risk of chronicity
- Horizontal transmission
- Sexual contact (unprotected sex)
- Parenteral: IV drug use, needlestick, transfusions
- Household: sharing razors, toothbrushes
- NOT transmitted by: Casual contact, kissing, sharing food/water
| Important – فكرة سؤال | |
| In endemic areas → vertical transmission is most common In Western countries → sexual and IV drug use are most common |
تذكر |
Pathophysiology
- HBV enters hepatocytes via bile salt transporter receptor
- Viral DNA is repaired and transcribed
- Key point: Liver injury is immune-mediated, not from direct viral damage
- Cytotoxic T cells attack infected hepatocytes
- Explains why immunosuppressed patients have less liver damage
- HBV can integrate into host DNA → HCC risk even without cirrhosis ➜ مهم
Clinical Features
Acute HBV Infection
- Incubation: 1-4 months
- 70% are asymptomatic (subclinical)
- Symptomatic cases:
- Prodrome: Fatigue, malaise, anorexia, nausea
- Jaundice phase: Jaundice, dark urine, pale stools
- Right upper quadrant pain (hepatomegaly)
- Serum sickness-like syndrome: Fever, rash, arthralgia
- Lab findings:
- ALT and AST >10× normal (ALT > AST)
- Elevated bilirubin
- INR >1.5 = poor prognosis
- >95% of adults recover spontaneously
- <1% develop fulminant hepatitis
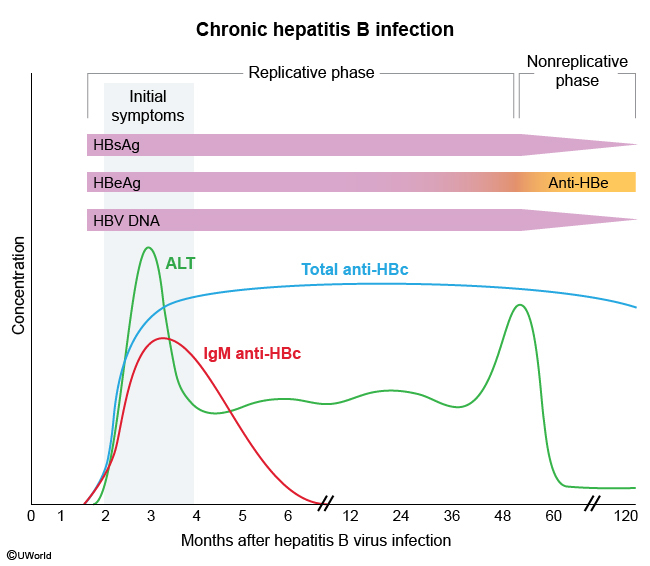
Chronic HBV Infection
- Usually asymptomatic until cirrhosis develops
- May have fatigue or extrahepatic manifestations
- Lab: ALT/AST may be normal or intermittently elevated
- 20-30% develop cirrhosis
- 2-3% annual HCC risk
Serologic Markers
| HBV Serologic Markers | ||
| Marker | What it means | Clinical significance |
| HBsAg | Surface antigen | • Current infection (acute or chronic) • First marker to appear • If >6 months = chronic |
| Anti-HBs | Surface antibody | • Immunity (recovery or vaccination) • Protective antibody |
| Anti-HBc IgM | Core antibody (IgM) | • Acute infection • Only marker in window period |
| Anti-HBc IgG | Core antibody (IgG) | • Past or chronic infection • NOT from vaccination • Persists for life |
| HBeAg | e antigen | • High infectivity • Active viral replication |
| Anti-HBe | e antibody | • Lower viral replication • Better prognosis |
| Important – فكرة سؤال | |
|
Window period: HBsAg disappeared but Anti-HBs not yet appeared فترة النافذة: اختفى HBsAg ولكن Anti-HBs لم يظهر بعد ← فقط Anti-HBc IgM إيجابي |
تذكر |
Natural History of Infection
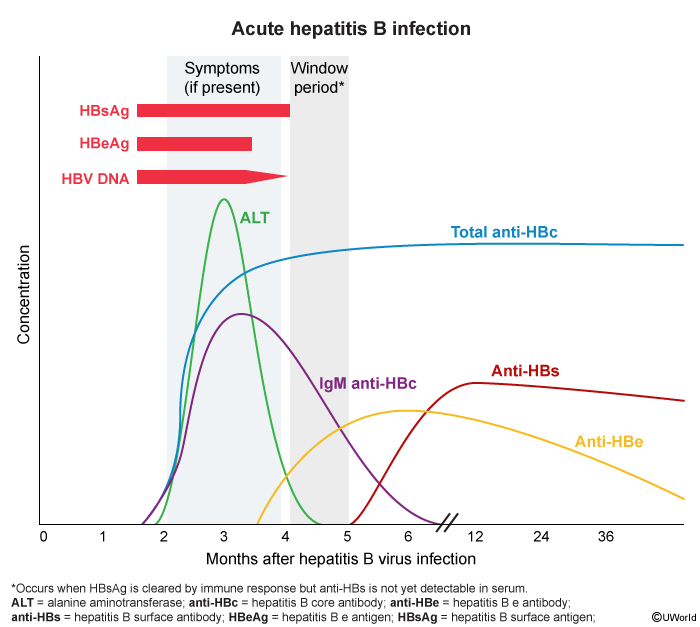
Acute HBV Timeline
- 0-4 months: HBsAg appears first, then HBeAg, HBV DNA
- 3-5 months: Symptoms appear, ALT rises, Anti-HBc IgM appears
- 3-6 months: Anti-HBe appears, HBeAg disappears
- 4-6 months: Window period (only Anti-HBc IgM positive)
- 6+ months: Anti-HBs appears = immunity
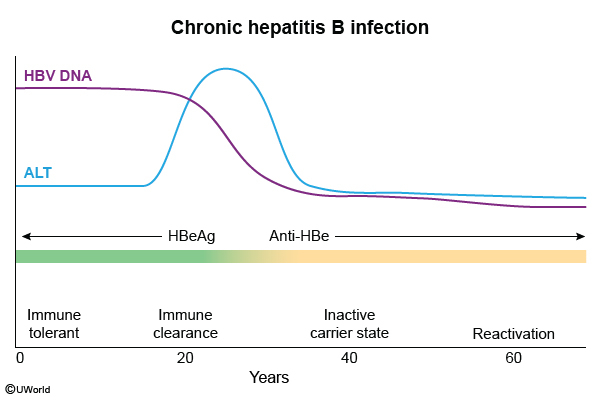
Chronic HBV Phases
- Phase 1 - Immune tolerant
- High HBV DNA + HBeAg positive
- Normal ALT (no inflammation)
- Common in vertical transmission
- Phase 2 - Immune active ➜ Highest risk for cirrhosis
- High HBV DNA + HBeAg positive
- Elevated ALT (active inflammation)
- Phase 3 - Inactive carrier
- Low HBV DNA + HBeAg negative/Anti-HBe positive
- Normal ALT
- Good prognosis
- Phase 4 - Reactivation
- Fluctuating HBV DNA and ALT
- HBeAg negative (escape mutants)
Diagnosis Summary
| Common HBV Scenarios | ||
| Scenario | Serologic Pattern | |
| Acute infection | HBsAg (+), Anti-HBc IgM (+), HBeAg (+) | |
| Window period | Only Anti-HBc IgM (+) | |
| Recovery/Immunity | Anti-HBs (+), Anti-HBc IgG (+) | |
| Vaccination | Only Anti-HBs (+) | |
| Chronic infection | HBsAg (+) for >6 months | |
Complications
- Hepatic complications
- Cirrhosis (20-30% of chronic cases)
- HCC (2-3% annually) - can occur WITHOUT cirrhosis
- Fulminant hepatitis (<1%)
- Extrahepatic complications
- Polyarteritis nodosa
- Membranous nephropathy
- Mixed cryoglobulinemia (rare)
Treatment
Acute HBV
- Usually supportive care only (>95% recover)
- Antivirals given only if:
- Symptoms >4 weeks + bilirubin >3 mg/dL
- INR >1.5
- Acute liver failure
Chronic HBV - Treatment Indications
- ALT >2× normal + high HBV DNA
- HBeAg positive: HBV DNA >20,000 IU/mL
- HBeAg negative: HBV DNA >2,000 IU/mL
- Cirrhosis (treat regardless of ALT or HBV DNA)
- Immunosuppression planned
- HCC
First-line Antivirals
- Entecavir: Potent, low resistance ➜ Preferred
- Tenofovir: Also treats HIV
- Lamivudine: High resistance, not preferred
Prevention
Vaccination
- Universal vaccination:
- All newborns within 24 hours
- If mother HBsAg (+): Give HBIG + vaccine within 12 hours
- High-risk groups: Healthcare workers, IV drug users, HIV patients
- Success = Anti-HBs ≥10 mIU/mL
Post-exposure Prophylaxis
- If exposed person vaccinated + adequate Anti-HBs → No PEP needed
- If unvaccinated/unknown status:
- Source HBsAg (+) → HBIG + vaccination
- Source unknown → Vaccination only
| للامتحان – Exam pearls | |
|
• HBV = DNA virus (only hepatitis virus that's DNA) |
مهم |
Hepatitis C
Definition
- Acute HCV infection: Infection lasting <6 months
- Chronic HCV infection: Persistent infection >6 months (50-80% of cases)
- Caused by hepatitis C virus (HCV), an enveloped single-stranded RNA virus
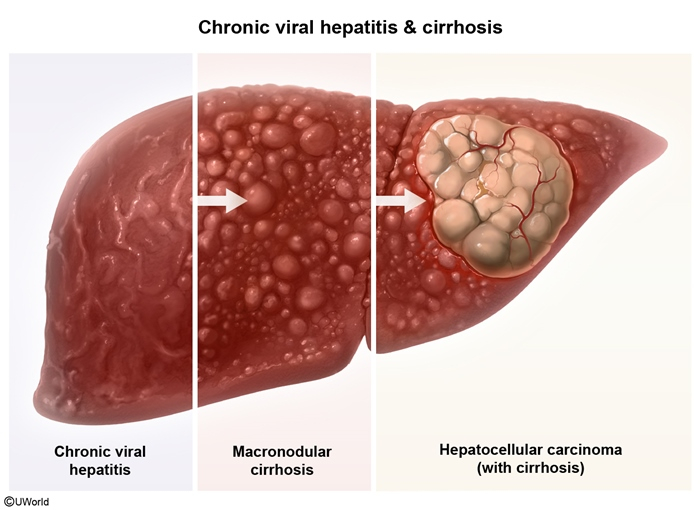
- Major cause of cirrhosis and hepatocellular carcinoma worldwide
Epidemiology
- Global burden: 58 million people with chronic HCV
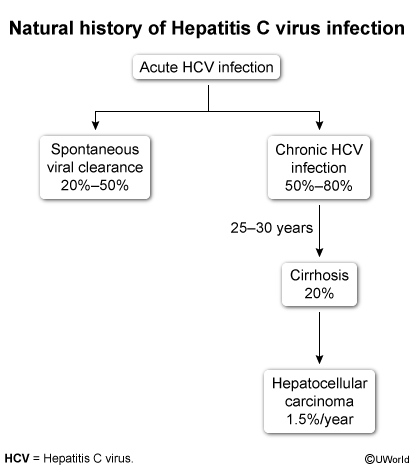
- Natural history ➜ Very important for exams
- Acute infection: 20-50% spontaneous clearance
- Chronic infection: 50-80% (much higher than HBV)
- Cirrhosis: 20% of chronic cases over 20-30 years
- HCC: 1.5% annual risk in cirrhotic patients
- 6 major genotypes with geographic variation
Transmission
- Injection drug use: Most common in developed countries
- Blood transfusions: Before 1992 screening
- Healthcare exposures: Needlesticks, unsafe medical practices
- Sexual transmission:
- Less common than HBV
- Higher risk with multiple partners, MSM, HIV coinfection
- <0.1% risk in monogamous couples
- Perinatal: 2-5% risk (lower than HBV)
- Others: Tattoos, piercings, sharing razors
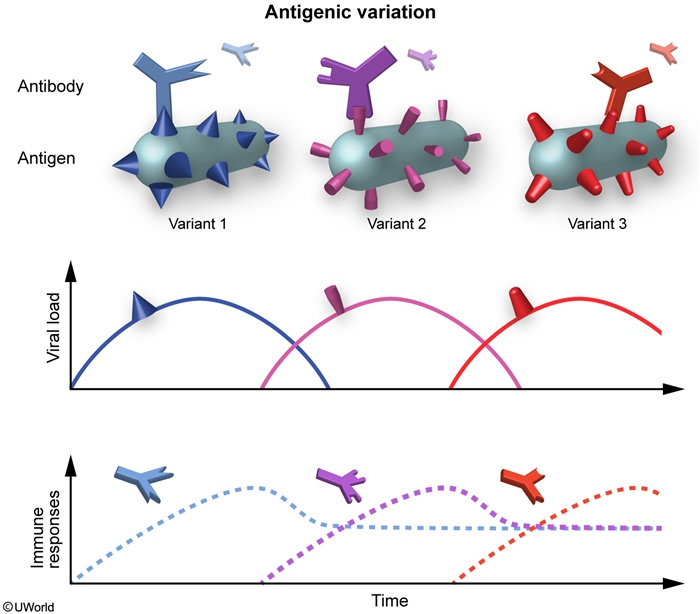
Pathophysiology
- RNA virus with high mutation rate → No proofreading enzyme
- Antigenic variation: Continuous mutations allow immune evasion
- Multiple quasispecies develop
- Prevents vaccine development
- No lifelong immunity after infection
- Chronic inflammation → Fibrosis → Cirrhosis → HCC
- Key difference from HBV: HCC only occurs with cirrhosis
Clinical Features
Acute HCV (2-26 weeks after exposure)
- 80% asymptomatic ➜ Silent infection
- When symptomatic:
- Jaundice, fatigue, malaise
- RUQ pain, nausea/vomiting
- Low-grade fever
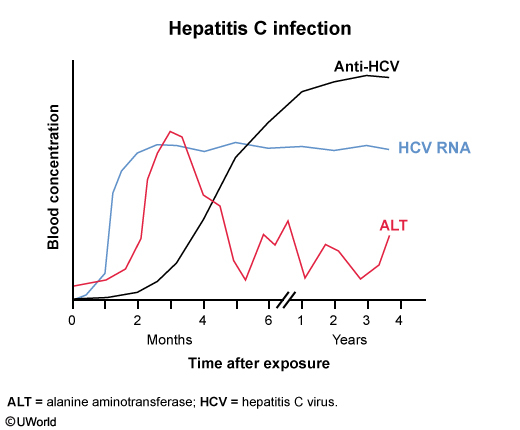
- Lab findings:
- ALT/AST ↑ (10-20× normal)
- HCV RNA detectable in days-weeks
- Anti-HCV antibodies appear in 2-6 months
Chronic HCV
- Often asymptomatic until cirrhosis
- Nonspecific symptoms: Fatigue, abdominal pain, weight loss
- Lab findings:
- ALT/AST variable (1/3 have normal ALT)
- Poor correlation between ALT and liver damage
- Persistent HCV RNA and anti-HCV
| Important – فكرة سؤال | |
|
Unlike HBV, HCV has normal ALT in 1/3 of chronic cases → ALT doesn't reflect liver damage على عكس HBV، في HCV ثلث المرضى لديهم ALT طبيعي ← ALT لا يعكس ضرر الكبد |
تذكر |
Diagnosis
Screening
- Universal screening: All adults once
- High-risk groups:
- Born 1945-1965 (baby boomers)
- IV drug users
- HIV patients
- Hemodialysis patients
Diagnostic Approach
- Step 1: Anti-HCV antibody
- Positive = Current infection, past infection, or false positive
- Negative = No infection (unless recent exposure)
- Step 2: If antibody positive → HCV RNA (PCR)
- Positive = Active infection
- Negative = Resolved infection or false positive antibody
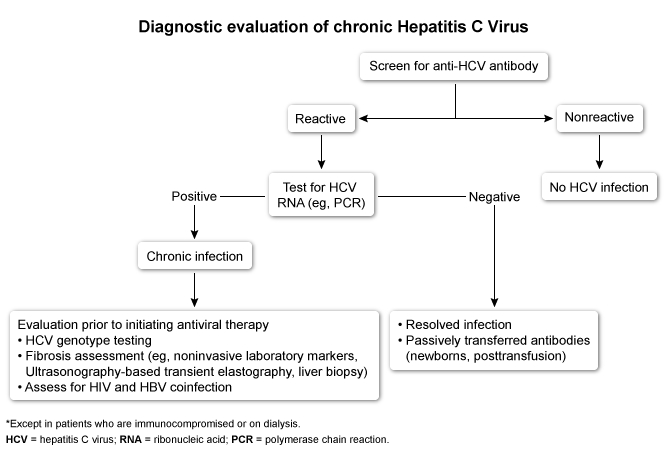
| HCV Test Interpretation | ||
| Anti-HCV | HCV RNA | Interpretation |
| Negative | Not done | No HCV infection |
| Positive | Positive | Active HCV infection |
| Positive | Negative | Resolved infection or false positive |
| Negative | Positive | Early acute infection (window period) |
Complications
Hepatic Complications
- Cirrhosis: 5-30% of chronic cases
- HCC: Only with cirrhosis (unlike HBV) ➜ مهم جداً
- 1.5% annual risk in cirrhotic patients
- Requires surveillance with ultrasound q6 months
Extrahepatic Manifestations
- Mixed cryoglobulinemia syndrome (most common)
- Palpable purpura
- Arthralgia
- Glomerulonephritis
- Peripheral neuropathy
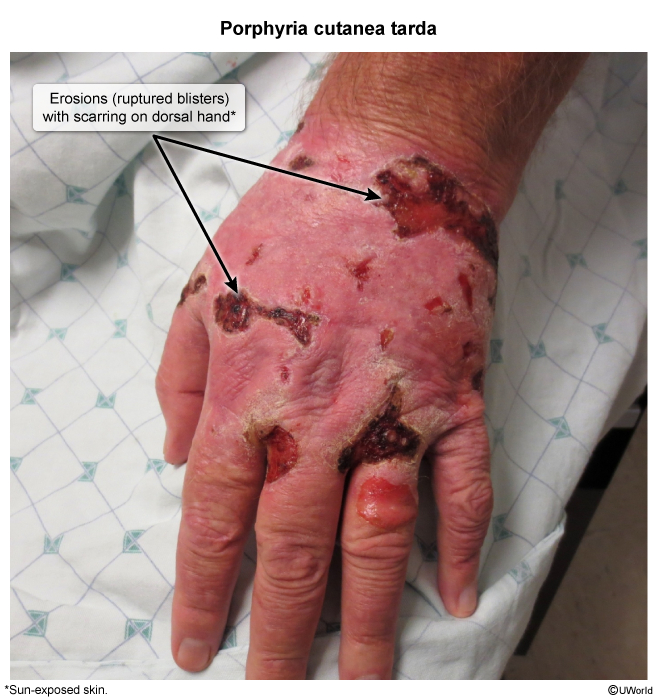
- Porphyria cutanea tarda
- Photosensitive skin lesions
- Blisters on sun-exposed areas (dorsal hands)
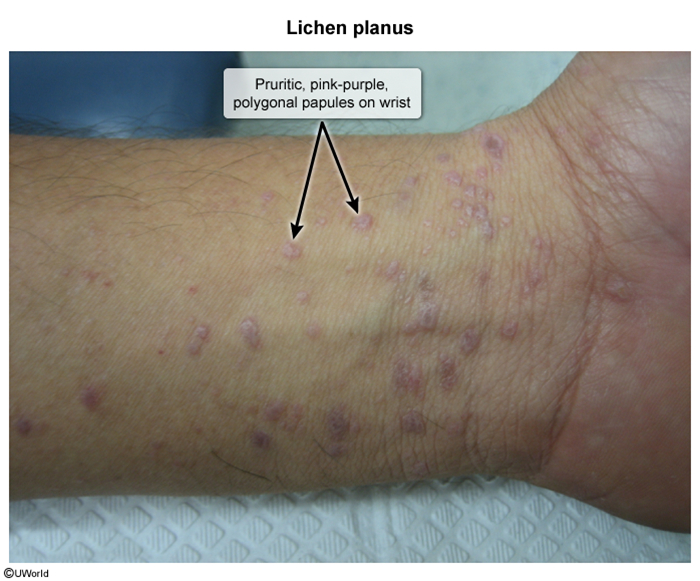
- Lichen planus: Pink-purple pruritic papules
- Membranoproliferative glomerulonephritis
- B-cell lymphoma
Treatment
Direct-Acting Antivirals (DAAs)
- Revolutionary treatment: >95% cure rate ➜ SVR (sustained virologic response)
- Duration: 8-12 weeks only
- Classes:
- NS5B polymerase inhibitors (sofosbuvir)
- NS3/4A protease inhibitors (simeprevir)
- NS5A inhibitors (ledipasvir)
- All patients should be treated regardless of fibrosis stage
- SVR = Undetectable HCV RNA 12 weeks after treatment = CURE
| Important – فكرة سؤال | |
| HCV is now CURABLE with DAAs (>95% success) while HBV is only suppressed, not cured | تذكر |
Special Considerations
- Pregnancy:
- Defer treatment until after delivery
- Vaginal delivery is safe (C-section doesn't reduce transmission)
- Breastfeeding allowed unless nipples bleeding
- Coinfections: Vaccinate against HAV and HBV
- Reinfection possible: No immunity after cure
Occupational Exposure
- Risk after needlestick: ~2%
- No PEP available (unlike HBV)
- Management:
- Baseline anti-HCV antibody
- HCV RNA at 3 weeks if high concern
- Repeat antibody at 6 months
Prevention
- NO vaccine available due to antigenic variation
- Risk reduction:
- Needle exchange programs
- Blood screening (since 1992)
- Safe injection practices
- Education about transmission risks
| HCV vs HBV - Key Differences | |
| • HCV = RNA virus, HBV = DNA virus • HCV chronicity 50-80%, HBV only 5% in adults • HCV causes HCC only with cirrhosis, HBV can cause HCC without cirrhosis • HCV is curable with DAAs, HBV is only suppressed • No vaccine for HCV, effective vaccine for HBV |
للمقارنة |
Hepatitis D
Overview
- Causative agent: HDV (Deltavirus), defective circular RNA virus
- Key feature: Requires HBV (HBsAg) for replication ➜ Cannot exist without HBV
- Prevalence: 15-20 million infected worldwide
- Geographic distribution: Mediterranean, Middle East, parts of Africa and South America
Transmission
- Parenteral route: IV drug use (most common)
- Sexual contact
- Vertical transmission (rare)
Clinical Patterns
- Coinfection: HBV + HDV acquired simultaneously
- More severe acute hepatitis
- Usually self-limited
- Low chronicity rate
- Superinfection: HDV infects chronic HBV carrier
- More aggressive disease course
- Rapid progression to cirrhosis
- High chronicity rate (~90%)
Diagnosis
- Anti-HDV IgM and IgG antibodies
- HDV RNA (confirms active replication)
- HBsAg positive (required)
Treatment
- Limited options:
- Interferon-alpha (high doses, extended duration)
- HBV antivirals have limited effect on HDV
- Liver transplantation for end-stage disease
Prevention
- HBV vaccination (prevents HDV by preventing HBV)
- No specific HDV vaccine
Hepatitis E
Epidemiology and Transmission
- Causative agent: HEV (Hepeviridae family), nonenveloped single-stranded RNA virus
- Endemic areas: Asia, Africa, Mexico
- Transmission:
- Fecal-oral route (contaminated water)
- Undercooked meat (especially pork)
Clinical Features
- Similar to HAV: self-limited acute hepatitis
- Incubation: 2-8 weeks (average 6 weeks)
- Most infections asymptomatic
- Key difference from HAV: Severe disease in pregnancy
| Important – فكرة سؤال | |
|
HEV in pregnancy (especially 3rd trimester) → Fulminant hepatitis with mortality up to 25% التهاب الكبد E في الحمل (خاصة الثلث الثالث) ← التهاب كبد خاطف مع معدل وفيات يصل إلى 25% |
تذكر |
Diagnosis
- Anti-HEV IgM: Acute infection
- Anti-HEV IgG: Past infection
- HEV RNA: For immunocompromised patients
Complications
- Fulminant hepatitis: Pregnant women (3rd trimester)
- Chronic infection: Immunosuppressed patients only
- Neurological complications (rare): Guillain-Barré syndrome
Treatment and Prevention
- Treatment: Supportive care
- Ribavirin for chronic infection (contraindicated in pregnancy)
- Prevention:
- Improved sanitation
- Vaccine available only in China
- No post-exposure prophylaxis
Viral Hepatitis Comparison
| Hepatitis A–E Comparison Table | |||||
|---|---|---|---|---|---|
| Feature | HAV | HBV | HCV | HDV | HEV |
| Virus type | RNA | DNA | RNA | RNA (defective) | RNA |
| Transmission | Fecal-oral | Blood, sexual, vertical | Blood | Blood (needs HBV) | Fecal-oral |
| Incubation | 2–6 weeks | 1–4 months | 2–26 weeks | Similar to HBV | 2–8 weeks |
| Chronicity | Never | 5% adults 90% neonates |
50–80% | ~90% (superinfection) | Rare (immunosuppressed) |
| Fulminant risk | <1% | <1% | Rare | High | High in pregnancy |
| HCC risk | No | Yes (±cirrhosis) | Yes (with cirrhosis) | Yes | No |
| Vaccine | Available | Available | None | HBV vaccine | China only |
| Treatment | Supportive | Antivirals | DAAs (cure >95%) | IFN-α | Supportive |
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.