YourMedPass
أكبر مرجع لامتحان الامتياز الأردني وامتحانات الإقامة
Chronic Pancreatitis
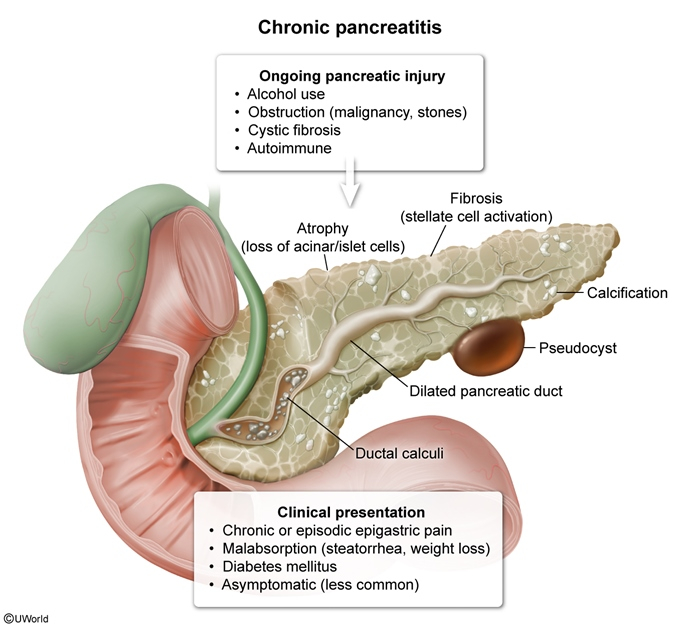
Chronic pancreatitis is a progressive inflammatory disorder characterized by irreversible structural damage to the pancreas, leading to both exocrine and endocrine insufficiency. Chronic alcohol abuse is the most common cause, followed by idiopathic cases. Patients typically present with recurrent epigastric pain, steatorrhea, and weight loss. Diagnosis is confirmed by imaging showing pancreatic calcifications, ductal changes, or atrophy. Management focuses on alcohol cessation, pain control, pancreatic enzyme replacement, and managing complications including diabetes.
Last updated: July 29, 2025
- Progressive inflammation of the pancreas resulting in irreversible structural damage and functional impairment
- Characterized by fibrosis, loss of acinar and islet cells, and ductal abnormalities
- Results in both exocrine insufficiency (maldigestion) and endocrine insufficiency (diabetes)
- Incidence: 5-12 per 100,000 people annually
- More common in men (especially alcohol-related cases)
- Peak age: 40-50 years for alcohol-related; earlier for hereditary forms
- Less than 5% of heavy drinkers develop chronic pancreatitis
Remember TIGAR-O:
- Toxic-metabolic: Alcohol (most common cause, 40-70%), smoking, hypercalcemia, chronic renal failure
- Idiopathic: 20-30% of cases
- Genetic: PRSS1, CFTR, SPINK1 mutations
- Autoimmune: Type 1 (IgG4-related) and Type 2
- Recurrent acute pancreatitis
- Obstructive: Pancreas divisum, tumors, strictures
High-Yield Point: In young adults with chronic pancreatitis, always consider cystic fibrosis (CFTR mutations) especially if there's recurrent pneumonia, sinusitis, or infertility.
- Alcohol → oxidative stress → stellate cell activation → fibrosis
- Progressive destruction of pancreatic parenchyma
- Loss of acinar cells → exocrine insufficiency (occurs after 90% destruction)
- Loss of islet cells → endocrine insufficiency (diabetes)
- Ductal obstruction and calcification
| Clinical Manifestations of Chronic Pancreatitis | |
| Pain |
|
| Exocrine Insufficiency |
|
| Endocrine Insufficiency |
|
Exam Tip: In later stages, patients may have NO pain ("painless pancreatitis") but still have malabsorption and diabetes.

Laboratory Tests
- Amylase/Lipase: Usually NORMAL (unlike acute pancreatitis)
- Pancreatic function tests:
- Fecal elastase-1 < 200 mcg/g (most practical test)
- 72-hour fecal fat > 7g/day (confirms steatorrhea)
- Serum trypsinogen < 20 ng/mL
- Glucose: Check fasting glucose/HbA1c annually
Imaging
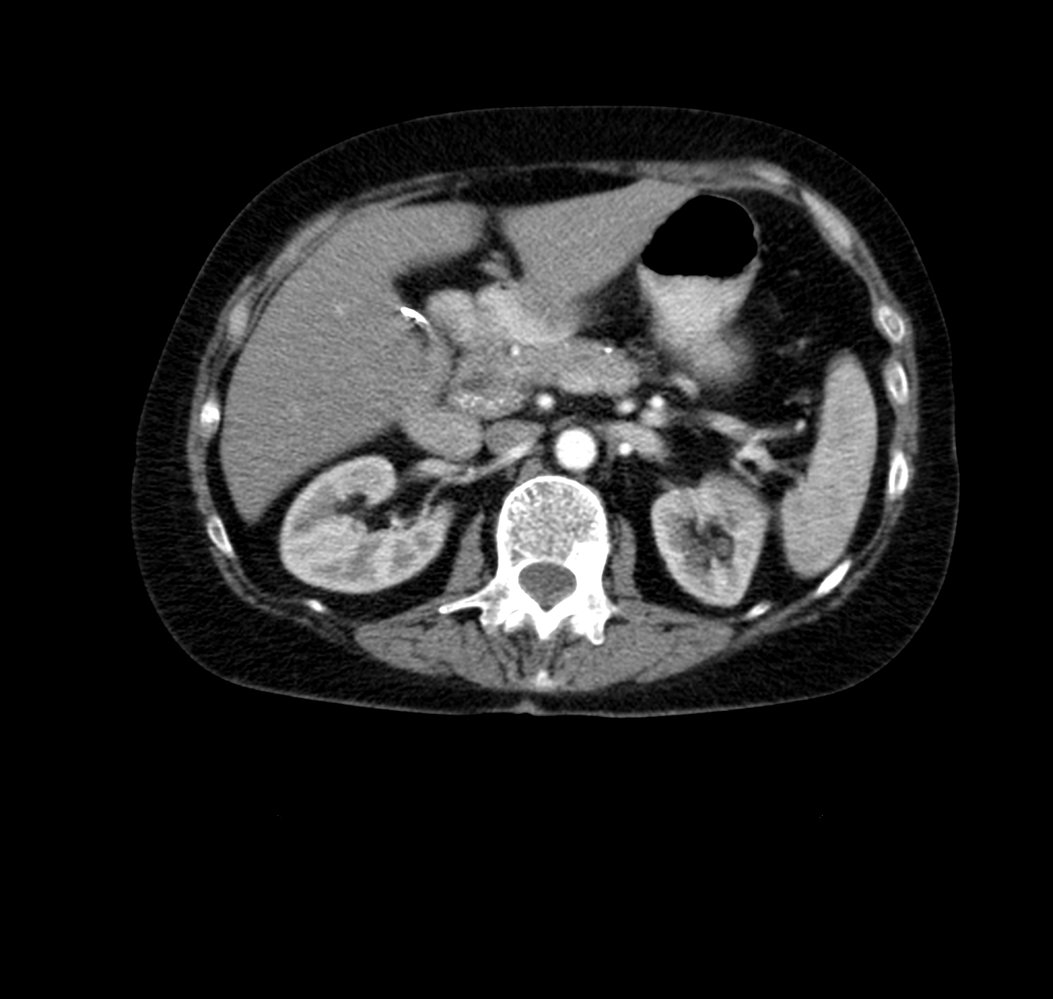
- CT abdomen (best initial test):
- Pancreatic calcifications (pathognomonic)
- Pancreatic atrophy
- Ductal dilation
- MRCP: If CT is non-diagnostic
- "Chain of lakes" appearance
- Ductal strictures and dilations
- Plain abdominal X-ray: May show calcifications (30% sensitivity)
Remember: Pancreatic calcifications on imaging = Chronic pancreatitis until proven otherwise
Conservative Management
- Alcohol and smoking cessation (most important)
- Diet: Small, frequent, low-fat meals
- Pancreatic enzyme replacement:
- Given with meals
- Add PPI to prevent enzyme degradation
- Fat-soluble vitamins (A, D, E, K)
- Diabetes management: Insulin (oral agents usually ineffective)
Pain Management
- First-line: NSAIDs, acetaminophen
- Second-line: Tramadol, TCAs (amitriptyline), gabapentin/pregabalin
- Avoid opioids (high addiction risk)
- Interventional:
- Celiac plexus block
- ERCP with sphincterotomy
- Surgery (last resort)
- Pancreatic pseudocyst (most common)
- Splenic vein thrombosis → gastric varices
- Bile duct obstruction → jaundice
- Pancreatic ascites/pleural effusion
- Pancreatic adenocarcinoma (especially hereditary pancreatitis)
- Most common cause = Alcohol
- Pathognomonic finding = Pancreatic calcifications
- Best initial imaging = CT abdomen
- Triad: Calcifications + Steatorrhea + Diabetes
- Pain may disappear in advanced disease
- Amylase/Lipase are usually NORMAL
- Treatment: Enzymes + No alcohol + Pain control (no opioids)