YourMedPass
أكبر مرجع لامتحان الامتياز الأردني وامتحانات الإقامة
Irritable bowel syndrome (IBS)
Irritable bowel syndrome (IBS) is a common functional gastrointestinal disorder characterized by chronic abdominal pain associated with altered bowel habits. It affects approximately 10-15% of the population, with higher prevalence in women. The diagnosis is based on clinical criteria (Rome IV) and exclusion of organic disease. Management focuses on symptom control through lifestyle modifications and targeted pharmacotherapy.
Last updated: July 31, 2025
- IBS is a functional disorder - no structural or biochemical abnormalities detectable by conventional tests
- Characterized by recurrent abdominal pain + altered bowel habits (diarrhea, constipation, or both)
- Peak onset: late teens to early 20s
- Female predominance (14% vs 9% in males)
- 50% of patients have comorbid psychiatric conditions (anxiety, depression)
- Does NOT increase risk of colorectal cancer or IBD
The exact mechanism is unclear, but multiple factors contribute:
- Visceral hypersensitivity: Heightened pain perception to normal gut stimuli
- Altered gut motility: Abnormal intestinal contractions
- Gut-brain axis dysfunction: Abnormal communication between CNS and enteric nervous system
- Post-infectious changes: Can develop after acute gastroenteritis
- Microbiome alterations: Changes in gut bacterial composition
- Psychosocial factors: Stress and emotional factors influence symptom expression
Core Symptoms:
- Abdominal pain/discomfort
- Crampy, diffuse
- Related to defecation (improves or worsens)
- Often triggered by meals or stress
- Altered bowel habits
- Change in stool frequency
- Change in stool form/consistency
- May have mucus in stools
- Additional symptoms: Bloating, abdominal distension, urgency, incomplete evacuation
| Note | |
| IBS symptoms are typically relieved by defecation and worsened by stress. The absence of nocturnal symptoms is an important distinguishing feature from organic disease. | ملاحظة |
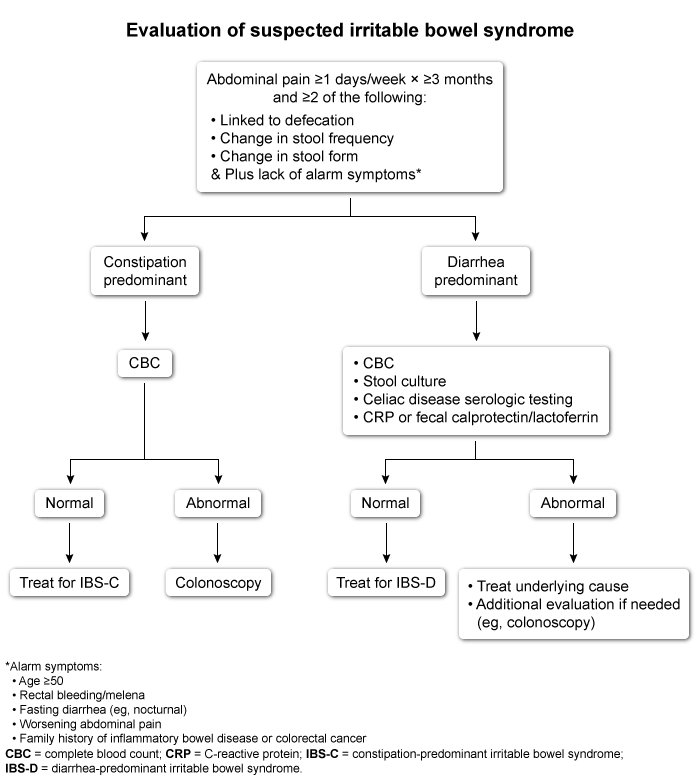
Rome IV Criteria:
Recurrent abdominal pain ≥1 day/week for the past 3 months, associated with ≥2 of the following:
- Related to defecation
- Change in stool frequency
- Change in stool form (appearance)
IBS Subtypes:
- IBS-D (Diarrhea-predominant): >25% loose stools, <25% hard stools
- IBS-C (Constipation-predominant): >25% hard stools, <25% loose stools
- IBS-M (Mixed): >25% loose AND >25% hard stools
Alarm Features (Red Flags):
Presence suggests organic disease - require further investigation:
- Age of onset ≥50 years
- Unintentional weight loss
- Nocturnal or progressive symptoms
- Blood in stools
- Iron deficiency anemia
- Family history of colorectal cancer or IBD
- Elevated inflammatory markers (CRP, calprotectin)
See () for diagnostic criteria and alarm features.
Diagnostic Approach:
- IBS-C: CBC to exclude anemia
- IBS-D: CBC, celiac serology, inflammatory markers (CRP, fecal calprotectin), stool studies
- Colonoscopy: Only if alarm features present or age >50
| Important – فكرة سؤال | |
| IBS can be diagnosed based on clinical criteria without extensive testing if no alarm features are present. Avoid unnecessary investigations in young patients with typical symptoms. | تذكر |
- Inflammatory bowel disease: Bloody diarrhea, elevated inflammatory markers, abnormal colonoscopy
- Celiac disease: Positive serologies, malabsorption symptoms
- Colorectal cancer: Age >50, bleeding, weight loss, anemia
- Medication side effects: Metformin (diarrhea), opioids (constipation)
- Functional dyspepsia: Upper GI symptoms without bowel habit changes
- Ovarian cancer: Older women, bloating, early satiety, weight loss
General Approach:
- Lifestyle modifications (all patients):
- Regular meals, adequate sleep
- Exercise
- Stress management
- Dietary changes:
- Avoid trigger foods (alcohol, caffeine, gas-producing foods)
- Consider low FODMAP diet
- Increase soluble fiber (psyllium)
Pharmacotherapy:
Treatment is symptom-targeted - see ()
For Abdominal Pain:
- First-line: Antispasmodics (hyoscyamine, dicyclomine) - as needed
- Second-line: Tricyclic antidepressants (amitriptyline, nortriptyline)
- Low doses for analgesic effect
- Good for IBS-D (anticholinergic effects slow transit)
- Avoid in IBS-C
For IBS-D (Diarrhea):
- First-line:
- Soluble fiber (psyllium)
- Loperamide (as needed)
- Second-line:
- Bile acid sequestrants (cholestyramine)
- 5-HT3 antagonists (alosetron) - restricted use
For IBS-C (Constipation):
- First-line:
- Soluble fiber (psyllium)
- Osmotic laxatives (polyethylene glycol)
- Second-line:
- Lubiprostone
- Linaclotide (guanylate cyclase agonist)
| Important – فكرة سؤال | |
|
Remember: Tricyclic antidepressants are preferred for IBS-D but should be avoided in IBS-C due to anticholinergic effects causing constipation. تذكر: مضادات الاكتئاب ثلاثية الحلقات مفضلة في IBS-D ولكن يجب تجنبها في IBS-C بسبب التأثيرات المضادة للكولين التي تسبب الإمساك |
تذكر |
- Chronic condition with fluctuating symptoms
- 80% of patients improve over time
- Does NOT increase risk of:
- Colorectal cancer
- Inflammatory bowel disease
- Other organic GI diseases
- Main impact is on quality of life
- Young patient + chronic abdominal pain + altered bowel habits + relief with defecation = IBS
- Nocturnal symptoms suggest organic disease, NOT IBS
- Diagnosis is clinical - avoid unnecessary tests without red flags
- Treatment is symptom-based, not curative
- Strong association with psychiatric comorbidities
- More common in women and young adults