YourMedPass
أكبر مرجع لامتحان الامتياز الأردني وامتحانات الإقامة
Gastroesophageal reflux disease (GERD)
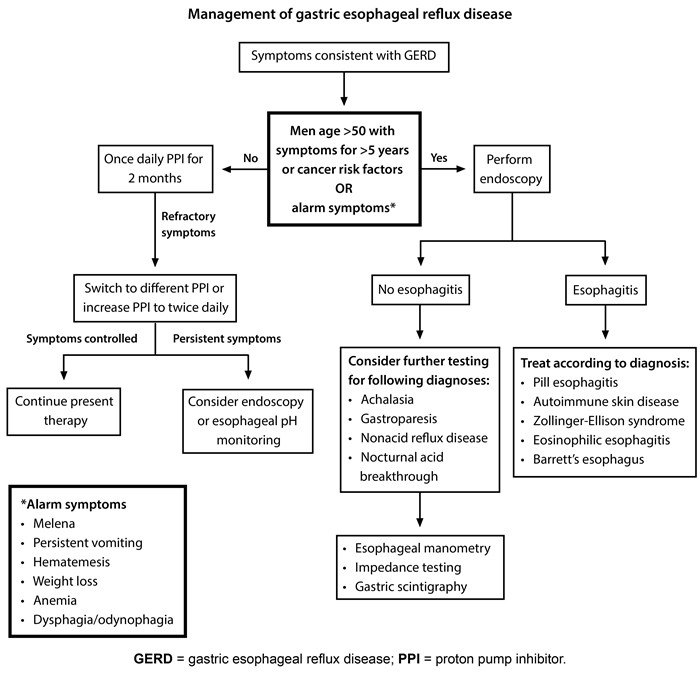
GERD is a common but complex condition that involves multiple factors from transient LES relaxations to specific anatomical anomalies. A careful approach to diagnosis, including recognition of red flags and utilization of EGD or esophageal pH monitoring, can guide an appropriate therapeutic strategy. Management commonly involves lifestyle changes and medications like PPIs, with surgery reserved for specific cases. Chronic mucosal damage in GERD must be treated to prevent the progression to Barrett’s esophagus and potential adenocarcinoma.
Last updated: July 16, 2025
GERD is a chronic disorder where stomach contents flow back into the esophagus, irritating the mucosa. It can be classified into:
- NERD (Non-erosive Reflux Disease): Characteristic symptoms without evidence of injury (50-70% of GERD patients).
- ERD (Erosive Reflux Disease): With evidence of esophageal injury (30-50% of GERD patients).

GERD develops due to factors like:
- Gastroesophageal Junction Dysfunction:
- Increased transient lower esophageal sphincter relaxations (TLESRs) ➜ Most common cause
- An imbalance between intragastric and LES pressures,
- Anatomical abnormalities (e.g., hiatal hernia).
- Impaired Esophageal Acid Clearance: Reduced salivation or peristalsis.
- Smoking
- Stress
- Obesity
- Pregnancy
- Angle of His enlargement
- Iatrogenic causes
- Inadequate protective factors
- Gastrointestinal malformations and tumors
- Scleroderma
- Asthma
The histopathological findings include the following (may vary depending on the severity of mucosal damage):
- Superficial coagulative necrosis in the nonkeratinized squamous epithelium
- Thickening of the basal cell layer
- Elongation of the papillae in the lamina propria and dilation of the vascular channels at the tip of the papillae (leading to hyperemia)
- Inflammatory cells (granulocytes, lymphocytes, macrophages)
- Transformation of squamous into columnar epithelium leads to Barrett metaplasia
- Typical Symptoms:
- Heartburn (most common),
- Regurgitation,
- Dysphagia.
- Atypical Symptoms: Noncardiac chest pain, belching, bloating, dental erosion, etc.
- Red Flags: Dysphagia, anemia, unintentional weight loss, vomiting, signs of GI bleeding.
The diagnosis is based on a combination of clinical presentation, endoscopic evaluation, reflux assessment, and therapeutic response.
- Approach: Includes clinical evaluation, rule out life-threatening diagnoses, empiric PPI trial, EGD, esophageal pH monitoring.
- EGD (Esophagogastroduodenoscopy):
- Indicated in red flags, no symptomatic improvement after PPI trial.
- Not necessary for a typical GERD presentation
- 24 Esophageal pH Monitoring:
- Used to identify abnormal reflux (Best and most sensitive).
- 24-hour pH monitoring is considered the gold standard for GERD diagnosis.
- Esophageal barium swallow
- Contrast medium is swallowed and serial
- May show strictures, tumors, hiatal hernias, and severe esophagitis
- Esophageal manometry.
- To rule out esophageal motility disorders
- Lifestyle Changes: Include modifications in diet and eating habits.
- Avoid eating < 3 hours before bedtime.
- Weight loss (if obese)
- Elevate the head of the bed (if with nocturnal symptoms).
- Avoid triggers (e.g., alcohol, coffee , spices).
- Smoking cessation
- Pharmacological Therapy:
- PPIs (Proton Pump Inhibitors): Standard treatment for 8 weeks.
- Once-daily therapy, 30–60 minutes before a meal
- Most effective therapy
- Most common maintenance therapy
- Heal esophagitis, if present
- Examples: omeprazole, pantoprazole
- H2 receptor antagonists:
- Consider as alternate maintenance therapy for NERD, or in addition to PPIs to control nighttime symptoms
- Decreases acid secretion by blocking H2 receptors in gastric parietal cells
- Examples: famotidine,cimetidine
- PPIs (Proton Pump Inhibitors): Standard treatment for 8 weeks.
- Surgical Therapy (Nissen's fundoplication): Indicated in select cases with complications despite medical therapy.
- Indications:
- Discontinuation of medical therapy (e.g., due to nonadherence or side effects)
- Symptoms refractory to medical therapy
- Complications despite optimal medical therapy, e.g., severe esophagitis , strictures, recurrent aspiration
- Large hiatal hernia
- Indications:

- Reflux esophagitis: most common complication of GERD
- Erosive esophagitis
- 30% of patients with untreated GERD
- Iron deficiency anemia: mucosal erosions and ulcerations → chronic bleeding → anemia
- Esophageal stricture
- Results from healing of erosive esophagitis
- Causes dysphagia to solids/food impaction
- Esophageal rings: e.g., Schatzki rings
- Barrett esophagus
- Definition: intestinal metaplasia of the esophageal mucosa induced by chronic reflux.
- Histopathological examination of the mucosa shows a columnar epithelium instead of the normal squamous epithelium.
- Precursor to esophageal adenocarcinoma
- Diagnosed by endoscopy with biopsy
- Definition: intestinal metaplasia of the esophageal mucosa induced by chronic reflux.
- Reflux laryngitis: hoarseness (due to laryngopharyngeal reflux)
|
Gastroesophageal reflux disease |
|
|
Pathophysiology |
|
|
Manifestations |
|
|
Complications |
|
|
Initial treatment |
|
|
H2R = histamine 2 receptor; LES = lower esophageal sphincter. |
|