Summary
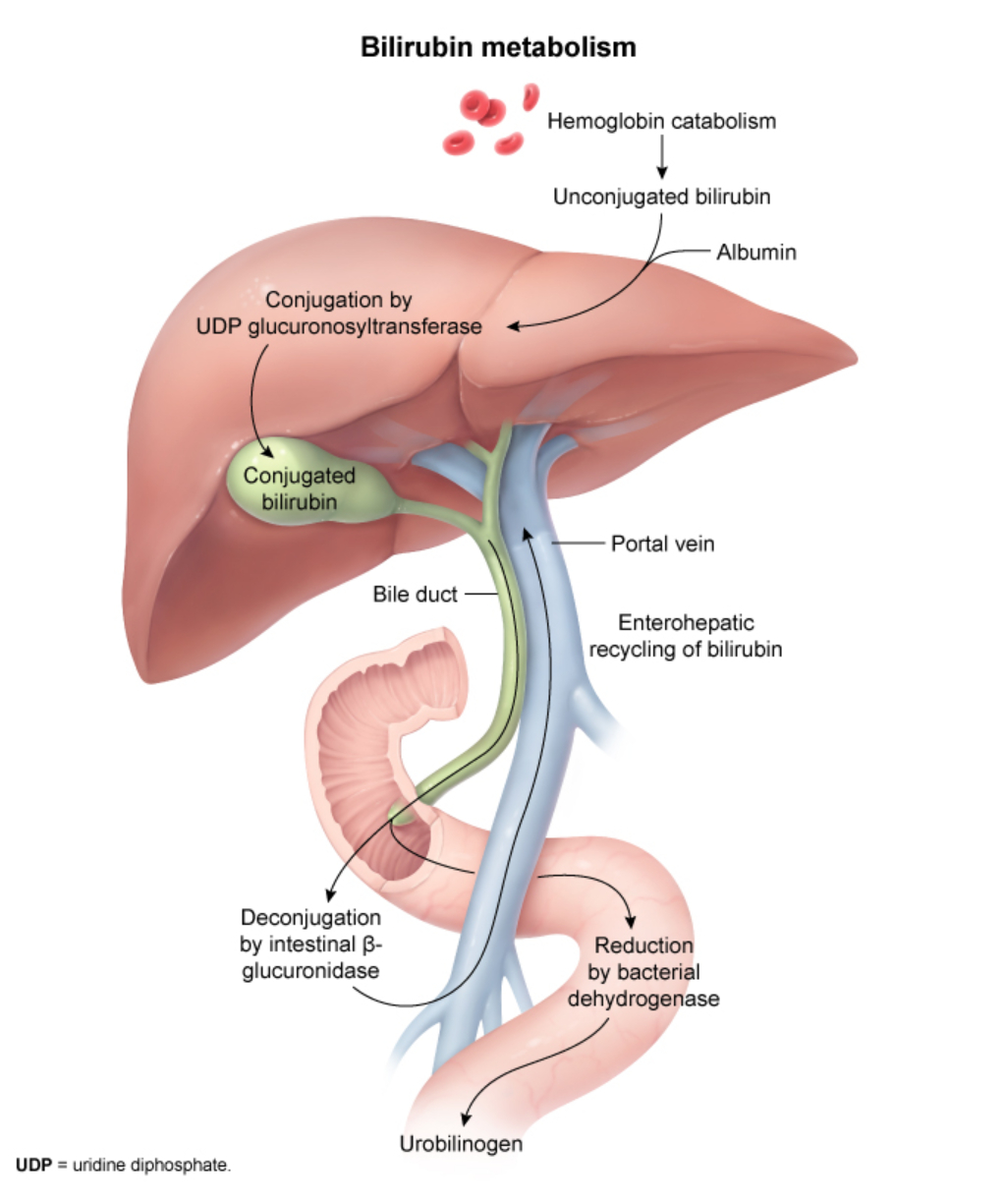
Bilirubin is a yellow pigment produced from the breakdown of heme-containing proteins, primarily hemoglobin from senescent red blood cells. Although it serves as an antioxidant at physiologic levels, excess bilirubin can be toxic and leads to jaundice (yellow discoloration of skin and sclerae). Bilirubin metabolism involves three main steps: production (from heme breakdown), conjugation (in the liver), and excretion (via bile and intestines). Jaundice can be classified based on the site of pathology into prehepatic, intrahepatic, and posthepatic causes. Hyperbilirubinemia can also be classified as unconjugated (indirect) or conjugated (direct), each with distinct causes and clinical implications. Understanding bilirubin metabolism is crucial for diagnosing and managing various hepatobiliary disorders, from benign conditions like Gilbert syndrome to serious pathologies like biliary obstruction or hepatitis.
Overview
- Bilirubin is the end product of heme catabolism, primarily from hemoglobin breakdown
- Normal total serum bilirubin: < 1 mg/dL (17 μmol/L)
- Jaundice becomes clinically visible when bilirubin > 2-3 mg/dL
- Two forms of bilirubin:
- Unconjugated (indirect) bilirubin: Lipophilic, bound to albumin, cannot be excreted in urine
- Conjugated (direct) bilirubin: Water-soluble, can be excreted in urine
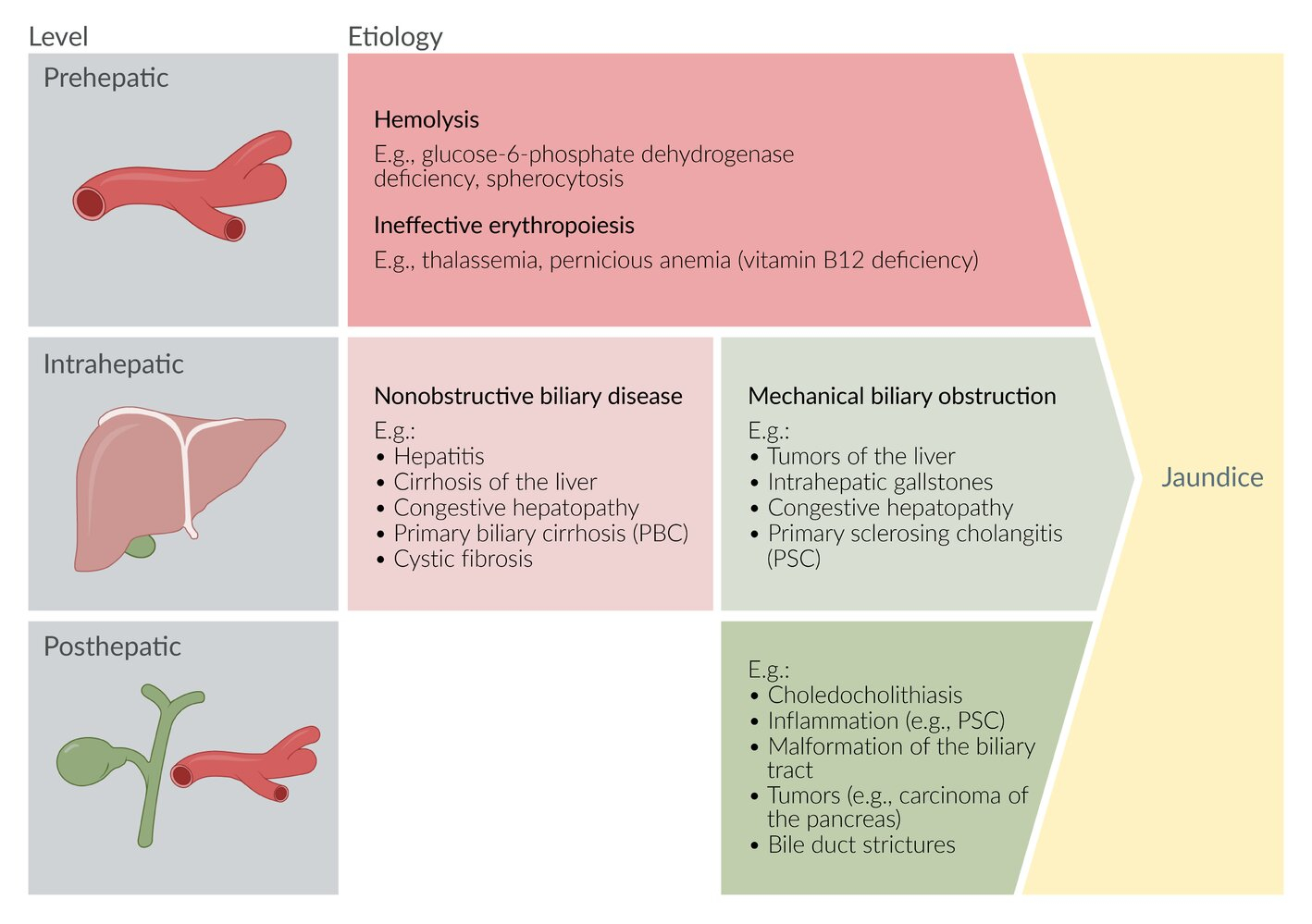
- Classification of jaundice by site of pathology:
- Prehepatic: Before the liver
- Intrahepatic: Within the liver
- Posthepatic: After the liver
Bilirubin Metabolism
1. Bilirubin Production
- Source:
- 80% from hemoglobin of senescent RBCs
- 20% from other heme-containing proteins (myoglobin, cytochromes)
- Process:
- RBCs are phagocytosed by macrophages in the reticuloendothelial system (spleen, liver, bone marrow)
- Heme → Biliverdin (green) by heme oxygenase
- Biliverdin → Unconjugated bilirubin (yellow) by biliverdin reductase
- Transport: Unconjugated bilirubin binds to albumin for transport to liver (water-insoluble)
| Important – فكرة سؤال | |
| Unconjugated bilirubin is lipophilic and cannot be filtered by the kidneys, so it does NOT appear in urine even when elevated. Only conjugated bilirubin can appear in urine. البيليروبين غير المقترن محب للدهون ولا يمكن ترشيحه بواسطة الكلى، لذلك لا يظهر في البول
|
تذكر |
2. Hepatic Uptake and Conjugation
- Uptake: Bilirubin is taken up by hepatocytes via specific transporters
- Conjugation:
- Enzyme: UDP-glucuronosyltransferase (UGT1A1)
- Process: Unconjugated bilirubin + glucuronic acid → Conjugated bilirubin
- Result: Water-soluble bilirubin that can be excreted
- Location: Smooth endoplasmic reticulum of hepatocytes
3. Excretion
- Biliary excretion:
- Conjugated bilirubin is actively transported into bile canaliculi
- Stored in gallbladder and released into small intestine
- Intestinal metabolism:
- Intestinal bacteria convert conjugated bilirubin → urobilinogen
- Fate of urobilinogen:
- 80% → further oxidized to stercobilin (brown color of stool)
- 20% reabsorbed (enterohepatic circulation):
- Most returns to liver
- Small amount → kidneys → urobilin (yellow color of urine)
Classification of Jaundice
Prehepatic Jaundice
Definition: Jaundice caused by excessive bilirubin production before it reaches the liver
Mechanism: Increased hemoglobin breakdown → overwhelms liver's conjugation capacity
Type of hyperbilirubinemia: Unconjugated (indirect)
Causes:
- Hemolysis
- G6PD deficiency
- Sickle cell anemia
- Hereditary spherocytosis
- Autoimmune hemolytic anemia
- Hemolytic transfusion reaction
- Ineffective erythropoiesis
- Thalassemia
- Pernicious anemia
- Sideroblastic anemia
- Increased bilirubin production
- Massive blood transfusions
- Large hematoma resorption
- Medication side effects
- Rifampin, probenecid (impaired hepatic uptake)
- Ribavirin
- Protease inhibitors (atazanavir, indinavir)
Intrahepatic Jaundice
Definition: Jaundice due to liver dysfunction
Mechanism: Impaired bilirubin conjugation, hepatocellular injury, or intrahepatic cholestasis
Type of hyperbilirubinemia: Can be unconjugated, conjugated, or mixed
Causes:
- Impaired bilirubin conjugation (unconjugated)
- Gilbert syndrome
- Crigler-Najjar syndrome
- Hepatocellular injury (mixed)
- Viral hepatitis (A-E, EBV, CMV)
- Alcoholic hepatitis
- Drug-induced hepatitis (acetaminophen, statins)
- Cirrhosis
- MASH (metabolic dysfunction-associated steatohepatitis)
- Wilson disease
- Autoimmune hepatitis
- Impaired hepatic excretion (conjugated)
- Dubin-Johnson syndrome
- Rotor syndrome
- Intrahepatic cholestasis (conjugated)
- Primary biliary cholangitis
- Primary sclerosing cholangitis
- Intrahepatic cholestasis of pregnancy
- Drugs (oral contraceptives, anabolic steroids)
- Sepsis
- Total parenteral nutrition
Posthepatic Jaundice
Definition: Jaundice due to obstruction of bile flow after it leaves the liver
Mechanism: Biliary obstruction → backflow of conjugated bilirubin into blood
Type of hyperbilirubinemia: Conjugated (direct)
Causes:
- Malignancy
- Pancreatic head cancer
- Cholangiocarcinoma
- Ampullary cancer
- Gallbladder cancer
- Hepatocellular carcinoma
- Metastases to porta hepatis
- Gallstone disease
- Choledocholithiasis (most common benign cause)
- Cholangitis
- Mirizzi syndrome
- Biliary strictures
- Post-surgical
- Chronic pancreatitis
- Primary sclerosing cholangitis
- Infections
- AIDS cholangiopathy
- Liver flukes
- Ascariasis
| Note | |
| Remember the mnemonic "HOT Liver" for common causes of jaundice: Hemolysis, Obstruction, Tumor, Liver disease | ملاحظة |
| Note | |
| In conjugated hyperbilirubinemia, look for dark urine (due to bilirubinuria) and pale stools (due to decreased stercobilin). These findings suggest biliary obstruction. | ملاحظة |
Clinical Features
General Features of Jaundice
- Jaundice (icterus): Yellow discoloration of skin and sclerae
- Visible when bilirubin > 2-3 mg/dL
- Best seen in natural light
- First appears in sclerae and under tongue
- Pruritus: Due to bile salt deposition in skin (mainly in cholestatic jaundice)
Features by Type of Jaundice
| Clinical Features by Jaundice Type | |||
|---|---|---|---|
| Feature | Prehepatic | Intrahepatic | Posthepatic |
| Urine color | Normal (no bilirubinuria) | Dark (if conjugated) | Very dark (tea-colored) |
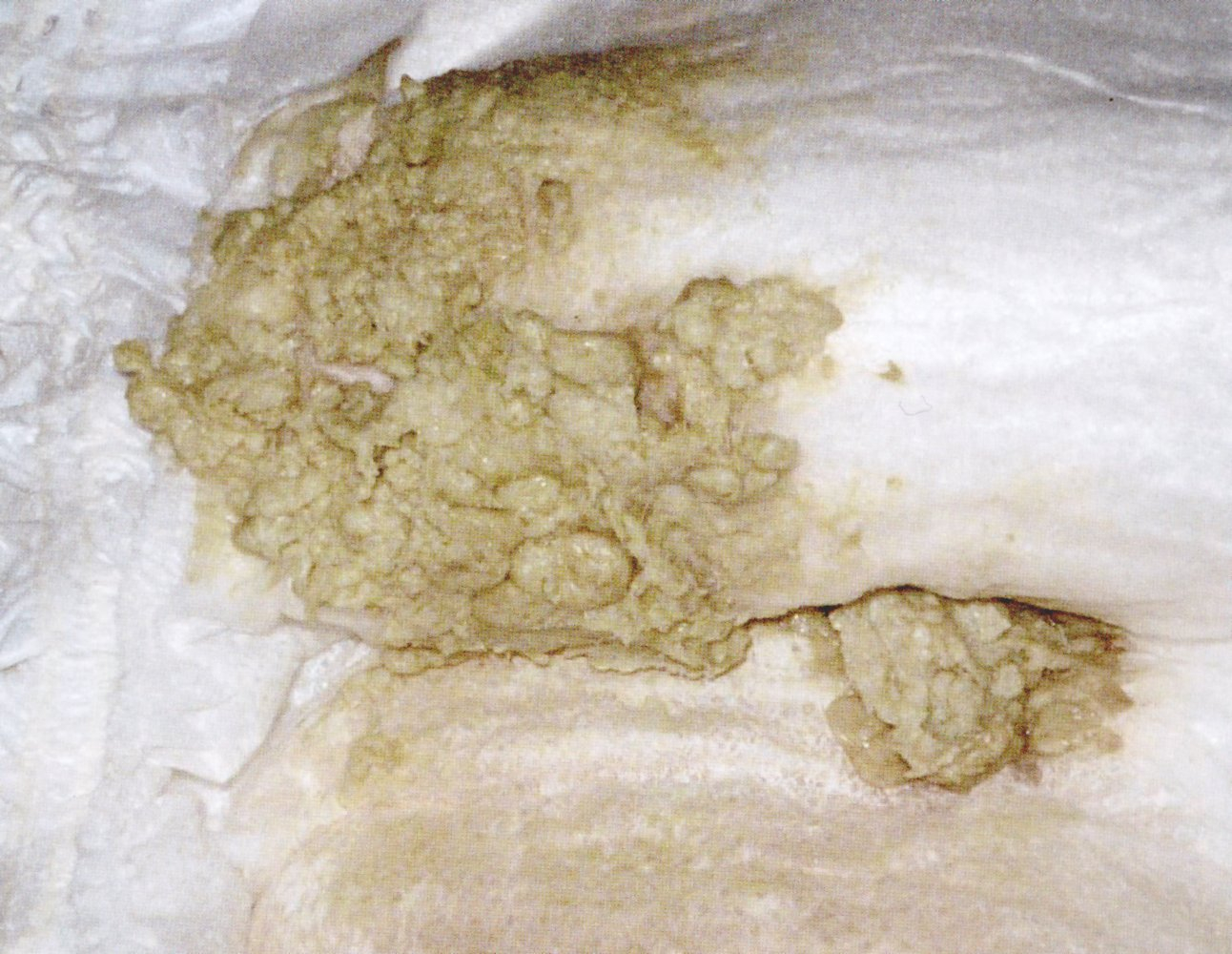
| Stool color | Normal or dark | Variable | Pale / clay-colored |
| Pruritus | Absent | Variable | Present |
| Associated symptoms |
|
|
|
| Important – فكرة سؤال | |
|
Painless jaundice + palpable gallbladder (Courvoisier sign) = Think pancreatic head cancer يرقان غير مؤلم + مرارة محسوسة = فكر في سرطان رأس البنكرياس |
تذكر |



Diagnosis
Initial Workup
- History:
- Onset and duration of jaundice
- Associated symptoms (pain, fever, weight loss)
- Alcohol use, medications, travel history
- Family history of liver disease
- Physical examination:
- Degree and distribution of jaundice
- Signs of chronic liver disease
- Abdominal examination (hepatomegaly, splenomegaly, masses)
Laboratory Tests
- Step 1: Fractionated bilirubin
- Total bilirubin
- Direct (conjugated) bilirubin
- Indirect (unconjugated) = Total - Direct
- Step 2: Based on predominant type
- If unconjugated predominant:
- Complete blood count (CBC) with smear
- Reticulocyte count
- Haptoglobin, LDH
- Direct Coombs test
- If conjugated predominant:
- AST, ALT (hepatocellular pattern if elevated)
- Alkaline phosphatase, GGT (cholestatic pattern if elevated)
- PT/INR, albumin (synthetic function)
- Viral hepatitis serologies
- If unconjugated predominant:
- Urine tests:
- Urinalysis for bilirubin and urobilinogen
- Bilirubinuria = conjugated hyperbilirubinemia
- Absent urobilinogen = complete biliary obstruction
| Laboratory Findings by Jaundice Type | |||
| Test | Prehepatic | Intrahepatic | Posthepatic |
| Indirect bilirubin | ↑↑ | ↑ | Normal |
| Direct bilirubin | Normal | ↑ | ↑↑ |
| AST/ALT | Normal | ↑↑ | Normal or mildly ↑ |
| ALP/GGT | Normal | Normal or ↑ | ↑↑↑ |
| Urine bilirubin | Absent | Present | Present |
| Urine urobilinogen | ↑↑ | Normal or ↑ | ↓ or absent |
Imaging Studies
- Ultrasound (first-line for suspected obstruction):
- Dilated bile ducts suggest obstruction
- Can detect gallstones, masses
- CT scan: Better for pancreatic pathology
- MRCP: Non-invasive visualization of biliary tree
- ERCP: Diagnostic and therapeutic for biliary obstruction
Differential Diagnosis
| Common Causes of Jaundice by Age Group | |||
|---|---|---|---|
| Age Group | Unconjugated | Conjugated (Hepatocellular) | Conjugated (Obstructive) |
| Neonates |
|
|
|
| Young Adults |
|
|
|
| Older Adults |
|
|
|
Treatment
General Principles
- Treat the underlying cause معالجة السبب الأساسي
- Supportive care for symptoms
- Monitor for complications
Treatment by Jaundice Type
- Prehepatic Jaundice
- Hemolysis:
- Treat underlying cause
- Folic acid supplementation
- Blood transfusion if severe anemia
- Avoid triggers (in G6PD deficiency)
- Drug-induced:
- Discontinue offending medication
- Hemolysis:
- Intrahepatic Jaundice
- Gilbert syndrome:
- Reassurance (benign condition)
- Avoid fasting and dehydration
- Crigler-Najjar syndrome:
- Type I: Phototherapy, liver transplantation
- Type II: Phenobarbital (induces UGT)
- Hepatocellular injury:
- Remove offending agents (alcohol, drugs)
- Antiviral therapy for hepatitis
- Corticosteroids for autoimmune hepatitis
- N-acetylcysteine for acetaminophen toxicity
- Liver transplant for fulminant hepatic failure
- Gilbert syndrome:
- Posthepatic Jaundice
- Biliary obstruction:
- ERCP with sphincterotomy for choledocholithiasis
- Biliary stenting for malignant obstruction
- Surgery for resectable tumors
- Cholecystectomy after acute cholangitis resolves
- Biliary obstruction:
Symptomatic Treatment
- Pruritus:
- Cholestyramine (bile acid sequestrant)
- Ursodeoxycholic acid
- Antihistamines (limited efficacy)
- Rifampin for refractory cases
- Fat-soluble vitamin supplementation (A, D, E, K) in chronic cholestasis
Summary Table
| Comparison of Jaundice Types | |||
|---|---|---|---|
| Prehepatic | Intrahepatic | Posthepatic | |
| Main mechanism | ↑ Bilirubin production | Liver dysfunction | Biliary obstruction |
| Bilirubin type | Unconjugated | Mixed | Conjugated |
| Common causes |
|
|
|
| Lab pattern |
|
|
|
| Clinical clues | Normal urine color | Variable presentation | Dark urine + pale stools |
| ALP = alkaline phosphatase; ALT = alanine aminotransferase; AST = aspartate aminotransferase; GGT = gamma-glutamyl transferase; LDH = lactate dehydrogenase | |||
احصل على التجربة الكاملة
اشترك للوصول لفيديوهات الشرح التفصيلي والبطاقات التعليمية التفاعلية وأسئلة الممارسة مع تتبع التقدم.